Joseph Casper is CEO of Sandlot Solutions of Fort Worth, TX.
Tell me about yourself and the company.
The Sandlot organization has been around for six or seven years, tied to an organization out of Dallas-Fort Worth, North Texas Specialty Physicians, building a health information exchange solution, managing patient risk, and driving connectivity among the physicians.
I became the CEO because I have 12 years of experience in building health information exchange systems. I’m the co-inventor of the first gateway solution that was initially deployed at Swedish Medical Center, two or three of the sites up in New York including Manhattan, the District of Columbia, the state of New Mexico, a couple of million people in Los Angeles, and the province of British Columbia. Needless to say, I got a fair amount of experience.
I’m somewhat of an entrepreneur. This is the fourth company that I’ve been involved in where we build technology or software that I’d either led as CEO or run as president of the company.
You have a somewhat unusual advantage of working directly with North Texas Specialty Physicians. What are the main lessons you’ve learned from that organization?
When you can come at this from the angle of physicians connecting physicians together, the majority of the health information exchanges that were originally deployed connected hospitals to hospitals. They had a flavor that looked very different then when the problem you’re trying to solve is your independent physician organization with tight hospital relationships. You deploy electronic medical records, you try to connect primary care physicians on one platform to specialty physicians on another platform where everyone is bearing risk, you quickly realize that you need to have solution in place that can connect them.
NTSP invested in Sandlot to solve that problem. As they started to solve that problem, they started to solve other problems, primarily increasing their risk business and then understanding the kind of analytics tools that’s required to do that, the sort of information you need to have at your fingertips from claims data merged together with clinical data so that you have a very rich set of data to run analytics against to look for gaps in care and to push on to physicians in a seamless way.
The company has been described as offering a fourth-generation solution. What does that mean?
Having participated in these things since 2001 when I first touched health information exchange, we were off initially just connecting hospitals. The fourth-generation health information exchange starts from the physician end. It creates the connectivity required from hospitals to physicians in a bi-directional way. If you go back to, say, the second generation, they were pushing information out, so discharge notes were being pushed out to the physicians. But you weren’t able to capture that information and ingest it back in.
The fourth-generation product first connects the physicians together in a way that the clinical dataset is not only brought into a repository — where you can run analytics against it, look for gaps in care, report so you can manage frequent flyers, look at your top admissions — but you can then bundle that Continuity of Care Document back up and push it back out into the physicians. When the patient shows up from primary care to a specialist or secondary care, that aggregated CCD is there ingesting data from the hospital visit, from national labs, and from others. This continuum moves us further up the pipeline to say it’s aggregated along the way. What was documents has been broken down now into discrete data.
Where we would immediately differentiate ourselves from many of the folks who are moving documents around, CCDs around, is that they keep that data in that format. You can’t run analytics and gaps in care against documents. You have to break that down. You have to organize that. You have to normalize that.
As you push it back into the hospitals, or as you start to build communities out of that, you have the advantage of a system that was built from the ground up knowing that as you add data to it, you take it, put in discrete data, you merge that together with claims data. When it comes time to run an analytics view, it’s not only the valuable clinical data you’re doing that with, but you’ll also have the ability to look at the claims, where we identify that specific tests have or have not been done as well outside of the system because we see or we don’t see a claim for that.
Most technology vendors offer systems that were designed for statewide and regional exchanges, and sometimes they and their customers are still struggling to make that work. Will those products become obsolete, or is there room both for what Sandlot does and what they do?
That market will break itself up based upon how well the specific states did. There are some states, some of the smaller ones, who have been very successful in this. Very large hospital entities who have a very large market share, they came on board early, and in some cases they were innovators in what they did. Those have stabilized, and many of them have found a sustainable business model, which the HIEs have lacked forever.
Then there are systems that are being deployed right now, dollars being spent, and unfortunately those systems will never make it, because they don’t have that planned for that sustainable business model. We’re seeing private organizations saying, I need to do this. I have to do it for Meaningful Use. I need to do it to run my business. I’m taking on risk and I can’t take on risk if I can’t see both the clinical and the claims data for that patient. I can’t trust the state to get it done, so I’m going to go do it myself.
As a result of that, where we see the folks who really want to drive to make that happen, we’re seeing hospital associations stepping in and saying, “I’ll take that lead. I’ll run that,” or a lead hospital and the community saying, “I’ll take lead, I’ll do that.” We’re seeing that from two sides, where there clearly is plenty of room for us to coexist with the state systems that are out there, and in fact, connect to them as needed.
