Access EForms

Booth 3071
Contact: Cody Strate, VP of marketing
cody.strate@accessefm.com
603.205.3479
Access EForms converts frustrating, paper-based forms into Epic/Cerner/Meditech-integrated and tablet-enabled EForms that patients electronically sign. We’re a Meditech partner, and our technology powers Cerner’s new “Cerner Forms Suite.” At HIMSS, we will put a particular focus on the paper-based informed consent problem that causes expensive delays/cancellations in the OR, frustrates the surgical team, and makes for a very poor patient experience. Our paperless, EHR-integrated Informed Consent solution feels like an inherent part of your clinician’s EHR experience, which promotes user adoption. In the end, we eliminate the paper, we reduce OR delays and cancellations, we improve the lives of the surgical team, and we improve the patient experience. Stop by booth 3071 and we’ll show you what’s possible with eliminating your difficult, paper-based processes.
Agfa Healthcare

Booth 3745
Contact: Miriam Ladin, director, marketing and communications – North America
miriam.ladin@agfa.com
617.852.4545
We at Agfa HealthCare believe that the ability to optimize resources through a consolidated imaging management platform will become a competitive advantage for our clients. The CIO and IT functions typically support as many as 70 distinct service lines that capture and consume medical imaging. Learn how to reduce complexity with a converged single platform technology and bring order and value to these disparate systems, workflows, and behaviors across the enterprise. We believe that consolidated clinical alignment will better enable high-impact, data-driven, cost-conscious care, compared to the complexity of maintaining multiple and redundant systems.
Visit Agfa HealthCare to discuss how to create a controlled environment for managing and sharing images, including a secure, single sign-on framework that provides context-controlled and audited access to data. The genuine, standards-based consolidation platform facilitates security hardening, thus reducing multiple points of security failure. Single platform technology arguably enables your team to guard fewer gates. Enterprise imaging enables accurate attribution of metadata to episodes of care, providing actionable information and a trail of documentation for use in revenue and risk mitigation gains. With patient safety in the forefront of quality care delivery, easy access to secure and accurate patient data becomes a necessity to clinical and fiscal excellence. Support busy clinicians with clinical confidence in the records they view and drive both their productivity and satisfaction.
Learn how to reduce complexity and TCO while you enjoy the virtual reality (VR) video experience in our Virtual Reality Lounge. Enter to win your own Oculus VR headset in booth 3745.
Black Book Market Research

To arrange a meeting, contact Doug Brown.
Contact: Doug Brown, president
doug.brown@blackbookmarketresearch.com
727.463.7806
Bluetree

Booth 2487
Contact: Ryan Hill, marketing manager
rhill@bluetreenetwork.com
651.380.3713
Bluetree was named the top-ranked Epic Systems Strategy, Support, & Implementations firm according to Black Book Market Research in August 2019. If you visit Bluetree’s booth this year and fill out a leaf, the National Forest Foundation will plant one tree in your name or your organization’s name. One daily grand prize winner will receive 100 trees planted in their name.
Bright.md

To arrange a meeting, contact Ray Costantini.
Contact: Ray Costantini, CEO and co-founder
ray@bright.md
Founded in 2014 and based in Portland, OR, Bright.md is a leading healthcare automation company dedicated to modernizing direct-to-patient telehealth for healthcare systems with its AI-powered virtual-care platform, SmartExam. Bright.md partners with premier healthcare organizations in North America, including three of the top five not-for-profit health systems in the United States. These partners offer SmartExam to more than 10 million patients who are seeking convenient urgent and primary care online. Bright.md has been named the Leader in the “Forrester New Wave: Virtual Care Solutions for Digital Health” report, a Gartner Cool Vendor in Healthcare, a Vendor to Watch by Chilmark Research, and is the preferred choice of Avia’s Virtual Access cohort. Bright.md is venture-backed by B Capital Group, Seven Peaks Ventures, Pritzker Group Venture Capital, Oregon Venture Fund, and the Stanford-StartX Fund. For more information, visit Bright.md.
Capsule Technologies

Booth 2441
Contact: Sam Larson, head of global marketing
slarson@capsuletech.com
475.223.6174
Capsule continues ‘making the complex simple and the simple insightful.’ Whether you’re considering unlocking the power of medical device data to automate clinical documentation workflows in critical care for the first time, interested in simplifying patient vitals acquisition and utilization for overloaded med-surg staff, or investigating ways to identify at-risk patients sooner hospital-wide, we can help you make change happen. Stop by our booth and speak directly with a representative to find out how our new Capsule Medical Device Information Platform can make the complex simple and simple insightful for your facility. The Capsule Medical Device Information Platform captures and contextualizes clinical data, providing real-time patient information that can facilitate early intervention and enable better clinical outcomes.
CareSignal

