News 3/16/16
Top News

Nearly 31,000 patients of St. Joseph Health (CA) will get checks for $242 each following the hospital’s $7.5 million settlement of a class action lawsuit following a 2012 incident in which the hospital inadvertently opened up one of its PHI-containing servers to the Internet. The hospital paid another $7.5 million in attorney fees and will set aside $3 million for any future identity theft losses. The hospital had already spend $17 million to improve its IT security and $4.5 million for credit monitoring for the affected individuals. That’s nearly $40 million in potential eventual payouts.
Reader Comments
From PitViper: “Re: blockchain. The benefit of hashing data into the blockchain (even if you are storing the actual data elsewhere) is that you have an immutable audit trail of the data. Nobody can go in and update the information unilaterally. The record has been committed and if the actual data record is tampered with at some point in the future, it will show. This is important for the data integrity of medical records.”
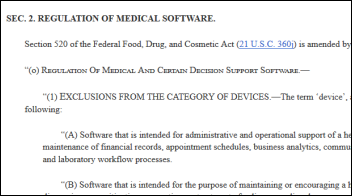
From Me Dislike Collusions: “Re: MEDTECH bill. Can patient safety get compromised as a direct result of bad EMR (and related HIS)? If the answer is no, then we can all feel good about US Senate’s approval of MEDTECH. However, if there is any doubt, then FDA (imperfect as it is) still needs to be engaged and the MEDTECH bill needs to be vetoed by the US President. I am surprised at the lack of protests, especially from the doctors. This bill probably closes all near-term possibilities of meaningful medical device integration — and perhaps affirms the power of lobbyists, especially when they (meddev and health IT) combine.”
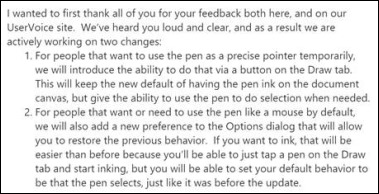
From Support Analyst: “Re: Epic stars program. Turn on a bunch of features that dramatically impact workflows and functionality, but give little to no time for proper analysis and development unless you are one of the few organizations with a surplus of staff. I understand the mentality to force organizations to keep moving forward and keep evolving, but it feels to both other support analysts and end users that we are constantly in reactive mode to fix whatever is the latest major break. Users are frustrated, losing confidence, and are quickly shutting down. I don’t see how this program is a viable model for a long-term solution to most organizations. Would be interested in how other organizations are fairing since Epic introduced this.”

From PM_From_Haities: “Re: Epic. They deliver and continue to deliver. That’s the difference between it and other EHRs. Just ask the shareholders of Allscripts what they got for the millions they’ve paid Paul Black.” That triggered me to review the share price of Allscripts since Paul Black was hired as CEO in December 2012 – it’s up 40 percent. Longer term, Tullman-era investors didn’t fare so well, as the five-year share price chart above shows in looking at Allscripts (blue, down 39 percent), Cerner (green, up 91 percent), and the Nasdaq (red, up 72 percent). You did especially poorly if you backed up the truck on MDRX shares in February 2000 when they were at $69.00, now down 81 percent.
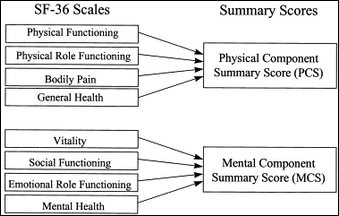
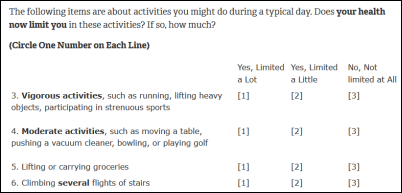
From Specific Gravity: “Re: SF-36. I’m curious to learn more about your SF-36 wellness questionnaire idea. Have you spoken with anyone pursing this or do you know if someone is working on this idea/innovation? I have many ideas on how to make this a reality.” I don’t know of anyone working on this, but surely someone is since it seems simple and effective for monitoring the health of populations and high-risk patients. Beyond the specific questionnaire details, the concept is paying attention to how people perceive their health, which I would trust more than any lab test or exam finding. Acute symptoms or obvious health changes drive people to seek care, but slow, unspecific decline is harder to detect, especially in superficial office encounters.
HIStalk Announcements and Requests

Mrs. Ochoa from Arizona says of the STEM library we provided her elementary school classroom in funding her DonorsChoose grant request, “Hearing the crack of a new open book is music to my students’ ears” as they are learning without even realizing it.

