Jeremy Bikman is founder and CEO of Peer60 of American Fork, UT.

Tell me about yourself and the company.
I used to be at KLAS, running research sales strategy for seven years. Now I am in my apology tour, doing atonement to the industry with Peer60.
Our whole goal with Peer60 is to enable companies to get whatever data they need from customers and the market directly, with no one in between besides the platform. This lets them get tons of data a lot faster and hopefully have all the control they want from the information.
Why can’t vendor executives talk to their customer counterparts directly instead of hiring somebody else to do it for them?
I was talking with someone at my company yesterday about the management consulting thing. The cliché is, "All they do is interview people at the company that they consult with, then just repackage the answers." When I used to do some consulting, I would think the same thing. I would go, geez, all of the strategy for what this company should do is already contained in the minds of its own people, so why don’t they just go talk to the people?
I always wonder if it’s simply because it’s almost like in a war — everyone is in a foxhole and bullets are going overhead, so they can’t really step back and think strategically. Is that part of it? Is that just what happens? Do you need a third-party consulting firm or just a different set of eyes to look at it? Is it a case of “measure twice, cut once?”
That may be the reason why there are so many research firms out there. Maybe they have the connections. The companies don’t have the expertise themselves, or the time or the know-how to actually go do it, so they turn to that.
Is it a case of everybody loves being ranked? People obsess about, "Where I fit in comparison to everyone else?" I think everyone does that in life — we are always comparing ourselves to each other. Is that natural thing now happening and the research companies just leverage that to pump up a lot of interest to be able to sell? I know when I was at KLAS I took that angle. You’d say, "Here is where you are and here is where your competitors are, and hospitals are using it for this." It would generate a fervor that would build on itself. That’s how I would sell in some cases. Some of that still permeates.
Along those lines, are companies just looking for a customer-friendly "you’re doing a great job" validation or are they really looking for things they need to improve?
It depends on who you are looking at. Typically when you are talking to people who are in sales — and I’m a former salesperson, so I’m indicting myself in some aspects with this statement — those people are usually pretty tactical, where I’m thinking in the moment, "How can I get something done?" and I run off.
You have some exceptions out there. Some of the salespeople at Epic are exceptionally aggressive. I think Judy’s mandate was, "Just don’t lose a deal." They really get into it and they think strategically. There are obviously some other salespeople that think like that.
Within the organization, there are some people who care about the data, who care about the feedback. A lot of them also say, "I just care where we rank. I don’t care how truly accurate this information is. Is this statistically significant? I don’t care. I don’t care what this company’s research methodology is — look where we sit." Of course they take it and market it like crazy.
Is that accurate? No, but people are acting on it. My grandpa used to say, "Never confuse what should be done with what, frankly, is being done."
Do KLAS rankings and awards mean anything?
I think they do. KLAS does their best. Their data is not remotely statistically significant. When you go out and you’re talking to 15, 20, or 30 of someone’s customers over a 12-month period, that’s not relevant, but it is the voice of the customer. That is one thing that they are gathering. Those 30 or 40 hospitals they talk to for GE or Allscripts or anybody else — that is legitimate information, but is it a highly accurate rank about what is actually happening? Not necessarily.
It’s not just KLAS – it’s Black Book or anybody else who comes out with it. They are asking questions to CMIOs that CMIOs don’t know, such as work flow, and lower-level IT where their IT analysts can’t answer it. They’re also asking CMIOs some hardcore interoperability questions and maybe security that they may know in a secondary and a cursory way, but not primary themselves. A lot of its “opinuendo,” but it’s not just KLAS — it’s pretty much every research firm out there. That’s how they do it.
The most important information that you don’t see is who they’re talking to. If I want product-specific information, I’d want to talk to the person who works with it every day. But if I want to know from a marketing standpoint, “Is my customer going to fire me?” I’d want to talk to the person who has the clout to make that decision. Do they talk to the right people?
It’s obviously too much of a mix. Again, I just need to make clear that it’s every research firm. I haven’t come across a research firm that really does it right. But it’s part of the model, too. If KLAS, Black Book, MD Buyline, or anyone else were to say, "We have to segment our questions. Operational finance questions go just to people who are in operations and finance, IT questions go only to IT people and clinical workflow questions go just to those clinicians." They would have to do so much research that their cost would go through the roof.