Booth 8200, kiosk 8200-45 and Booth 680, kiosk 680-09
Contact: Jason Roche, director, marketing
jason.roche@caresignal.health
314.272.2586
With 10 peer-reviewed publications, CareSignal is an evidence-based, remote patient monitoring platform without the headache of devices or apps. Standardized, automated text messages scale patient engagement and monitoring, collecting real-time patient-reported health data to prioritize patient intervention.
We will be raffling off hundreds of dollars worth of Visa gift cards each day for those who visit the booth and complete the demo.
CareSignal will co-host a CIO Reception Monday, March 9 from 5-7pm at Urban Tide in the Hyatt Regency Orlando. RSVP here.
The Chartis Group

To arrange a meeting, contact Gregg Mohrmann.
Contact: Gregg Mohrmann, director and Informatics & Technology Practice co-leader
chartis@chartis.com
877.667.4700
Chartis provides comprehensive advisory services and analytics to the healthcare industry. With an unparalleled depth of expertise in strategic planning, performance excellence, informatics and technology, and health analytics, Chartis helps leading healthcare organizations achieve transformative results. Connect with us at HIMSS to learn about some of the results our clients have achieved in these, among other, areas:
- Using technology-enabled innovation to unlock new potential and accelerate digital transformation.
- Using ERP to improve margin, cost, satisfaction, and differentiation.
- Harnessing the power of data and analytics.
- Leveraging the EHR to improve cost, quality, outcomes, and satisfaction.
- Ensuring IT, as a strategic partner, delivers high impact and high value.
CI Security

Booth 413
Contact: Vivian Zhou, healthcare program director
vivian.zhou@ci.security
206.620.0277
CI Security protects and defends healthcare organizations from cyber threats with HIPAA-compliant Managed Detection and Response solutions and expert consulting services. CI Security was founded by the CISO of a major city and a co-author of the HIPAA Security Rule because they saw a need for cybersecurity solutions built to protect and defend critical services, patient care, and protected data. Ten years later, CI Security is the MDR leader proven in healthcare, and has been recognized in Gartner Research’s Guide for Managed Detection and Response Services in 2018 and 2019. Hospitals and clinics trust CI Security to monitor networks 24/7, protect patient care and EPHI, and manage risk in a rapidly evolving cyber threat landscape. Find out more at https://ci.security.
Clinical Architecture

Booth 1629
Contact: John Wilkinson, EVP, sales and partnerships
john_wilkinson@clinicalarchitecture.com
317.580.8417
Clinical Architecture was founded in 2007 by industry veterans, clinicians, and informatics experts to deliver innovative solutions that maximize the effectiveness of healthcare. We work with industry-leading organizations, four of the top five health systems, leading EHR/HIE vendors, the Joint Commission, the CDC, and others to solve challenges around healthcare data quality, interoperability, and clinical documentation. Visit our booth (1629) to find out who the Informonster is, pose for a picture with him, and grab a stuffed version of the Informonster to take home with you.
CloudWave

Booth 1021
Contact: Bryan Blood, EVP, sales
bblood@gocloudwave.com
877.991.1991
CloudWave is the healthcare cloud transformation company. We create solutions that embrace the full cloud continuum – from the Cloud Edge, to managed private cloud services in our OpSus Healthcare Cloud, to seamless federation with public cloud services. CloudWave’s focused portfolio of OpSus Healthcare Cloud services includes hosting over 100 healthcare applications, disaster recovery, systems management, security, backup, and archiving services. CloudWave architects healthcare IT solutions with the goal of operational sustainability. Our engineers and consultants have long-standing, successful track records designing and implementing solutions for hospitals. For more information, please visit www.gocloudwave.com.
Collective Medical

Booth 8200-31
Contact: Wayne Grodsky, chief revenue officer
wayne.grodsky@collectivemedical.com
215.287.990
Collective Medical empowers care teams to improve patient outcomes by closing the communication gaps that undermine patient care. With a nationwide network engaged with every national health plan in the country, hundreds of hospitals and health systems, and tens of thousands of providers, Collective’s system-agnostic platform is trusted by care teams to identify at-risk and complex patients and facilitate actionable collaboration to make better care decisions and improve outcomes. Based in Salt Lake City, Collective is proven to streamline transitions of care, improve coordination across diverse care teams, and reduce medically unnecessary hospital admissions. Learn more at www.collectivemedical.com.
CompuGroup Medical

To arrange a meeting, contact Tillmann Schwabe.
Contact: Tillmann Schwabe, VP of sales, CGM US
tillmann.schwabe@cgm.com
480.440.6516
CompuGroup Medical is one of the leading e-health companies in the world. With a revenue base of approximately EUR 717 million in 2018, its software products are designed to support all medical and organizational activities in doctors’ offices, pharmacies, laboratories, and hospitals. Its information services for all parties involved in the healthcare system and its Web-based personal health records contribute toward safer and more efficient healthcare. CompuGroup Medical’s services are based on a unique customer base of more than 1 million health professionals including doctors, dentists, pharmacists, and other service providers in inpatient and outpatient facilities. With locations in 19 countries and products in 56 countries worldwide, CompuGroup Medical is the e-health company with one of the highest coverage among e-health service providers. More than 5,500 highly qualified employees support customers with innovative solutions for the steadily growing demands of the healthcare system. For more information, please visit www.cgm.com.
ConnectiveRx