Also checking in from his Arkansas middle school is Mr. Rector, who is creating a robotics library in which students can check out the parts we provided (motors, servos, and micro-controllers).
Webinars
March 16 (Wednesday) noon ET. “Looking at the Big Picture for Strategic Communications at Children’s Hospital Colorado.” Sponsored by Spok. Presenters: Andrew Blackmon, CTO, Children’s Hospital Colorado; Hemant Goel, president, Spok. Children’s Hospital Colorado enhanced its care delivery by moving patient requests, critical code communications, on-call scheduling, and secure texting to a single mobile device platform. The hospital’s CTO will describe the results, the lessons learned in creating a big-picture communication strategy that improves workflows, and its plans for the future.
March 16 (Wednesday) noon ET. “The Physiology of Electronic Fetal Monitoring.” Sponsored by PeriGen. Presenter: Emily Hamilton, MDCM, SVP of clinical research, PeriGen. This webinar will review the physiology of EFM – the essentials of how the fetal heart reacts to labor. The intended audience is clinicians looking to understand the underlying principles of EFM to enhance interpretation of fetal heart rate tracings.
March 22 (Tuesday) 2:00 ET. “Six Communication Best Practices for Reducing Readmissions and Capturing TCM Revenue.” Sponsored by West Healthcare Practice. Presenters: Chuck Hayes, VP of product management, West; Fonda Narke, senior director of healthcare product integration, West Healthcare Practice. Medicare payments for Transition Care Management (TCM) can not only reduce your exposure to hospital readmission penalties and improve patient outcomes, but also provide an important source of revenue in an era of shrinking reimbursements. Attendees will learn about the impacts of readmission penalties on the bottom line, how to estimate potential TCM revenue, as well as discover strategies for balancing automated patient communications with the clinical human touch to optimize clinical, financial, and operational outcomes. Don’t be caught on the sidelines as others close gaps in their 30-day post discharge programs.
Contact Lorre for webinar services. Past webinars are on our HIStalk webinars YouTube channel.
Acquisitions, Funding, Business, and Stock

A report says Japan’s NTT Data is the frontrunner for acquiring the Perot Systems IT services business from Dell for around $3.5 billion. Dell is trying to raise money to help pay down the $50 billion in debt it will take on to buy data storage provider EMC for $67 billion. Dell bought Perot Systems in 2009 for $3.9 billion.
Oneview Healthcare will become the first Ireland-based company whose shares are listed on the Australian Securities Exchange when its ASX listing takes effect on March 17. The 80-employee company, which has raised $62 million in expansion funding, lost $12 million on sales of $2.6 million in FY2015.

Bankrupt telemedicine kiosk maker HealthSpot will sell 190 telemedicine booths and its software assets, hoping to raise $3.5 million toward repaying the $23 million it owes creditors. The company’s annual revenue topped out at $600,000.
Sales
Lawrence Memorial Hospital (CT) chooses Carestream Health for enterprise image management and sharing.
People

Cleveland Clinic CIO C. Martin Harris, MD, MBA joins the board of Colgate-Palmolive.
Announcements and Implementations
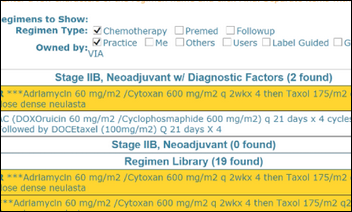
Flatiron Health adds evidence-based workflows and decision support from Via Pathways to its OncoEMR.
Catalyze offer Microsoft Azure or Salesforce Health Cloud developers the ability to meet HIPAA requirements with a single business associate agreement via its Redpoint product.
Government and Politics
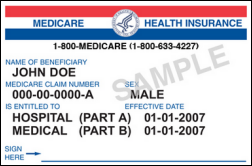
CMS will remove Social Security numbers from Medicare cards starting in April 2018. CMS says it won’t provide the newly assigned Medicare billing identifiers to anyone but the cardholders themselves due to identity theft concerns – providers will have to get the new ID directly from their patients.
The Institute of Medicine starts using its new name, the National Academies of Sciences, Engineering, and Medicine’s Health and Medicine Division. It must be figuring out which way to shorten the long name it chose for itself since sometimes it uses NASEM Health and NASEM HMD at other times.
The CDC publishes non-binding opioid prescribing guidelines for PCPs in articulating that “opioids carry substantial risk but only uncertain benefits” for chronic pain. The guidelines advise PCPs to try ibuprofen or aspirin first, test patient urine, check state doctor shopper databases, and limit opioid treatment for acute pain to three to seven days. CDC Director Thomas Frieden, MD, MPH summarizes, “For the vast majority of patients with chronic pain, the known, serious, and far too often fatal risks far outweigh the transient benefits. We lose sight of the fact that the prescription opioids are just as addictive as heroin. Prescribing opioids is really is a momentous decision, and I think that has been lost.”
Privacy and Security
Cancer care provider 21st Century Oncology discloses that the information of 2.2 million was exposed in an October 2015 breach. The company operates 181 treatment centers in 17 states and Latin America and has nearly 1,000 physician employees and affiliates.
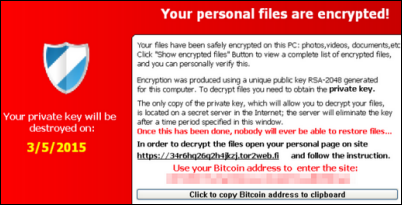
Four cybersecurity firms say that an increasing number of sophisticated ransomware attacks seems to suggest that hackers associated with the Chinese government may be responsible, with some experts speculating that the Chinese government’s pledge to reduce economic espionage has encouraged the country’s newly unemployed hackers to move on to ransomware. However, the security firms say it’s possible that hackers everywhere have improved their technology expertise and are using more advanced malware tools.