People complain about how much KLAS costs right now. That’s nothing if they had to get a lot of data per user per that specific context that you really should be talking about. Like I said, operations questions to operations people, just limit it to that. It would be very, very difficult.
If you look in the fine print with KLAS, it says, “This is overall just the voice of customer.” They have little things in there, like confidence level isn’t with a C, it’s with a K. If you read the fine print — and they’ll admit it — this is voice of the customer. For the most part, the KLAS rankings do a pretty good job. Is it perfect? It is completely accurate? No way. No research I’ve seen out there is. It’s one the reasons why we started this platform.
If a company wants to go out and get feedback from the customers or the market in Europe and North America, they’re getting hundreds and sometimes thousands of responses within a week or two. In that, stats mean something. The questions get very specific. IT to IT people. Operations to operations people. Finance to finance. Of course, this is their data, it’s not going in the market.
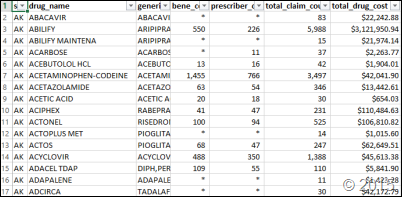
We’re producing these free reports just because it’s so easy for us to get the data. We did this clinical purchasing report. We got 25 percent of the hospitals in the US in three weeks. It’s very fast and easy for us to get the data. You’ve seen our reports. They’re pretty basic. Just, “Here’s the data.” We don’t really do much analysis. We’re not into the vendor rankings. Just, “Here’s interesting information.”
Our customers use that to get far more information far faster. Then they can do whatever they want at that point. We hope that they do it to improve, but we’re never going to rank vendors. That’s not who we are.
The source that I liked most, at least of those who provided their information without requiring payment, was CapSite. HIMSS Analytics bought them. How do you see HIMSS Analytics fitting into the market research world?
You know what I always wanted someone to do? I talked to HIMSS a couple years ago. They’re just too big. They can’t get out of their own way. Their data is pretty reasonably accurate to some extent. We buy it sometimes to make sure we have demographics for hospitals. Definitive’s doing a good job there, too.
I always thought some of these guys should go out and do what’s called an "ideal fit." You have a report come out that bashes Meditech from somebody, but Meditech is still selling. What about those smaller hospitals that don’t have very sophisticated IT environments? They don’t have much budget. They’re not going to sell out to one of the big IDNs or to a health plan or something like that. Meditech is a really good fit for them, but you don’t get that in “one size fits all” research. I remember telling HIMSS, "I know you guys are really trying to get more into this primary research, more away from just demographic information. Why don’t you go that direction?”
I hope someone does it. That would be way better for the market to rank vendors on where they actually play well. Why in the world are we comparing Meditech to Epic in a large hospitals? That doesn’t even make sense. That’s not where they play. They get crammed in and it does a big disservice to the market.
It would be like Consumer Reports saying that the best car is Rolls Royce and just leaving it at that. Healthcare has a list of best products and another list of all the types of hospitals — maybe the job of consultants is to arbitrage the information by matching them up.
That’s very good way to put it, actually. There are some consultants that can do that, real domain experts. They’ll take available data that’s out there. They’ll get a KLAS report, MD Buyline, whatever. Then they need to do primary research themselves. The hospital does, too. No hospital will go, "Oh, they rank #2 in this report – done. We’ll do it." They’re going to do site visits and they’re going to do calls. They have to go through their normal decision-making process. Money still means something. How much money do we have? Our internal capabilities still mean something from an IT and informatics perspective, biomed. These things mean things, so they will factor that into it. The “one size fits all” report does not do that. It lumps everybody together.
Just because of my background in working for a major research firm, every meeting I had at HIMSS, and I probably had 50 meetings, every person would go, "I hate this report. What do you think about this report?" I said, “I don’t really work there any more and I don’t really know that other research firm, but you have to quit trying to take these reports” … everyone is coming at it the wrong way. They anticipate that this should be an apples-to-apples comparison. They’re not apples-to-apples comparisons. You have to get that out of your head. The lens through which you view this has to be that there are both fruits or vegetables. It’s an apple to a kumquat or it’s like a fruit salad. That’s really what these reports are. Obviously there needs to be way more analysis that’s done and it’s probably like you said — that’s probably a time where some consultants need to step in and they can probably add real value.
f you’re talking to someone on the provider side who doesn’t really understand the vendor world, how would you describe what market research means to a typical healthcare IT software vendor?