Booth 7950
Contact: Mark Mosebrook, senior director, EHR business development
marketing@connectiverx.com
908.809.6100
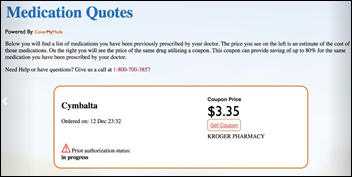
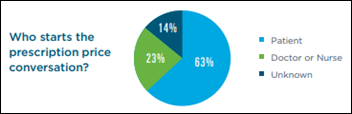
Leading technology-enabled pharmaceutical services company that simplifies how patients get on and stay on complex medications. We work with biopharmaceutical manufacturers, EHRs, pharmacy systems, and others to help patients afford medications, increase adherence, and simplify the patient-provider experience. We do this by leveraging our technology-enabled services to accelerate speed-to-therapy, and by expertly navigating the complexities in accessing innovative therapies and improving outcomes. Based on our experience pioneering co-pay programs, managing awareness/adherence communications, and establishing a state-of-the-art hub service, we help customers overcome barriers to access and use so patients can experience better health. Visit us at booth 7950 to learn how we touch each critical stage of the patient journey.
Culbert Healthcare Solutions

To arrange a meeting, contact Brad Boyd.
Contact: Brad Boyd, president
bboyd@culberthealth.com
857.919.2003
Culbert Healthcare Solutions provides high-value, professional services focused on improving clinical, operational, and revenue cycle performance and the overall patient experience. Our experienced healthcare professionals help group practices and hospitals optimize technology and navigate the change-management process. For more information about Culbert Healthcare Solutions, visit www.culberthealth.com.
Cumberland Consulting Group

To arrange a meeting, contact Praneet Nirmul.
Contact: Praneet Nirmul, partner
praneet.nirmul@cumberlandcg.com
917.214.0975
Cumberland is a leading healthcare consulting and services firm providing strategic advisory consulting services, IT professional services, and outsourced managed services to clients in the payer, provider, and life sciences markets. We deliver solutions that advance the business of healthcare. Our comprehensive suite of services includes:
- Advisory and IT strategy.
- System selection.
- M&A support.
- Systems implementation.
- Systems optimization and upgrades.
- Application service desk.
- Advanced maintenance support.
- Advanced application support.
- IT service desk.
- Legacy systems support.
For more information on Cumberland, visit www.cumberlandcg.com.
Diameter Health

Booth 7461
Contact: Tom Gaither, VP of marketing
tgaither@diameterhealth.com
781.249.9475
Diameter Health identifies and fixes systemic clinical data quality issues so you can put clinical data to work to improve care and lower costs. Diameter Health automatically turns clinical information into a structured, clinical data asset optimized for use in downstream applications. Built on a foundation of hundreds of millions of patient records, deep clinical expertise, and adherence to national standards, our scalable, API-driven technology is the critical success factor for clinical data integration. Diameter Health will be part of a use case demonstration in the Da Vinci booth, 7972. Diameter Health President and Chief Strategy Officer John D’Amore and Health Current CIO Keith Parker will present “How to Tame Your Data Dragon: A Statewide Approach” on Wednesday, March 11, from 10–11am. Visit Diameter Health’s website and check out our video testimonials.
Direct Recruiters

To arrange a meeting, contact Frank Myeroff.
Contact: Frank Myeroff, managing partner
fmyeroff@directrecruiters.com
440.996.0051
For over 37 years, Direct Recruiters has been recognized as the relationship-focused search firm that assists top-tier organizations with recruiting, acquiring, and retaining high-impact talent for mission-critical positions. Direct Recruiters services clients across North America and has years of experience placing candidates internationally. What does relationship-focused mean to us? We get to know you, we have in-depth knowledge of your industry, and we understand our candidates, helping you make the right decisions that will positively impact your organization.
Ellkay

Booth 4071
Contact: Auna Emery, director of marketing communications
auna.emery@ellkay.com
520.481.2862
As a nationwide leader in healthcare connectivity, Ellkay has been committed to enabling interoperability for more than 15 years. With connectivity to over 50,000 practices across over 700 EHR/PM systems, Ellkay builds the data pipeline for hospitals, health systems, practices, EHR/PM systems, laboratories, payers, HIEs, ACOs, and other healthcare organizations. At HIMSS, Ellkay will demonstrate its innovative connectivity solutions. Ellkay is hosting happy hour at its booth, 4071, on Tuesday and Wednesday from 4-6pm.
Engage

Booth 1585
Contact: Rich Robinson, director of marketing
rich.robinson@thinkengage.com
509.230.8763
With more than 20 years of experience solving the most complex IT challenges, Engage is an innovative IT services and consulting company with exceptional expertise in Meditech Expanse and other supporting technologies. With a unique IT delivery model, Engage has a proven history of delivering projects on time and within budget. Engage provides EHR and ERP implementation and optimization, support, cloud-hosting services (private, public, and hybrid) and consulting to more than 170 hospitals and clinics across the US. By developing long-term relationships, Engage helps customers achieve impressively high EHR adoption and satisfaction rates, along with reduced risks and total cost of ownership. Visit www.thinkengage.com for more information. Visit us at booth 1585. Also, stop by our Bourbon Tasting with Pure Storage Tuesday and Wednesday from 3-5pm at booth 1529.
Ettain Group

