Zoë Barry is founder and CEO of ZappRx of Boston, MA.

Tell me about yourself and the company.
I founded ZappRx in 2012. I came at it from the patient perspective. My youngest brother was diagnosed with severe epilepsy and couldn’t get on medication for almost a year and a half. This led to him to have a stutter, a learning disability, short-term memory loss, and he couldn’t remember what happened the day before. It was absolutely devastating as a family.
I was working on Wall Street at the time and had some familiarity with what was going on in healthcare technology. I guess you could say I became prescription obsessed. I started diligencing all of the problems with prescriptions, the different types of prescriptions, and tools that could be used to prescribe these medications. Ultimately, I found that there was no real product in the marketplace.
I jumped into founding ZappRx in 2012. I have made it my mission and the company’s mission to make it better, faster, and more transparent for high-risk patients to access lifesaving medications.
Why was such obvious inefficiency overlooked by other companies that might have tackled the problem?
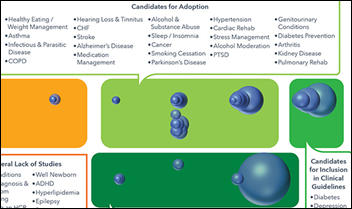
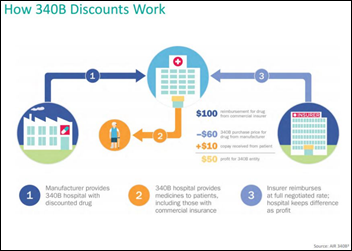
I think it’s because the volume is so low for specialty drugs. When Meaningful Use came out, the first order of priority was to get doctors using EHRs. The second order of priority was to tackle prescriptions. E-prescribing came to the market and focused on the high-volume transactions. If you look at the drug market, there are 3.7 billion prescriptions written annually. E-prescribing focused on the ones that are spent at retail pharmacies that are covered by pharmacy benefit. That’s the bulk of the prescription volume in the United States.
Specialty drugs are only 2 percent of the volume, about 70 million prescriptions total, although they make up about 40 percent of the drug spend. You need a very different software and product that handles specialty prescriptions and you need a very different business model for something that accommodates only 2 percent of the market.
If I had to pick a comparable company, I might say CoverMyMeds, which brilliantly improved clinician efficiency and patient access while getting drug companies to pay for its product. Is is still reasonable to create a business that assumes drug companies will provide revenue?
CoverMyMeds is very smart. My understanding is that they have two customer channels, pharma and payers. Those are the two stakeholders that have skin in the game in terms of getting patients on certain therapies and getting them on as quickly and as efficiently as possible. If you look at the other two stakeholders that are users of CoverMyMeds — doctors and pharmacies — it doesn’t make a lot of sense to have doctors or pharmacies pay for prior authorization. It makes more sense for the pharma companies and the payers to do that.
That’s a great analogy, because we look at it very similarly. Our software connects specialists with specialty pharmacies, but our business model focuses — similar to CoverMyMeds – on pharmaceutical companies and payers.
How do you get your message in front of that small percentage of specialty drug prescribers that your product is good for them, they don’t have to pay for it, and it’s easily implemented?
We raised venture money in order to build the company. I had very little money. Even though obviously it sounds like a lot when you raise a couple of million dollars, it goes really fast. I focused our Series A funding on getting the product right and getting the top key opinion leaders using the product. I focused on a couple of the highest-volume prescribers at the top institutions and I was able to get them on board.
It’s sort of a waterfall effect. You start at the top and those doctors and their staff became incredibly vocal about how amazing our product was, how much time it was saving for the nurses who were managing all of this paperwork, and how much faster patients were getting onto therapy. Therefore, how much healthier the patients were. Even though it was a small subset, those doctors were able to underscore their experience.
We ended up hiring a director of sales to then take those early adopters and go out and seed more of the market. Then something really amazing happened, which we did not expect at all. As more doctors adopted, they started going to pharma ad boards and saying, “I will never want to write a prescription any other way other than via ZappRx ever again.” It’s that huge moment you have to pinch yourself when you’re a founder, you had this crazy vision, and you dropped everything and put all of your time and effort — blood, sweat, and tears — into building a company. When a doctor who is a new user who signed up r on their own says that to a pharma customer, it is just amazing.
We just closed our Series B funding. In our life as a startup, our Series A funding was focused on getting the product right — the right feature set, the technology, and the core partnership. Our Series B is now focused on growth. We’ve hired our own sales team. We’re striking more partnerships. We’re going to grow from that more organic growth to much more at scale nationwide.