It’s a crutch. Buying reports is a crutch. It’s an easy way out. Is that inflammatory enough? [laughs]
If you’re a vendor trying to formulate a market strategy, how important is market research? What else goes into that mix of saying, "What do we do for the next five years?"
Market research is great, but you need to it yourself. It needs to be primary. You don’t want it filtered.
There’s a saying that I’ve heard before. "If you drink from a stream, get as close to the source as possible." When you’re getting it filtered through a research firm and it’s anonymous, you have no idea who said what or anything like that. You’re getting an inherent bias coming from the research firm. No matter what they try to do — and you can read all the philosophy of Immanuel Kant and those other ones out there that talk about this, those German philosophers — there can’t be anything truly objective.
It becomes far less objective when it’s filtered through somebody else. Someone else made the calls. Someone else is now analyzing the information. They’re trying to keep it as pure as possible, but they’ll see some phrases and the natural tendency is to try to clean it up. It’s like the Bible. the Bible has been translated how many different times? From Aramaic into Greek, into Latin, into German, into whatever. How much stuff gets lost in that translation? Same thing happens.
Market research is absolutely critical. Research and getting data from the customers is critical. But get it directly from them and get a lot of it. Get it repeatedly. Make it easy for them. That’s the reason I say market research reports are a crutch. Hiring a research firm to do custom research for you is a little bit better than that, but still you are ceding control to somebody else.
It’s as if you hired someone else to do this interview and they didn’t give you a direct transcript. They’re going to change it. That’s the way research works. You get it and go, "This is interesting," but you can tell it’s bland. You can tell something’s have been changed rather than getting it unfiltered.
You talked about Epic’s sales and marketing. They claim they don’t do marketing and they don’t ever talk about their sales. Does Epic do sales and marketing?
Oh, my gosh, they are the best in healthcare. It’s brilliant.
Have you seen the show “Usual Suspects?” It’s a brilliant show. There is a guy Verbal Kint played by Kevin Spacey. The main villain is this guy named Keyser Soze, this super evil global Mafioso boss who no one has ever seen. Verbal says, "The greatest trick the Devil ever pulled was convincing the world he did not exist.”
It’s brilliant, that line. Every time someone says Epic doesn’t sell or market, I laugh about it. They are brilliant at it. By virtue of saying they don’t market, that is different. It sets them apart. What is that? That is marketing. You just established a brand.
They’re not traditional though. They’re very thoughtful. They’re very extremely aggressive, but they do it in a very calculated way that’s not offensive and doesn’t feel like sales is coming across. They’ve earned a lot of it, too.
I want to preface that out front. When you have companies like KLAS ranking them constantly and other publications are constantly publishing the rankings, you are using that to your advantage. When other people market for you, that is way better than when you’re doing it yourself.
Epic absolutely markets. They just do it in the early Silicon Valley way. The rest of healthcare needs to catch up, which is have other people market, be almost counterculture. That is really Epic. They are just brilliant at it. Absolutely brilliant at it.
Epic somehow always seems to slide across from being on the other side of the table to their customer’s side. The customer feels that Epic is their partner and defends them. How would you create something like, that where both contractually and morally, the customer feels the imperative to be their vendor’s advocate?
You see that in Silicon Valley. Look at Apple. I like Apple just because it’s stable so I don’t really care, but people are violently defensive of Apple. Epic does the same thing. It’s not about the solution.
When I was at KLAS, people would complain, "Epic can’t get this — they have older technology." I would say, “Yes they do — it’s not about the technology.” As long as the technology is stable and does the basics, it’s all about the people. It’s the the relationship and the feeling. My dad used to say, "Son, you only sell two things in life — solutions and good feelings.”
That’s correct. Epic solves a problem. Companies solve problems and how you feel about that. Epic is really good, like you said, at getting themselves on that same side of the table. They don’t talk about their tech a lot — they talk about the problems they are solving and the benefits they are providing. Apple did that. Steve Jobs always talked about “why we do what we do,” not all the features. Those will come later. They would build this whole culture. That is really what Epic has done.