To arrange a meeting, contact Dawn Wasson.
Contact: Dawn Wasson, senior marketing and communications manager
dwasson@ettaingroup.com
704.719.2796
Ettain group is the talent solutions company that delivers recruitment solutions and managed solutions in five practice areas – technology, healthcare IT, digital, professional, and government. Ettain health, a division of Ettain group, is led by business, technology, and clinical experts with deep expertise to support our customers in selecting, implementing, and optimizing their IT investments. We are committed to providing customized solutions and connecting talent to meet the critical needs of healthcare customers nationwide. With expertise across Epic, Cerner, Meditech (certified Meditech Expanse consulting firm), and other majors EHRs, Ettain health is the partner you can trust to provide expertise and deliver and manage top talent across the full spectrum of healthcare IT projects.
First Databank

Booth 2559
Contact: David Manin, senior director of marketing
dmanin@fdbhealth.com
650.872.4588
FDB is the leading provider of drug and medical device knowledge that helps healthcare professionals make precise decisions. With thousands of customers worldwide, FDB enables our information system developer partners to deliver valuable, useful, and differentiated solutions. We offer more than four decades of experience in transforming medical knowledge into actionable, targeted, and effective solutions that help improve patient safety, operational efficiency, and healthcare outcomes. For a complete look at our solutions and services, please visit www.fdbhealth.com.
HIMSS Highlights:
- FDB CDS Analytics – Introducing a new solution to evaluate and improve the efficacy of clinical decision support for meds and beyond.
- FDB Specialty Pharmacy Module – Interactive scripts – Coming in 2020 to Epic’s Coordinated Care Management.
- Lehigh Valley Health Network Case Study – LVHN successfully leverages hyperkalemia and pharmacogenomics-related decision support content in FDB Targeted Medication Warnings.
- Session: Friday, March 13 at 10:45am in room W300.
- Meducation Receives Cerner Award – FDB’s SMART on FHIR app wins Cerner Open Developer Experience (code) Program Member Adoption Award.
- FDB Drug Info Now in Amazon Alexa – Drug information authored specifically for Alexa now provides answers to consumers’ medication questions.
- Wine Reception and $1,000 Amazon Gift Card Raffle – Join us for a glass of wine and a chance to win $1,000 Wednesday, March 11, from 4:30-6pm in booth 2559.
Get-to-Market Health

To arrange a meeting, contact Steve Shihadeh.
Contact: Steve Shihadeh, CEO and founder
steve@gettomarkethealth.net
Get-to-Market Health is a specialized consultancy focused exclusively on accelerating sales and driving revenue growth for our healthcare technology clients. We work with business leaders to simplify the complexity and unique buying patterns of the healthcare technology market. We help our clients overcome the challenges they face as they work to drive revenue and market innovation. We bring deep, broad experience and valuable network connections across multiple levels of the healthcare technology industry. The partners at Get-to-Market Health are industry experts, having worked at and with dozens of healthcare technology businesses ranging from small startups to large, established companies. We’ve helped private, seed stage, VC-backed, PE-owned, and public companies develop successful teams in all major commercial disciplines.
HBI Solutions

To arrange a meeting, contact Laura Kanov.
Contact: Laura Kanov, SVP, product strategy
lkanov@hbisolutions.com
615.392.5201
HBI Solutions, a precision health analytics company, provides machine learning as a service to better predict, prevent, and personalize treatment before a condition becomes acute, chronic, and costly. Additionally, our acute surveillance and transition risk solutions help hospitals and health systems identify and mitigate event and utilization risk to reduce costs and improve outcomes. Come visit us in the InterSystems booth, 3301.
The HCI Group

Booth 4467
Contact: Chris Parry, VP of business and talent development
chris.parry@thehcigroup.com
904.239.4670
The HCI Group is a global leader in healthcare digital transformation. We are committed to improving healthcare globally through a combination of disruptive innovation, design thinking, and cost optimization. HCI offers a broad scope of digital transformation solutions in nearly 20 countries in North America, Europe, the Middle East, and Asia Pacific. Join us on Tuesday and Wednesday at 11am and 3:30pm at booth 4467 for insightful and practical 20-minute talks with Ed Marx. He’ll share a digital transformation model with expert guests who have helped cross-industry organizations around the globe with world-class human-centered and physical design.
HCTec

To arrange a meeting, contact Brenna Davis.
Contact: Brenna Davis, marketing manager
bdavis@hctec.com
615.786.0733
HCTec is the trusted partner to more than 250 hospitals and healthcare systems across the US for highly specialized health IT staffing, project-based consulting, and application managed services support. With HCTec’s HIT solutions, hospitals are able to reduce operating costs, improve quality, and optimize labor forces.
Health Catalyst

