News 10/25/17
Top News
Imprivata acquires Caradigm’s identity and access management business for an unspecified amount. Caradigm, a GE Healthcare company, has been in the process of streamlining operations for several years now. It announced workforce reductions in April, and August 2016.
HIStalk Announcements and Requests
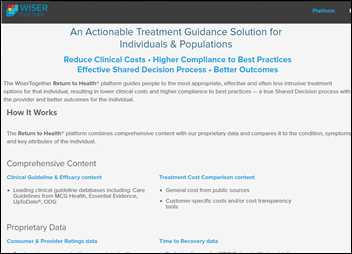
Welcome to new HIStalk Platinum Sponsor WiserTogether. The Washington, DC-based company’s treatment guidance platform improves outcomes and satisfaction while lowering cost. People and populations use its Return to Health solution to select the most appropriate and effective personalized treatment option in sharing decision-making with their provider. Condition, symptom, and demographic information is assessed against clinical efficacy and guideline content, treatment costs, provider ratings data, and time-to-recovery guidelines to present treatment options labeled as Poor, Good, and Best. Nearly 90 percent of users choose effective treatments, reducing the use of ineffective tests and treatments by 25 percent in creating a 400-900 percent ROI. The company just announced enhancements that include analytics and reporting that allows healthcare organizations to understand how patients make treatment decisions and which options they are likely to choose. Thanks to WiserTogether for supporting HIStalk.
I came across this video describing how patients can use WiserTogether’s Return to Health tool to find evidence-based treatments that are cost effective.
Webinars
Here is the recording from today’s webinar with ZappRx on improving care and saving time with streamlined specialty drug prescribing.
October 25 (Wednesday) 1:00 ET. “Delivering the Healthcare Pricing Transparency that Consumers are Demanding.” Sponsored by: Health Catalyst. Presenter: Gene Thompson, director, Health City Cayman Islands. Health systems are unlike every other major consumer category in not providing upfront pricing information. Learn how one health system has developed predictable, transparent bundled pricing for most major specialties. Attendees will gain insight into the importance of their quality measures and their use of actual daily procedure costing rather than allocated costs. They will also learn about the strategic risk of other market participants competing with single bundled pricing. The organization’s director will expand how its years-long process is enabling healthcare delivery reform.
October 26 (Thursday) 2:00 ET. “Is your EHR limiting your success in value-based care?” Sponsored by: Philips Wellcentive. Presenters: Lindsey Bates, market director of compliance, Philips Wellcentive; Greg Fulton, industry and public policy lead, Philips Wellcentive. No single technology solution will solve every problem, so ensuring you select the ones most aligned to meet your strategic goals can be the difference between thriving or merely surviving. From quality reporting to analytics to measures building, developing a comprehensive healthcare strategy that will support your journey in population health and value-base care programs is the foundation of success. Join Philips Wellcentive for our upcoming interactive webinar, where we’ll help you evolve ahead of the industry, setting the right strategic goals and getting the most out of your technology solutions.
November 8 (Wednesday) 1:00 ET. “How Clinically Integrated Networks Can Overcome the Technical Challenges to Data-Sharing.” Sponsored by: Liaison Technologies. Presenters: Dominick Mack, MD, executive medical director, Georgia Health Information Technology Extension Center and Georgia Health Connect, director, National Center for Primary Care, and associate professor, Morehouse School of Medicine; Gary Palgon, VP of healthcare and life sciences solutions, Liaison Technologies. This webinar will describe how Georgia Heath Connect connects clinically integrated networks to hospitals and small and rural practices, helping providers in medically underserved communities meet MACRA requirements by providing technology, technology support, and education that accelerates regulatory compliance and improves outcomes.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock
Select Medical Holdings will combine its Concentra occupational and urgent care company with California-based Dignity Health’s US HealthWorks subsidiary as part of an expanding partnership that includes the joint development of a 60-bed hospital and operation of 12 outpatient clinics in Las Vegas.