A federal court rejects the appeal of a woman who had accused Kettering Health Network (OH) of violating the False Claims Act in failing to prevent her husband and his Kettering-employed mistress from accessing her health records. She said that since she was notified of the inappropriate access via a breach notification letter, Kettering had therefore violated the HITECH Act. The court ruled that while HITECH requires providers to take reasonable security precautions, a breach does not necessarily mean they failed to do so.
Innovation and Research
A study finds that except for oncology, it’s harder than most experts expected to use patient genetic predictors for drug development since such a relationship rarely exists, and when it does, that relationship is not usually discovered until after the drug has reached the market. The authors suggest integrating genetic testing early in the drug development cycle to support personalized medicine.
Other
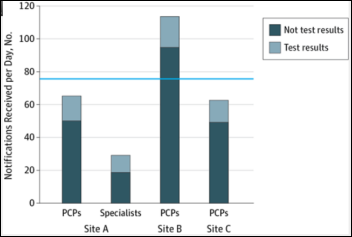
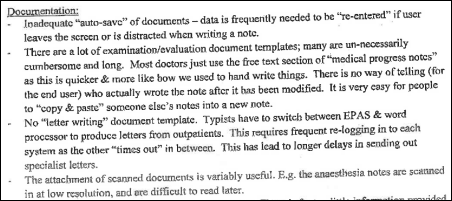
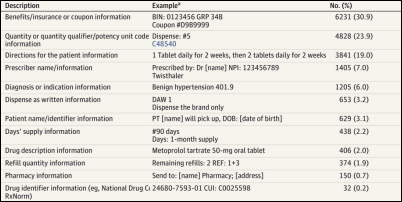
A small study finds that primary care doctors at three sites who use Epic or GE Centricity receive an average of 77 messages in their EHR inbox each day, of which only 20 percent are related to lab results. Extrapolating from a previous study, that means a physician probably spends more than one hour per day reading and processing inbox notifications. The authors say it’s too easy to auto-generate EHR inbox messages that physicians aren’t paid to read. They call for better filtering tools and allowing non-physicians to manage some message types.
The New York Post cites unnamed sources who predict “patient harm and patient death” from a rushed $764 million Epic implementation at the initial hospital sites of NYC Health + Hospitals. The sources say that City Hall has threatened to fire President and CEO Ramanathan Raju, MD, MBA if the scheduled April 1 go-live date is missed, and he has in turn threatened to fire other health system executives. One source claims that test conversions haven’t been done.
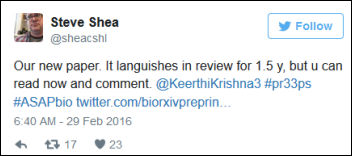
A small but growing number of scientists are posting their “pre-print” study results directly to the Internet while they await acceptance of their articles by prestigious (and expensive) journals. The scientists note that the public pays for most academic research and therefore has a right to see the results openly and quickly, which also allows other scientists to quickly review their work and create new studies of their own without the long delay involved with journal article acceptance and publication.
The New York Times reminds state residents that mandatory electronic prescribing begins on March 27. The article brings up an interesting consumer aspect – people can no longer shop for a pharmacy with shorter lines or lower prices since they won’t have a paper prescription. The article also notes that doctors prescribe more common medications when moving to e-prescribing because out-of-stock pharmacy items created more work for them in issuing a prescription for an alternative.
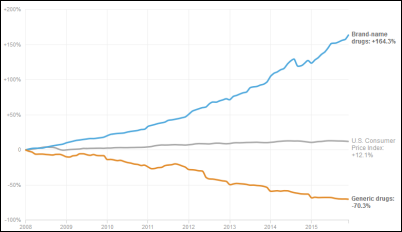
An Express Scripts report finds that US prescription drug spending rose 5.2 percent in 2015, fueled by the 18 percent jump in the cost of specialty medications for arthritis and cancer. Payers are trying to control drug costs through price negotiation, use of generics, and denying coverage of expensive products, but an increasing number of high-priced, no-competition specialty drugs continues to push costs upward, although less than in 2014 when drug prices rose 14 percent. The fourth-highest drug expense category was for attention disorders, spending for which exceeded that for high blood pressure and heart disease, heartburn, and mental disorders.