Booth 2428
Contact: Sarah Stokes, marketing director, events
sarah.stokes@healthcatalyst.com
801.634.6287
Health Catalyst is a next-generation data, analytics, and decision-support company committed to achieving massive, sustained improvements in healthcare outcomes. We are the leaders in a new era of advanced predictive analytics for population health and value-based care with a suite of machine learning-driven solutions, decades of outcomes-improvement expertise, and an unparalleled ability to unleash and integrate data from across the healthcare ecosystem. Visit us at booth 2428 to see how the Health Catalyst Data Operating System (DOS) — a next-generation data warehouse and application development platform powered by data from more than 100 million patients and encompassing over 1 trillion facts — can help improve your organization’s quality, add efficiency, and lower costs.
Healthcare Growth Partners

Booth 4490
Contact: Christopher McCord, managing director
chris@hgp.com
713.955.7935
Healthcare Growth Partners (HGP) is an exceptionally experienced investment banking and strategic advisory firm exclusively focused on the transformational health IT market. We unlock value for our clients through our Sell-Side Advisory, Buy-Side Advisory, Capital Advisory, and Pre-Transaction Growth Strategy services, functioning as the exclusive investment banking advisor to over 100 health IT transactions representing over $2 billion in value since 2007. With our focus, we deliver knowledgeable, honest, and customized guidance to select clients looking to execute high-value health IT, health information services, and digital health transactions.
Healthfinch

Booth 2079
Contact: Dawn Burke, director of marketing
dawn@healthfinch.com
608.561.1844 x17
Healthfinch develops Charlie, the healthcare industry’s most trusted, most used prescription renewal delegation engine. Charlie’s unique combination of EHR-integrated technology and protocol content enables health systems across the country to deliver a better, safer patient experience while also achieving lower rates of provider burnout, improved quality metrics, and significant time and cost savings. Learn more at healthfinch.com or at booth 2079.
Stop by anytime during exhibit hall hours to see a demo and get a “Charlie the Healthfinch” plush! Healthfinch will also host an in-booth happy hour at booth 2079 on Tuesday, March 10 from 4-6pm. RSVP for the happy hour here.
Healthwise

Booth 2533
Contact: Jim Watkins, VP
jwatkins@healthwise.org
208.387.6774
Healthwise has set the standard for patient education since 1975. Nonprofit and independent, we’re a trusted resource for health content, technology, and services. Discover new ways to connect with your patients and save your clinicians time. Stop by booth 2533 to learn how.
- Explore new longitudinal programs that digitally connect patients with education resources for critical health interactions, saving care teams time and strengthening patient engagement.
- See how savvy healthcare marketers are using plug-and-play health education to create rich digital experiences for patients in less than half the time it used to take.
- Preview how industry-leading medical illustrators are using 3-D animation to bring medical concepts to life in a way that’s engaging and easy to understand.
Hyland Healthcare

Booth 2759
Contact: Megan Phelps, global programs manager
meghan.phelps@hyland.com
913.343.1305
Hyland Healthcare provides connected healthcare solutions that harness unstructured content from all corners of the enterprise and link it to core clinical and business applications such as EHRs and ERP systems. Hyland Healthcare offers a full suite of content services and enterprise imaging solutions, bringing documents, medical images, and other clinically rich data to the healthcare stakeholders that need it most. This comprehensive view of patient information accelerates business processes, streamlines clinical workflows, and improves clinical decision making.
Join us for daily happy hours in our booth from 5-6pm on Tuesday and Wednesday, and from 3-4 pm on Thursday. Enter our drawing for a chance to win Apple AirPods.
Impact Advisors

To arrange a meeting, contact Keith MacDonald.
Contact: Keith MacDonald, VP and client relationship executive
keith.macdonald@impact-advisors.com
617.935.9320
Impact Advisors is a nationally-recognized healthcare consulting firm that is solving some of the toughest challenges in the industry by delivering strategic advisory, technology implementation, and performance-improvement services. Our comprehensive suite of digital health, clinical optimization, and revenue cycle services spans the lifecycle of our clients’ needs. Our experienced team has a powerful combination of clinical, revenue, operations, consulting, and IT experience. The firm has earned a number of prestigious industry and workplace awards, including Best in KLAS for 12 consecutive years; Healthcare Informatics HCI 100; Crain’s Chicago Business Fast Fifty; as well as “Best Place to Work” awards from: Modern Healthcare, Consulting Magazine, Becker’s Hospital Review, and Achievers. For more information about Impact Advisors, visit www.impact-advisors.com.
Legacy Data Access

Booth 1473
Contact: John Hanggi, director, business development
jhanggi@legacydataaccess.com
678.701.5589
Running old applications just to get to the data? STOP – We need to talk! For organizations retiring or replacing healthcare systems, Legacy Data Access offers the industry’s most comprehensive set of software tools and solutions for working with data from retired systems. Our solutions provide comprehensive functionality for the storage, access, management, and reporting of retired healthcare data. No time-consuming, labor-intensive, and risk-filled data conversions are required. The data is seamlessly accessible in its original format, with no loss of detail or integrity. Please visit us to discuss how we have successfully retired 304 different healthcare applications – a total of 863 applications.
Giveaways include key chains and the best dark chocolate in the exhibit hall. Drop a card for a chance to win one of three AirPod Pros.
Medhost