Insurance companies have jumped on the HIE technology business. Why do you think they were interested, and does that affect your business?
It certainly affects it, but maybe in some cases in a positive way. I’ll try to be kind here and not necessarily name names.
There is one of those entities who spent a fair amount of money — in the hundreds of millions of dollars — for one of those solutions. Unfortunately, the solution platform was near its end of life. As a result of that, many of their clients and many of those systems are really troubled. They’re ready to skip on to the next opportunity here with a richer set of analytics, with a richer set of things that one, aren’t going to cost as much; two, are far more creative with their capabilities; and three, can be turned up in timeframes measured in weeks, not in months, and the larger complex pieces measured in 100 days. I just made a commitment to do something that I will turn up 30 hospitals in 100 days. As a result of that, I think far more agile in that mode.
They are powerful when you find an area where they happen to be the carrier of choice. If you cross one of those paths … the other one on top there that is certainly quite sizeable has very good footprint, and when you look at that footprint and there is a relationship with them as the largest payer in the market and they rear their head. They’re capable, but as I heard, they’re quoting 15 weeks to do something that I can do in a week. The new generation of this drives down the cost significantly. I think they are opportunities for us. We are pursuing those entities knowing that they are quite vulnerable right now, and we’re getting traction.
Is there still an interest in acquiring companies like yours, and do you see that changing?
There is interest. Now we’re seeing others who have interest that see this market is quite rich in many ways. As soon as we start to see the risk markets stratify, there are entities who want to provide product that manages risk, they want to provide product that looks at analytics. Some more of an IT bent than those of a classical insurer, but I’m not having any discussions with any insurers right now.
Do companies try to cobble together a solution using something that’s strictly connectivity and then drop the analytics on the back end?
Of course. You can look at that as one of the insurers that you mentioned came from the other direction. They had those pieces and they tried to cobble on top of it an analytics tool and tried to bolt those pieces together to build something. You can get it to work. You don’t have the efficiency of it if you look at how those pieces are integrated.
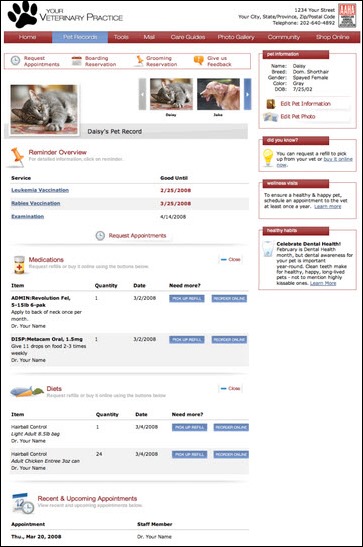
If you build it from the ground up, you are smart enough to say that if I have this piece of data and I want to offer a care manager … so one of the things we offer is care manager suite, it’s integrated right into the core foundation platform. If I’m looking at a patient that I’m managing under a care manager, one click and I get to see exactly what the reports would be on that patient. One more click and I can see exactly the medications that patient is on.
It is all pretty seamless, so when you look at it, has a nice look and feel to it. It’s pretty intuitive. It isn’t cobbled together so that somebody working with it has to say OK, this is obviously a different system, and this is obviously a different system. But I think over time, people will recognize they need to build those pieces out and they’ll come back with the products that are similar.
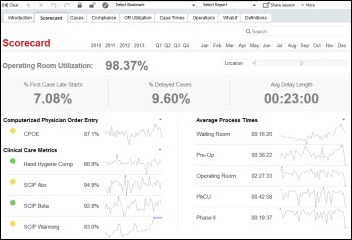
It would seem that the most oversold concept right now is analytics. Everybody says they’ve got it. Nobody really even knows what it means, much less what they’re trying to buy, or in some cases buying without even knowing what they’re going to do with it. What are the most useful or most commonly used analytics parts of your system?
NTSP as an organization was a pioneer. Took a second batch of pioneer, run a book of business through their own health plan, Care N’ Care, and operate a Secure Horizons book of business. By the time they’re done, there are about 80,000 at-risk patients sitting inside there. To climb the stars ranking, they started at three and a half stars. Over the last year, they climbed to four and a half stars. They did it by taking our analytics. The base piece of these are I ingest data such as A1C tests from a primary care physician or directly from a laboratory or from a specialist or from a bill that I’ve paid.