Technology companies often mistakenly think that a lack of technology usage in healthcare means it’s an easy target for disruption. What lessons have you learned in trying to breach the healthcare fortress?
It’s definitely hard. I’ve often joked in the startup ecosystem that if you’re going to be a healthcare entrepreneur, you have to raise enough money to not go bankrupt while you’re iterating on your idea and getting that first user. If anyone had told me it would take two and a half years from when I founded ZappRx to getting that first prescription out the door, I would’ve said you’re crazy. But it really did take that long.
Healthcare is reactive, not proactive. The amazing thing is, if you can survive that valley of death and you can get your foot in the door, you can be much stickier. It’s hard to kick you out once you get in. There are pros and cons to that. In the tech ecosystem, if you have a consumer model, it’s much more fickle. You get users really quickly, but you lose them just as fast.
What are the good and bad aspects of finding investors, working with them as mentors, and getting them involved in the company’s decisions?
Not all money is equal shades of green. There are investors that will come in that will add a huge amount of value. They’ll be thought partners with you. They’ll mentor you. They’ll coach you. Our board functions much more as a board that says, where are you blocked? What’s going badly? What’s going wrong? Where are you stalled? How can we help?
We needed to bring in more tech talent and we hired a bunch of engineers out of Google — we just got backed by Google. If it’s iterating on biopharma, we have access through GSK as one of our investors to speak with pretty much anybody on the biopharma side, any disease areas that we want to brainstorm. What’s the pain point? Is our product scaled immediately from pulmonology to rheumatology, or are there some extra features we may add to accommodate a new therapeutic category?
Conversely, a lot of startup companies have some bad experiences with investors that are just not thought partners. They come in only looking for an ROI. They’re investors that will not roll up their sleeves and actually do the work to help a company mature and grow and de-risk. That’s where you start seeing so much of these horror stories in the news or on blogs or companies that seem to be doing really well and then all of a sudden implode.
Some experts say founders shouldn’t dilute their equity by bringing investors in early, but on the other hand, their companies don’t get access to the expertise, contacts, and credibility those investors might bring to the table. If a founder doesn’t want to give equity but instead likes the idea of bootstrapping, what options does he or she have?
I’ve seen that with other companies that are tackling areas of specialty. What they’ve done is a more transaction-based business model. They’ll go out and say, I’m going to solve one small problem. They find the customer that would pay them to solve that problem. They have more of a bootstrapped approach, where they go the customers directly.
There’s pros and cons to that. You can pull in some money, you can pull in a customer, and you can iterate off the product, but you’re also bound by only that perspective of the customer. It’s unlikely that you’ll have a massively disruptive technology or business. It’s more likely that you’ll cover your costs and you’ll solve a small problem. It’s not something that’s going to fundamentally change the way healthcare operates today because you can’t build it agnostically.
We’re agnostic to all drugs. We’re agnostic to all specialty pharmacies. We’re agnostic to all payers. We strive to have all the drugs, all the steps, and every stakeholder connected to ZappRx. If I had taken money only from pharma early on, then I would be perhaps at odds with other pharma companies that compete in the same space, or other stakeholders that have competing interests to biopharma.
How does a first-time entrepreneur with a cool idea decide whether to just slowly build a stable, profitable business versus rolling the dice by taking investor money and thus being pushed to either succeed or fail quickly?
There are a couple of things, and they may not be immediately obvious. One of them is that you have to be in an environment where you have access to capital that is a thought partner. There are reasons there are hotbeds where startups are birthing these incredibly disruptive technology plays, whatever industry it is. Those typically tend to be Boston, San Francisco, and New York. There are other areas of innovation that are spawning throughout the country.
But if you’re in some small area in the backwaters of Florida, it’s probably unlikely that you’re going to be able to build a very disruptive play and think outside of the box. You just won’t have access to the intellectual capital that you need to think differently. You’re going to be more likely to surround yourself with people who are thinking, I don’t have a lot of money. I don’t have a huge nest egg or savings. I don’t have access to angel investors who can even just help me cover legal bills to incorporate the company, so I’d better find a customer really fast. That’s where you wind up with the bootstrapped mentality. Which, by the way, there’s always a place for every type of company.
You’ve said that accelerators are a farce. Why do you think that?
I did not go through any accelerators or incubators. I did one program that was remote coaching and focused on women, which is something I’m very passionate about enabling. That program is called Springboard and they did it very well.
I have a vendetta against these incubators that are only three or four months long. They take 7 percent equity as the typical amount for three to four months of “coaching.” Let me tell you, there is nothing that happens in three to four months that is worth 7 percent equity in a company. You just cannot change that much. Usually the grant that they give you is $100,000. You have to be a three- or four-person team to even apply. You’re not at ideation stage. It’s just unrealistic, and candidly, greedy.