Booth 2131
Contact: Brian Grant, senior director, marketing
Brian.Grant@medhost.com
Medhost has been providing products and services to healthcare facilities of all types and sizes for over 35 years. Today, more than 1,000 healthcare facilities nationwide partner with Medhost and are enhancing their patient care and operational excellence with its clinical and financial solutions including an integrated EHR. Additionally, its unparalleled support and hosting solutions make it easy for healthcare facilities to focus on what’s important – their patients and business.
At HIMSS 2020, Medhost will showcase its comprehensive and cloud-based technology solutions that include but are not limited to EHR, EDIS, general financials and revenue cycle solutions and services, patient engagement, and ambulatory integration solutions.
Giveaway: Thought Leaders Wanted! Visit Medhost at booth 2131 and record a podcast with us. For each podcast recorded, we will give away a $25 gift card. Sign up for a 15- to 25-minute slot today and share you expertise about HIT and the healthcare environment in a guided interview.
NextGate

Booth 3128
Contact: Stephanie Fraser, director of communications and media relations
stephanie.fraser@nextgate.com
734.233.1483
NextGate is the global leader in healthcare identity management. With over 250 customers in five countries, our solutions are deployed at the world’s most successful organizations and HIEs. NextGate will have two exciting in-booth events this year:
- Whisky Tasting on Tuesday, March 10 at 4:30pm: Join Whisky Librarian Dr. Nick van Terheyden for a four-flight whisky tasting as he takes us through an introduction of Scotch Whisky Regional Styles. Register to secure a Glencairn whisky glass (first 50 people). We will also raffle off a bottle of whisky and a whisky dictionary.
- Let’s Talk About a National Patient Identifier on Wednesday, March 11 at 1pm: Join our expert panelists Ben Moscovitch, Pew Charitable Trusts; Julie Dooling, AHIMA; and policy wonk Mark Segal for an engaging discussion on patient matching and universal patient identifiers.
Stop by our booth to enter for a chance to win two backpack giveaways filled with a hoodie and $50 Amazon card, or pre-register for our whisky tasting for a Glencairn whisky glass and a chance to win a bottle of Scottish whisky.
Nordic

Booth 2879
Contact: Samantha Tiller-Schenck, experiential marketing manager
samantha.tiller-schenck@nordicwi.com
513.746.0398
Healthcare organizations are challenged to deliver higher quality care at a lower cost. Our award-winning team provides health IT staffing, advisory consulting, and managed services that result in a stronger business with better patient outcomes. Stop by for open and direct conversations, meet new CEO Jim Costanzo, and learn how Nordic has evolved to better serve you. If that’s not enough, we’ll also have a custom tea blend gift that may help calm the common stresses of HIMSS.
Obix by Clinical Computer Systems
Booth 7273 and 8300
Contact: John Murray, key accounts manager
john.murray@obix.com
224.856.3459
Embracing Mothers and Babies Throughout Birth – The Obix system is a clinician-focused software solution supporting integration, compliance, communication, and patient care. The clinical decision-support features and tools promote critical thinking by reinforcing experience and knowledge. Tour a smart hospital where the Obix system is monitoring a patient in the Labor and Delivery room, inside the Intelligent Health Pavilion. Also at HIMSS, Obix and Epic will demonstrate the exchange of data in real time in the Interoperability Showcase’s Maternal and Newborn Health use case.
OptimizeRx

Booth 8300-29
Contact: Maira Alejandra, media relations manager
malejandra@optimizerx.com
OptimizeRx is a digital health technology company, connecting life sciences, payers, providers, and patients using the largest point-of-care communications platform and disease-specific digital health frameworks. The cloud-based solutions support affordability and adherence efforts directly within the provider workflow, as well as after the patient leaves the care setting, providing a true omni-channel treatment experience and advancing positive outcomes. Come see us in action at the Interoperability Showcase.
Optimum Healthcare IT

To arrange a meeting, contact Larry Kaiser.
Contact: Larry Kaiser, VP, marketing and communications
lkaiser@optimumhit.com
516.978.5487
Optimum Healthcare IT has a dedicated meeting space (MP122). If you are interested in learning how our services can help your organization meet its healthcare IT needs, please visit www.optimumhit.com/contact and contact us today!
PatientKeeper

Booth 2006
Contact: Cristina Christy, senior events manager
cchristy@patientkeeper.com
781.373.6378
PatientKeeper’s EHR optimization software solutions streamline physician workflow, improve care team collaboration, and fill functional gaps in existing hospital EHR systems. With PatientKeeper as the “system of engagement” complementing the EHR, physicians can easily access and act on all their patient information from PCs, smartphones, and tablets. At HIMSS20, visitors can see demos of the complete range of PatientKeeper’s physician workflow applications, as well as the new Clinical Communications Suite, which enables care team members to securely communicate anytime, anywhere, through HIPAA-compliant messaging with embedded patient context. PatientKeeper is used by more than 70,000 physicians at hospitals and health systems across North America.
HIMSS giveaway: PatientKeeper will raffle off one Apple Watch each day to a qualified visitor who watches a demo at booth 2006.
PCare

