Top News

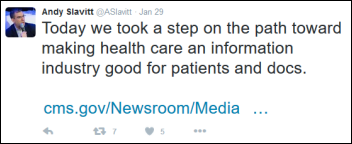
The White House will ask Congress to approve $1 billion for President Obama’s so-called “cancer moonshot.” Some of the areas to be funded within HHS are early detection via genomics, enhanced data sharing among institutions, and a virtual FDA Oncology Center of Excellence to review new combination products.
Reader Comments

From Judo Chop: “Re: Florida Hospital and Athenahealth. This is part of the December announcement by its parent company Adventist Health System selecting Athenahealth. Florida Hospital will replace a combination of Epic ambulatory EHR that’s used in a handful of clinics, Cerner ambulatory EHR, and Allscripts (the old Misys product) PM. Most of the rest of AHS is using NextGen’s EHR/PM.“ Adventist announced in December that it will be deploying Athenahealth’s PM/EHR to 1,600 employed physicians.
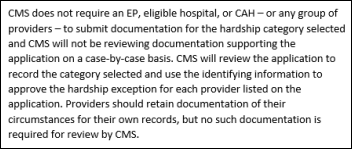
From Polecat: “Re: Meaningful Use hardship exception. The new form doesn’t even ask the EP or EH to submit documentation of their claimed reason.” Correct. I think we can assume that this wink-wink form means CMS will allow anyone to avoid EHR penalties. MU is an embarrassment to everyone involved at this point and even the government is trying to distance itself from it. Just check “EHR Certification/Vendor Issues” and you’re done.
HIStalk Announcements and Requests

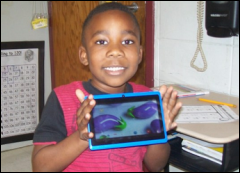
Mrs. Haley from Georgia couldn’t wait to send photos of her special education and gifted students using the three tablets we provided in funding her DonorsChoose grant request. She took these photos the day they arrived, where she had already installed reading and testing apps.
Also checking in was Mrs. B from North Carolina, who just got word that we had funded her request for science activity tubs. She says, “I couldn’t believe the email I received with information about my project … I yelled out loud and other staff members came to my classroom to see what was going on … I try to purchase what I can, but it seems as if my money is not going very far these days. Thank you very much from the bottom of my heart. You have made one teacher very happy … You will never know if a future mineralogist, petrologist, or geologist will be inspired by these kits!”
I was thinking today: has anyone actually ever heeded the warning to, “If this is a medical emergency, hang up and dial 911” after hearing those boring, time-wasting phone tree warnings when calling everyone from a dermatologist to a drugstore?
HIStalkapalooza
HIStalkapalooza Sponsor Profile – Fujifilm


With 16 years of industry-leading experience, our TeraMedica division remains independently focused on advancing VNA technology and healthcare interoperability while now leveraging Fujifilm‘s clinical capabilities. As the centerpiece of Fujifilm’s comprehensive medical informatics portfolio, Synapse VNA provides the industry’s leading image management solution. Fujifilm is proud to sponsor HIStalkapalooza. Visit us during HIMSS16 for all your medical informatics requirements, Booth #1024.
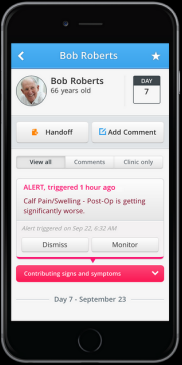
HIStalkapalooza Sponsor Profile – PatientSafe Solutions

PatientSafe Solutions has mobilized clinicians and redefined clinical workflows for more than a decade. Meet our team in Booth #4257 to learn how our Clinical Communications platform improves patient care and satisfaction while decreasing costs. Meet us at HIMSS. Our team can’t wait for HIStalkapalooza this year. Look for us at the event to get your picture taken for the 2016 HIStalkapalooza video!
Webinars
None scheduled soon. Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock
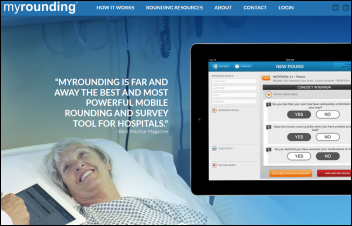
Huron Consulting Group acquires 25-employee, Denver-based MyRounding, which offers a mobile rounding and survey tool for hospitals.

Aetna announces that its profit jumped 38 percent in the most recent quarter, mostly due to its Medicare and Medicaid business, but says it lost money on its exchange-issued policies and warns that it has “serious concerns about the sustainability of the public exchanges.”

Alphabet, the recently formed parent company of Google, surpasses Apple as the world’s most valuable company after reporting impressive numbers in its first detailed report. Alphabet made $4.9 billion in profit on $21.3 billion in revenue for the quarter. Share price jumped 8 percent on the news, raising the company’s market capitalization to $559 billion.