When it comes time to look at, am I compliant with my diabetics, am I compliant with hypertension, am I compliant with the various measurements required for five-star, I take that data, and at the time that the physician or anyone who’s caring for that patient, our analytic set metrics together with the product called Dimensions scans across that patient in milliseconds, identifying the presence of or the absence of whatever that patient needs — based on whether their particular age, whether their particular disease state — and within seconds identifies that these are the appropriate gaps for this patient that need to be dealt with. Then we have a proprietary capability that we’re patenting that allows us to push that message into the EHR platform without regard to who that EHR platform is. It’s something we call the digital envelope.
What are your thoughts on CommonWell?
I think the CommonWell organization is a good idea. We all know why they banded together. There is certainly a particular vendor out there who’d love to see all these things connected together in their own schema. The schema among how the hospitals can connect together when they’re on the same platform works quite well. When they’re on various platforms, a diverse platform doesn’t work at all.
There is defined need there. CommonWell saw that as an opportunity to say, if we pull together, I think we can do this. I think in the end, it’s a good idea. The more we get people out there who are opening these gates up, opening up APIs, making this data available on standards and moving it around, the better healthcare United States will be. I’m all in favor of that piece.
But as we look at it and say, where are the EHR vendors headed, it certainly seems that another round has occurred. I know three or four organizations that started the path with one EHR platform, cut their teeth on it, and now recognize it’s not going to be able to do what they want to do, and so they’re switching. As they switch, that churn seems to give them an uplift to organizations who recognize things that need to be in the next generation of EHR platforms. Some of these folks are seeing their market share go downhill and they’re chomping to see, can they do something in CommonWell that might help that.
At the same time, there are EHR vendors out there who are right on the cutting edge of what they need to with EHR systems to meet Meaningful Use, to be compliant in this area, to push CCDs and CCDAs around so that the information that people want to manage risk can be done without a lot of cost and without a lot of pain.
Some will suffer in this process and some will prosper, but I think the ones that I’m dealing with that I see … I mean, we’re talking large groups, not a doc here and a doc there. This is 116 docs here and 200 docs here, and they’re making those changes. All of that seems to help foster that as we connect to them, they’re ready for that next step. They’re ready to ingest the data that we pull together. They’re ready to have that be part of their system. They can compile whatever they do and send it back to me so I can do the same thing again and again.
Where do you see the company and the market being in five years?
I’m embargoed for about two weeks from the best example that I could give. We’re seeing these entities who had been put together in patchwork in the past and have tried to make that work recognize it can’t work. Consequently, these entities have stepped up. Hospital associations looking to say, I can solve this problem. Larger community rollups that say, I can solve this problem if I put a common umbrella or a common platform around it.
We have grasped this because it’s right in our sweet spot. We have the ability to take the output of another HIE platform — any of those insurance companies or the ones you spoke of or any of the other ones out there — and sit on top of them. As long as they are compliant with the latest standards, our ability to do HIE-to-HIE connectivity exists.
Certainly the ability to go out and connect the physicians where hospitals are really struggling so that they can’t buy physicians any more. They know they need this physician affiliation strategy. They’re going at risk in the community. They need the information to go at risk in the community. They’ve tried to hook up to the state systems, but they’re not cutting it. They see the timeframe that is going to take them, they are not cutting it.
A cloud solution like ours, our base product that can come in and fill it up pretty quickly, is pretty attractive. We’re doubling our sales force in the last month. We’re doubling our capacity. That should give you an idea of the kind of interest that we have in what we’re doing.
We’re doing some very innovative things in Medicaid space. We won a contract to demonstrate that you can manage Medicaid patients in the same way that CMS was trying to manage Medicare patients. The ACO models that drive down cost and improve quality for Medicare are applicable for Medicaid. We’re going to be demonstrating that. We won a contract to do that. There’s great hope in the sorts of things we can do with states that are struggling with lack of budgets largely due to healthcare costs in a Medicaid population. We’re right on the cutting edge of that and excited to be there, too.















































The story from Jimmy reminds me of this tweet: https://x.com/ChrisJBakke/status/1935687863980716338?lang=en