Booth 3721
Contact: Bob Abrahamson, VP, marketing
rabrahamson@p-care.com
267.614.5214
PCare’s interactive patient engagement solution helps healthcare providers educate and collaborate with patients across the care continuum. The PCare open platform integrates with existing EHR systems, patient portals, and mobile health applications to connect patients and caregivers. PCare is the partner healthcare organizations trust to improve care quality, patient outcomes, and financial performance.
Visit PCare at the Spectrum Enterprise “Powering Innovations Across the Continuum of Care” booth, 3721, to learn about the PCare approach to patient engagement across the continuum for value-based organizations.
PerfectServe

Booth 4346
Contact: Guillaume Castel, CEO
gcastel@perfectserve.net
866.844.5484
PerfectServe’s unified platform for clinical communication and collaboration helps physicians, nurses, and care team members improve patient care. The PerfectServe and Telmediq solutions automate communication-driven workflows, eliminate non-clinical tasks, promote nurse mobility, and engage patients in their own care, resulting in quicker time to treatment and enhanced patient safety. The Lightning Bolt provider scheduling solution automatically generates optimized shift schedules to reduce burnout and increase patient access. PerfectServe’s scalable, cloud-based solutions allow 135,000 physician users and 230,000 nurse users to focus on delivering the best patient experience possible.
Visit the PerfectServe booth to learn more about our leading Clinical Communication & Collaboration, Nurse Mobility, Provider Scheduling, Contact Center, Answering Service, and Patient & Family Communication solutions. Book a meeting and find more information at perfectserve.com/himss20.
Phynd

Booth 1775
Contact: Rebecca Jones, content marketing specialist
rjones@phynd.com
603.581.4331
Phynd 360, an innovative provider data platform, serves as health systems’ central hub for all provider data. Phynd enables optimization for provider data – people, places, and services – in EHR, marketing, and claims systems via platform tools for provider enrollment, management, outreach, and search across the enterprise. Phynd is a member of the Epic App Orchard. Phynd clients include some of the most progressive and innovative in the country, with seven of the top 20 “Best Hospital Honor Roll” hospitals, as ranked by US News and World Report, using the Phynd platform to power their provider data. Phynd serves as a vital enterprise data platform for digital marketing teams seeking to optimize their digital front door experience for consumers. It offers real-time provider enrollment into Epic and other EHRs, used by patient access and registration teams to eliminate the dual, never-ending streams of provider data maintenance and claims tickets backlog.
Schedule a short appointment with Phynd, and we’ll reward you with a $100 Starbucks gift card!
PMD

To arrange a meeting, contact Ryan Sciacca.
Contact: Ryan Sciacca, director of sales
sales@pmd.com
800.587.4989 x2
PMD provides healthcare teams with a suite of powerful, intuitive, mobile software that streamlines communication, enhances productivity, and increases revenue. With PMD’s mobile communication, data capture, and care navigation platforms, healthcare teams finally have an elegant and simple technology to streamline communication and revenue cycle workflows while maximizing efficiency and collaboration. PMD interfaces with all major EHRs, hospital systems, and medical billing systems, enabling the efficient sharing of data and cutting down on medical errors. PMD is committed to developing the best solution and providing superior customer service. Visit our website or contact us today for more information or to schedule a free workflow consultation.
Prepared Health

Booth 4126
Contact: Monica Ginsburg, marketing manager
mginsburg@preparedhealth.com
773.251.4845
The Prepared Health platform simplifies senior care coordination. We empower hospitals and health plans to:
- Build post-acute and home care networks – organize high-quality providers across the care continuum.
- Enable real-time communication – smarter care transitions and coordination at every level of care.
- Activate home-based insights – leverage predictive models to increase healthy days at home.
“Create Value for the Buyer and the Innovator to Support Emerging Technologies,” session 319, will be held on Friday, March 13 from 10:45-11:45am. Speakers include innovation leaders from Jefferson Health, an 18-hospital system with nearly $6 billion in revenue; and Ashish Shah, CEO of Prepared Health.
QliqSoft