Life insurance company John Hancock dangles $25 Apple Watches to lure customers into its Vitality health and wellness program. Members who exercise regularly for two years will avoid having to pay off the typically $300 device in installments.

Nuance points the legal finger at MModal, alleging in a lawsuit that MModal products violate patents pertaining to transcription, speech recognition, and computer-assisted physician documentation technology. The lawsuit comes four months after Nuance suffered a malware attack on its cloud-based services that led to a $15 million loss in Q3.
![]()
Newton, MA-based Devoted Health raises $62 million, bringing its total to $69 since launching earlier this year. Company founders Ed and Todd Park (brothers of Athenahealth fame, among other illustrious health IT roles) plan to offer concierge-style Medicare Advantage plans beginning in 2019 that will incorporate house calls and virtual visits.
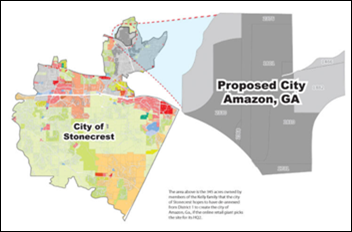
Amazon receives 238 bids from 54 states, provinces, and territories all vying to attract the company’s second headquarters. Amazon plans to invest $5 billion in the new facility, which will employ 50,000. Given its recent interest in health IT, it will be interesting to see if “Amazon HQ2” lands in a health IT-heavy town. As one would expect, city officials have dangled tax breaks and other incentives in front of the world’s largest online retailer. Outside of Atlanta, City of Stonecrest Mayor Jason Lary has promised to develop the city of Amazon and appoint Jeff Bezos as its lifelong mayor.
Reuters reports that Siemens has enlisted three banks to lead the organization of an early-summer IPO for its Healthineers unit.
Announcements and Implementations

Regional Health (SD) goes live on Epic over the weekend.

Swedish Bellevue Primary Care (WA) becomes the fourth Swedish location to roll out Versus Technology’s real-time locating system.

Definitive Healthcare adds retail clinics and assisted living facilities to its market research database of providers.

Thibodaux Regional Medical Center (LA) implements electronic signatures and forms technology from Access.
People

Tom Visotsky (HCS) joins Kno2 as VP of vertical market sales.

Cancer informatics company Inspirata names Josh Mann (Mann Consulting & Ventures) VP of its Cancer Information Data Trust Program.

Vikram Natarajan (Medfusion) joins SPH Analytics as SVP of development and IT.


Tenet Healthcare names Executive Chairman Ronald Rittenmeyer interim CEO. He takes over from Trevor Fetter, who announced his resignation in August after a two decade career at the Dallas-based health system. Tenet has been exploring strategic options recently, including the potential sale of parts of the company, and has been in the public eye over disagreements with investors over strategy, takeover rumors, and board-level resignations.
Technology

Medecision debuts new care management apps related to population analytics, EHRs, financial performance, risk scoring, and care coordination. The company will launch apps for care engagement and operational efficiencies later this year.
Government and Politics
Ft. Lewis, WA-based Madigan Army Medical Center goes live on Cerner, the fourth major installation of the DoD’s MHS Genesis program. The center is the largest of the program’s inpatient facility implementations, and the final one in the Pacific Northwest. I like that they’ve gotten a patient to host their tutorial videos, the first of which is accompanied by an 80’s-era soundtrack that will have you reminiscing about Jazzercise and GI Joe quicker than you can say “New Coke.”
A federal court dismisses CliniComp’s August lawsuit against the VA, which alleged that the administration had improperly issued Cerner a no-bid contract for a VistA replacement. CliniComp CEO Chris Haudenschild has vowed to appeal, adding that the company “simply wants the chance to prove that it can do the job cheaper, faster, and better.” The company’s systems are used in several VA hospitals.
Innovation and Research
The COPD Foundation, Geisinger (PA), GSK, and Jvion embark on a project that will identify COPD patients at risk of hospitalization and/or readmissions. Funded by GSK, the two-phased project will pair the foundation and Geisinger’s clinical expertise with Jvion’s AI-based patient risk stratification technology.
Black Book survey-takers rank Navicure as the top RCM technology vendor, with Experian, Patientco, Change Healthcare, InstaMed, and NThrive also scoring high for end-user satisfaction.
Other
The New Yorker digs into the pharma moguls of the Sackler family (apparently known more for their philanthropy than to the development of OxyContin) and their ties to the rise of pharmaceutical advertising, which some physicians feel account for the lion’s share of today’s opioid epidemic.