Furthermore, I believe that there are a lot of entrepreneurs who have to go through the experience of building the company. Accelerators often enable entrepreneurs who can’t. They take these premiums and then they spew out some mediocre ideas that suck up the capital or bandwidth for companies that have true potential.
Everybody and his brother runs an accelerator or incubator and has to fill their classes. Does that encourage questionable startups to think they’ll be successful just because they got in?
I would agree with that. There’s a reality that some startups aren’t aware of yet. If you go into an accelerator or an incubator, you get to demo day, and you wind up with no term sheets afterward, you are screwed. Because other investors are going to look at that and say, wow, you got into one of these fancy accelerator incubators. You sent us the investor weekly update. You’ve been sharing all this progress that you were supposedly making — which was really probably just a distraction — and now all the investors that I look to to make qualified decisions have passed on this investment. What are they seeing that I don’t see? Obviously I’m not going to invest also. Then your startup is dead.
I know several companies that went through that. They were not well-structured accelerators. It wound up being a three- to four-month distraction. Nobody gave them a term sheet. It was the kiss of death. They couldn’t raise money after that. They would have been so much better off just bootstrapping themselves or tinkering themselves and getting some of their own angel money for three to four months, focusing on where they were seeing traction and validation in the marketplace and then eventually raising money from an investor versus this silly accelerator.
Successful startups have to figure out what’s next, trying to balance board member interest or maybe even replacing the passionate founder with someone who has experience taking companies to the next level. How do you see growth changing ZappRx?
We focused initially on growing up. The lowest-hanging fruit was some of the most critical, focusing on culture and what your values are. We had been in a WeWork for the last two years. It’s one of these Uber or Airbnb type multi-billion dollar value cap companies. They take over office buildings and turn them into co-working spaces. A company can get one office, they can get 10 offices. We had a third of a floor at one of their locations. It enables you as a small company to have only a month-to-month lease. You can grow or shrink the number of offices as your company grows or shrinks, like happens in startup land.
They have conference rooms, kitchens, and all this stuff. You get to appear as though you are much further along than maybe you actually are. You have a doorman, more security, sign in, all of that stuff. It’s a lot of fun. They play music in the kitchen and they have kegs on every floor, ping pong tables, and all that startupy stuff. It’ great when you’re in ideation phase. You’re working crazy long hours, you’re throwing stuff at the wall and seeing what sticks, you’re pivoting, and you’re iterating. You need that fun, happy-go-lucky mindset.
But then once something sticks, you need to very quickly transition into focus and execution. I’m going to wash, rinse, and repeat. I am going to be laser-focused on making this the best that it possibly can be. Product, customer experience, pulling in the revenues, etc.
We moved offices and now have our own office, our own culture, and it’s 9,000 square feet. We’re really proud of it. Still legitimate security and all of that. But that’s where the maturation process starts. People are laser-focused and they’re not throwing ideas at the wall and iterating. They’re now tweaking and refining. You put your head down and you march forward. Your investors can sense that, too. They know when you’re in ideation phase — when it’s hopes and dreams — and they know when you’re in execution phase. They will come with you.
There are lots of growing pains. There are people who don’t make that transition. There are early-stage people, mid-stage people, and late-stage people. Every time I raise money, I look in the mirror and say, are you still fit to be CEO? I am the second-largest shareholder in the company after our largest investor, so I have the most incentive to either do well or find someone else who can do better than me. So far as the CEO of the company, I’ve done very well in that role, executing beyond what we’ve set out to do. We set some lofty goals and it’s kind of crazy to look back on that, but I haven’t done it alone. I’ve hired an amazing team. I’ve been working with a CEO coach. I work with my board. I have a whole group of mentors. I have outside resources, like a CEO group,that I lean on. But I focus on it a lot. When I do that, I see my team doing it as well.
Do you have any final thoughts?
Something that doesn’t get highlighted a lot that I’m really, really proud of is our gender balance at ZappRx and how many women leaders we have on the team. We are 50 percent women, which for tech companies in general is an astounding statistic. Even if you look forward at where I hope we’re growing — which is the Fortune 500 list — there are not a lot of women CEOs or management teams that are a chock-full of women. So I’m really proud to be 50 percent women. I mentioned that we are executing above and beyond. I think there’s something to do with that having a gender-balanced team, and a very diverse team at that.

























































































I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…