Sunquest parent Roper Technologies reports Q4 results: revenue flat, EPS $1.82 vs. $1.85, missing estimates for both and issuing 2016 guidance below expectations. The CEO said in the earnings call, “We think we will have mid-single digit organic growth in Medical throughout 2016 and we think that will get stronger as the year goes on. Sunquest has a number of version changes and software release updates that are rolling out in the second half that will be quite beneficial. And then Strata, Data Innovations, and SoftWriters which are growing rapidly, will become organic in the second half. Verathon and Northern Digital are going to continue to grow at a relatively high rate in 2016. And then we closed on January 7 the CliniSys acquisition in the UK, which is a European hospital laboratory software provider, and it will add to our acquisition sales growth in 2016.”
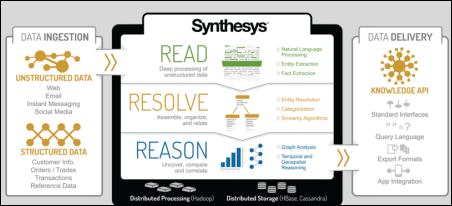
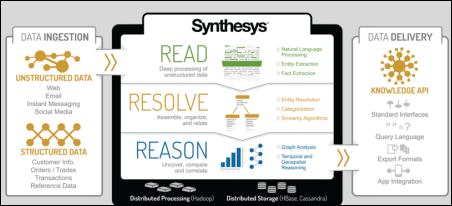
Machine learning vendor Digital Reasoning, which acquired Shareable on January 8 to create its healthcare business, raises $18.6 million, increasing its total to $53 million.

A New York Times article questions whether it was wise for the struggling Theranos to hire star litigator and company director David Boies as its legal representative, given that he would be representing Theranos management as a lawyer while his responsibility as a director is to the company’s shareholders. It concludes,
The potential for conflict is particularly great. What if Ms. Holmes resists changes that would be in the interest of shareholders? What if the board decides that it is time for her to go — and she stands her ground? The board could do little more than throw up its collective hands under the current governance structure. Mr. Boies and the other outside directors could resign in protest. But why would anyone, particularly Mr. Boies, be a director on a board that lacked the power to make fundamental changes? Indeed, what is Mr. Boies thinking? He may be paid lots of money for his roles, but for someone so successful and savvy to put himself in a position that is bound to be problematic is puzzling.
Meanwhile, Theranos finds another foot to shoot in indefinitely delaying its October promise to allow Cleveland Clinic to validate its technologies and insisting that it won’t publish anything about those technologies in peer-reviewed journals until it receives FDA approval for all 120 of its tests.
Sales

Joseph Brant Hospital (Ontario) chooses FDB MedsTracker MedRec for medication reconciliation.
Craneware signs a $7.5 million contract with an unnamed hospital operator.
People

Seattle Children’s Hospital (WA) names interim SVP/CIO Jeff Brown (Lawrence General Hospital) to the permanent role. He holds three master’s degrees in business administration, executive management, and health informatics.

Allscripts names Melinda Whittington (Kraft Foods Group) as CFO.



CareSync hires Russell Dumas (Napier HealthCare) as VP of clinical operations, David Antle (BobCAD-CAM) as VP of client services, and Teri Spencer (GTE Financial) as VP of human resources.

Cumberland Consulting Group hires Terrell Warnberg (QHR) as partner over its new performance improvement practice.


The Health Information Trust Alliance (HITRUST) appoints Epic President Carl Dvorak to its board and names David Muntz (GetWellNetwork) as senior advisor of public policy.

Athenahealh hires Prakash Khot (Kaseya) as CTO.

Laura Momplet, RN (Dignity Health) joins CTG as chief operations officer and chief clinical officer.
Employee health platform vendor Healthcare Interactive names John Capobianco (KickStart Partners) as president and chief marketing officer.
Announcements and Implementations

Craneware will offer patient payment plan technology from VestaCare with its medical necessity and price estimation products.

Premier announces that it will conduct Innovator Research using Medicare data from CMS’s Virtual Research Data Center. Premier’s research division will analyze episodes of care to identify best clinical practices for care improvement and cost reduction.
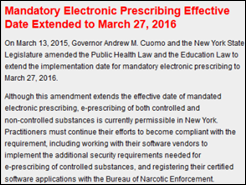
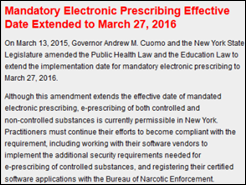
A Surescripts study of New York providers finds that 93 percent of pharmacies can receive electronic prescriptions for controlled substances while only 27 percent of prescribers have the technology to issue them. It also finds that 58 percent of prescribers are issuing electronic prescriptions in general. New York’s I-STOP law requires that all prescriptions be transmitted electronically by March 27, 2016, meaning a huge number of prescribers need to take action in the next seven weeks.
Government and Politics
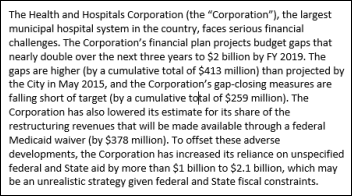
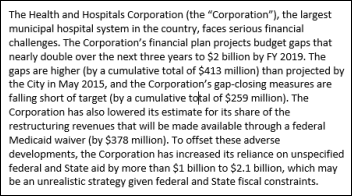
New York Mayor Bill de Blasio hires a consulting firm to figure out what to do about the city’s 11-hospital Health + Hospitals Corporation, which despite extensive city support is expected to run a deficit of $2 billion within the next three years. The health system hopes to convince more patients with commercial insurance to use its facilities than those of its competitors, all of which have similar ambitions.
Privacy and Security