This is a breach of a different kind: Saline Memorial Hospital staff receive an unexpected (and no doubt unruly) visitor when a deer crashes into its courtyard, prompting Arkansas Game and Fish to come and remove the animal.
Sponsor Updates
- Besler Consulting releases a new podcast, “Reducing Medicare spending through electronic health information exchange.”
- Carevive wins the 2017 Cerner Emerging Partner of the Year Award.
- Centrak will exhibit at LeadingAge October 29-November 1 in New Orleans.
- CoverMyMeds will exhibit at the CBI Electronic Benefit Verification and Prior Authorization Summit October 24-25 in San Francisco.
- Dimensional Insight will exhibit at the Hospital Quality Institute November 1-3 in Monterey, CA.
- EClinicalWorks will exhibit at the Connected Health Conference October 26-27 in Boston.
- FormFast, HealthCast, Impact Advisors, InterSystems, and Intelligent Medical Objects will exhibit at the CHIME CIO Fall Forum October 31-November 3 in San Antonio.
- Healthwise will exhibit at the HealthTrio 2017 Users Group Conference October 25-27 in Tucson.
- Optimum Healthcare IT publishes a new case study, “Epic Help Desk and Call Center Support at The Guthrie Clinic.”
- Iatric Systems will exhibit at the HCCA Regional Conference October 27 in Chicago.
- AdvancedMD, Clinical Architecture, and CompuGroup Medical join CommonWell.
- Nordic releases a new podcast, “How to communicate effectively during your EHR transition.”
Blog Posts
- Guess Whose eSignature Solution Meditech Uses? (Access)
- Difference between Machine Learning, Data Science, AI, Deep Learning, and Statistics (Agfa Healthcare)
- Mapping Digital Health: an Interview with Strata Health Executive VP Peter Smith (Datica)
- CEO Perspective: CarePort as a Company (CarePort)
- Chronic Care Management: Choosing the Right Care Coordination Company (CareSync)
- How Physician-Owned Practices can Generate Great Patient Reviews (ChartLogic)
- Understanding Customer Experience at Diameter Health (Diameter Health)
- How nurse-performed ultrasound is improving patient care and nursing efficiency (Elsevier Clinical Solutions)
- Innovations From Our National Conference (EClinicalWorks)
- Why You Should Consider Outsourcing Your Legacy Support During a System Implementation (Hayes Management Consulting)
- Management of Enterprise IT in Healthcare Environments (The HCI Group)
- How Consumers Can Use The National Health Index to Navigate Their Care Journey with Confidence (Healthgrades)
- What Works – Data Analytics and Business Intelligence Assessment Results in Strategic Roadmap and an Actionable Plan for Success (Huntzinger Management Group)
- EHR Satisfaction Survey 2017 – Do You Agree with the Results? (Iatric Systems)
- What is Master Data Management and Where Should I Start? (Impact Advisors)
- Is the Quality Payment Program the most disruptive feature of MACRA? (Imprivata)
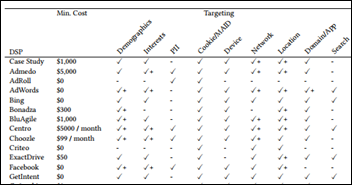
- Creating More Effective Healthcare Ads (Influence Health)
- Why Are We Still Talking About EMV Two Years After the Liability Shift? (InstaMed)
- Revenue Cycle Readiness: Looking Beyond the Numbers (Leidos Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne, Lt. Dan.
Get HIStalk updates. Send news or rumors.
Contact us.





















































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…