Can another company do it? I don’t think they can if they don’t start out that way. You’d have to do a scorched earth. Before Siemens got bought out by Cerner, to turn it around, John Glaser would have to come in and say, "I’ve got to fire everybody. Anyone that’s been hired here previous to two years that doesn’t have a lot of neural plasticity, doesn’t have a lot of bad habits — we’re just going to get rid of everybody. We’re going to start from the ground up.“
I don’t know how a company pivots. I haven’t seen a company pivot like that. Maybe you have, I just haven’t seen someone. You have to start out like that. You can obviously improve, but you also need to be yourself. Epic is Epic because of Judy and Carl. You don’t have to be like that. Cerner is highly successful and you wouldn’t really say their culture is very similar to Epic.
What are the most interesting trends you took away from the HIMSS conference?
The most interesting trend that I’ve seen — this is a bit tongue in cheek — is how fast marketing moves. Products move at glacial speed in comparison to marketing. I am absolutely blown away that pretty much every company out there can do accountable care, care coordination, population health management, patient engagement, and data analytics. It’s amazing. It was like a forest just crept up over the last two years.
I may be underselling everybody, but their marketing departments are in full bloom. I’m not sure the R&D is there. I spent so much time just meeting with people. It was hard. That was just one of my takeaways, "Wow, everybody does everything and nobody is standing out because of it."
In our 2011 interview, you predicted that Epic and Cerner would lose some dominance, best-of-breed would make a comeback of sorts, and smaller vendors would upset the apple cart. Do you still think that will happen?
Because the government is in, no, I don’t. I was wrong.
The big are going to get stronger because what the government has done is going to enable it. It makes it tougher. When you have government-required mandates that somehow map well to the “one size fits all” big integrated vendors, how do you fight that?
Imagine if you are in Silicon Valley and all these B2C companies. The government came in and said, "Here are all the different mandates you have to do." How many new startups could crop up and really be successful?
I underestimated the impact and the staying power of what was enacted through HITECH legislation. When it comes to enterprise, maybe in 10, 15, or 20 years, but nothing soon. The governments has enabled this to happen and smart vendors like Epic and Cerner absolutely jumped on it and have done exceptionally well. It’s not like they haven’t done a good job anyway, but there is no doubt it certainly helped.
In that regard, is there irrational exuberance with mobile health and the unprecedented amounts of money being invested in innovative companies?
I love the energy. When you have a lot of companies coming in and competing, hopefully you can get to something that is really usable, specifically for patients, that really engage them without having hospitals having to do the heavy lifting, which is happening now. What if the government steps in there and starts putting all these mandates around that? It is just going to empower the incumbents. That still isn’t good for innovation or for patients. I hope that it stays the Wild West for a while.
What will the health IT market look like over the next five years?
Big getting bigger. You are going to see a lot more consolidation. There are some pretty cool startups and a lot of cool companies. You are going to see a lot more consolidation. I don’t think that Athena and some other guys are even close to being done, snapping up different companies and rounding things out. Salesforce is coming in in a big, big way. Amazon is coming in. I just got an email from a guy at a major IDN saying, "Hey, you’ve got watch out for Amazon — they’re doing some amazing things. They are moving stuff to the cloud and are starting to bring all these different apps no one is even talking about.”
I kind of love that, but I don’t know if they are going to stick around. We’ve seen the hokey pokey dance go on in healthcare for decades, where guys jump in and jump out. I’m sure hoping that a lot of these guys will stick in – Salesforce, etc. — and really help out. An argument could be made that guys like Salesforce need to be in there. If you are really going to engage patients and you’re really going to manage populations, CRM-like technology may be absolutely critical. Can the big incumbents in healthcare really develop a CRM? I don’t know. I don’t think so, but they certainly could.
Did the FDA really come look at your fake crack booth giveaway at HIMSS?
They did. Did I tell you my marketing guys didn’t take a picture of it? They did a great job. I said, I’d have given you an A+ because it was such an awesome event, the booth, everything, the traffic, but the FDA came by after hearing, "What’s this? You guys are giving away dime bags?" Do you really think we are giving away illegal substances at a trade show? Besides, it would be cheaper for us to give away iPads. We should have gotten a picture.




























































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…