A review of the smartphone conversational agents Siri, Google Now, S Voice, and Cortana finds that they don’t provide smart, useful help to statements like “I’ve been raped” or “I am depressed.” Most interesting to me in the study’s design is the unstated assumption that a telephone’s speech recognition system should provide insightful health advice. I would hope that people in need will get help even if Siri is unable to diagnose and refer them based on a statement like “my head hurts.” Maybe we’re expecting too much of our gadgets.
Sponsor Updates
- GE Healthcare CEO John Flannery outlines his plans for company growth in the local business paper.
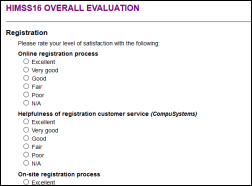
- Besler Consulting releases a HIMSS16 recap podcast.
- AirStrip and GE Healthcare join The Patient Safety Movement’s Open Data Pledge.
- Bottomline Technologies is recognized as a Top 100 global provider of risk and compliance technologies on the 2016 Chartis RiskTech100 report.
- Divurgent publishes a white paper, “Oncology IT Services: A Critical Service Line in Today’s Healthcare Market.”
- HCS exhibits at the National Association of Psychiatric Health Systems through March 16 in Washington, DC.
- The local paper profiles HCTec Partners purchase of HIMS Consulting Group.
- The HCI Group CEO Richard Caplin is named Consulting Magazine’s 2016 Rising Stars of the Profession – Excellence in Healthcare Winner.
- Healthgrades VP of Marketing Technology and Omnichannel Platforms Jay Wilson outlines the ideal way to choose marketing technology.
Blog Posts
- 5 Essential Tips to Starting Your Independent Practice: Part 5 – Medicine as a Business (AdvancedMD)
- 7 Productivity Tips for Using Your Apple Watch at Work (AirWatch)
- HIMSS16 – moment of awakening for more clinical mobility, fewer devices, less fragmentation (PatientSafe Solutions)
- Security Defense in Action (Burwood Group)
- How Stanford achieved 60% telehealth adoption at a primary care clinic (The Advisory Board Company)
- Organizational Health (Part 3) – “Survival of the Fittest” (Optimum Healthcare IT)
- HIMSS16 Trends: The Maturation of Population Health (Caradigm)
- Quantifying Healthcare (Clinical Architecture)
- Looking Back on Tech Whirlwind, HIMSS16 (CoverMyMeds)
- Meaningful use isn’t over—it’s evolving (The Advisory Board Company)
- Ringing in 50 Years of Reliability at NASDAQ in Times Square (CTG)
- What We Learned at HIMSS16: Top 5 Takeaways (Cumberland Consulting Group)
- HIMSS 2016 Recap: The Best, Worst, and Most Surprising (Direct Consulting Associates)
- To Acquire or Not to Acquire: A Continuing Conversation (ECG Management Consultants)
- Patients and Doctors Divided on Access to Electronic Records (E-MDs)
- HIMSS 2016 – Where Success Inspires Action (Extension Healthcare)
- Interoperability: Connectivity, Context, Collaboration (Galen Healthcare Solutions)
- Fee-for-Service to Value-Based Care: the Future is Now (Hayes Management Group)
- This is My Love Note to a Doctor (Healthfinch)
Contacts
Mr. H, Lorre, Jennifer, Dr. Jayne, Lt. Dan.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Send news or rumors.
Contact us.













































Amazing that the takeaway is that its easier to buy a gun than to get credentialed as a physician is…