Australia’s Royal Melbourne Hospital says it hasn’t completely eradicated the Qbot malware that infected its Windows XP computers two weeks ago. The hospital says the virus mutated six times in a single day. The keystroke-capturing malware penetrated the hospital’s pathology computers via a Windows XP exploit, managing to evade detection by the hospital’s updated antivirus product.
Other

A study finds that mobile text messaging increases medication adherence rates in chronic disease patients from an assumed baseline of 50 percent to 68 percent, although the sites that are screaming this out as big news failed to note that:
- It’s a meta-analysis, meaning that instead of doing new research it just combines information from previously published studies.
- The studies it reviewed involved fewer than 3,000 patients combined.
- Texting results were measured only for a short duration.
- The studies relied on what patients said they did rather than measuring what they actually did.
- The text messaging in each study was not consistent as to frequency and style.
This is not newsworthy other than the fact that it was published in JAMA Internal Medicine, where it will reach a wide audience. It’s also surprising that the journal misspelled the name of the Johns Hopkins Bloomberg School of Public Health in its author affiliation section.

Duke University Health System (NC) reports making a record profit of $355 million for 2015, explaining that, “For the three or four years leading up to this past year, we had made a series of investments in facilities and information systems that helped to relieve capacity constraints limiting growth … With our new IT capabilities, we are able to better manage care across the spectrum and become more efficient in that way.” The system said it made a lot of money by buying up oncology practices to increase inpatient volume.
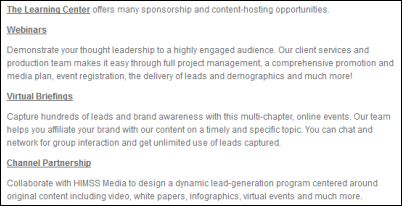
I received a survey link from HIMSS about its Learning Center, which sells thinly disguised advertising via its HIMSS Media business. Being a member of HIMSS means being inundated with its vendor-sponsored pitches, in this case disguised as “education,” where high-paying vendor members pay dearly to be hooked up with low-paying provider members in the “ladies drink free” business model.

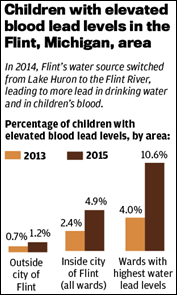
The Virginia Tech professor who led the study proving that the water in Flint, MI contains dangerous levels of lead says public science is broken as university faculty members are pressured to get funding and to become famous. He explains, “Where were we as academics for all this time before it became financially in our interest to help? … Science should be about pursuing the truth and helping people. If you’re doing it for any other reason, you really ought to question your motives … Everyone’s invested in just cranking out more crap papers … when you reach out to them, as I did with the Centers for Disease Control and Prevention, and they do not return your phone calls, they do not share data, they do not respond to FOIA … every single rock you turn over, something slimy comes out.”
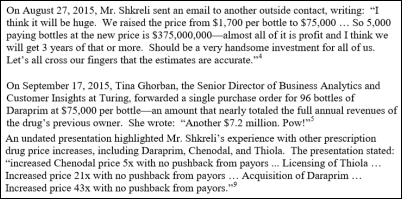
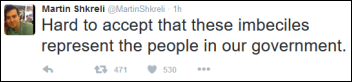
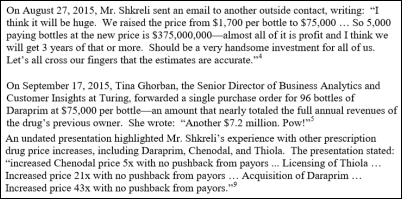
A Congressional investigation finds that despite the patient-focused claims of since-fired Turing Pharmaceuticals CEO Martin Shkreli, the company was gloating with delight at the profits it would make by jacking up the price of ancient drug Daraprim by 50-fold.
Weird News Andy titles this sad story “Out of the frying pan and into the fryer.” A patient with mental illness jumps out of a moving ambulance while being transported from a hospital and is struck and killed by a driver who then fled the scene.
Sponsor Updates
- Catalyze co-founder and CEO Travis Good, MD will speak on “Excitement in Healthcare Regulation” at the 2016 Hosting Milestone Summit Series on February 4 in Las Vegas.
- Divurgent will attend the South Carolina HIMSS Networking Reception & Dinner February 4 in Columbia.
- FormFast gears up for HIMSS16.
Blog Posts
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Send news or rumors.
Contact us.















































































If they haven't coordinated with the patient safety team, they have by definition "dropped the ball". And, given the reported…