Booth 421
Contact: John Skowlund, VP of business development
jskowlund@qliqsoft.com
866.295.0451
The QliqSoft team is excited to share many new patient and provider communication technology solutions at HIMSS20. Stop by booth 421 to participate in:
- Customer conversations – Hear from our customers, such as CAN Community Health and the University of Florida, about how QliqSoft solutions deliver results.
- Education sessions – Let our customer success team share all they have learned in the field. Subjects include chatbot use cases, operational effectiveness, the personification of technology, and more!
- Build your own bot: Earn your Build-a-Bot certification – You’ll leave with some sweet QliqSoft swag and your custom bot that you can take home and share with your team.
- Demo for donation – We’re donating $100 to CHIME for each CHIME member who stops by booth 421 to build a bot or demo any other QliqSoft product.
- Bots and Brews (Wednesday, March 11 at 4pm – booth 421) – Join us as we raise a toast to our most engaging team member, Quincy. Bring your healthcare chatbot questions. Bring your healthcare chatbot ideas. Let’s see where the conversation takes us.
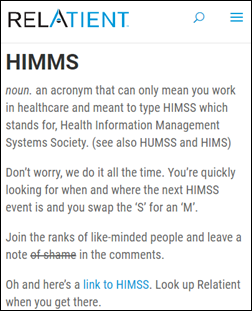
Relatient

Booth 2193
Contact: James Kanka, VP of marketing
jkanka@relatient.net
615.208.7384
Come chat with us at HIMSS, booth 2193, and learn what makes Relatient different. Customer feedback recently made us the 2020 KLAS Category Leader in Patient Outreach, for a platform that can flex to your needs and offers robust PM/EHR integration.
Swing by to enter for a chance to win in our promotions and giveaways.
Relatient’s CTO, Kevin Montgomery, is co-presenting an Essential Conversation with Oklahoma Heart Hospital’s Jonathan Minson to talk about “Achieving Patient Engagement in a Mobile-First Market.” Don’t miss out on a chance to participate in this discussion about changing patient expectations, healthcare IT dynamics, best practices for patient engagement, and insight from Oklahoma Heart Hospital, which is using patient engagement to save close to $1 million annually. This session will take place Thursday, March 12 at 1pm in room W303A.
ROI Healthcare Solutions

Booth 1213
Contact: Brent Prosser, VP, sales
brent.prosser@roihs.com
678.270.2867
ROI Healthcare Solutions is a trusted EHR, revenue cycle, and ERP consulting firm dedicated to the success of hospital and health systems across the US. Our goals center around driving cost savings, user adoption, business transformation, system performance, and operational excellence. ROI is a KLAS award-winning partner, with a unique approach to working with clients. We use old–fashioned communication, relationship cultivation, deep knowledge, and integrity to create successful on-time, on-budget outcomes. Our role varies from project to project; we are well equipped to assess, implement, upgrade, support, and staff for technology- and process-related engagements.
Our team is excited to meet with you at HIMSS this year in Orlando. We will have several raffles (wireless headsets, speakers, and more). Come by the Georgia Pavilion in Hall A for face-to-face time with our industry experts. Also, join us for a reception in our booth on Tuesday at 4:30 pm.
Spok

Booth 2579
Contact: Derek Kiecker, solutions adviser, team lead
Derek.kiecker@spok.com
952.230.5306
Spok representatives and senior executives will be on hand to show you how Spok is pioneering a new era of care collaboration. Our cloud-native, clinical communication platform gives hospitals the best in security, agility, and breadth and depth of services. Please stop by our booth to learn more about how Spok can help you achieve your hospital’s mission.
Spok will select one $500 gift card winner per day, at random, and notify them via email. Starbucks gift cards will be distributed in the booth following your demo, while supplies last. Spok will also host a social media contest: Tweet tagging @Spoktweets and using #HIMSS20 for your chance to win a $50 Amazon gift card each day of HIMSS20.
StayWell

Booth 3521
Contact: Eileen Faas, marketing manager
efaas@staywell.com
734.904.5880
StayWell is a health empowerment company that uses the science of behavior change and technology-driven programs to help people live healthier, happier lives. At this year’s HIMSS, StayWell will reveal its latest advancements in its health management solutions that connect the digital health universe among multiple points of engagement.
Using high-touch, high-tech solutions to present a progressive yet balanced approach to managing health risks, StayWell’s newest updates integrate the latest achievements in AI, interactive learning, and online health engagement to improve care, enhance provider knowledge, and advance care management.
Summit Healthcare

Booth 5558
Contact: Christine Duval, marketing manager
cduval@summit-healthcare.com
781.519.4840
We’re here to help you tackle any integration or automation challenge your organization is facing! Stop by to see our Robotic Process Automation (RPA) offerings LIVE. You will also have the chance to experience the company’s other advanced systems integration, automation, and business continuity offerings. These include Summit Exchange, which enables hospitals to manage systems integration at an enterprise level; and Summit All Access, the powerful, Web-enabled platform for 24/7 data exchange and availability. Attendees will also be able to explore the possibilities of utilizing Summit All Access as a business continuity tool in the event of planned or unplanned downtime, as well as resolving patient matching and duplicate record issues with the new Summit EMPI, powered by Dedalus.
Surescripts

Booth 2030
Contact: Komita Primalani, director, marketing events
komita.primalani@surescripts.com
571.303.0884
HIMSS20 invites health IT stakeholders to “be the change,” and Surescripts will be showing up with lots of practical guidance on transforming healthcare interactions for the better. From helping patients get affordable medications to navigating the shifting landscape of interoperability and information sharing, we’ll partner with experts from across the Surescripts Network Alliance to dig into some of the biggest developments in health IT. Visit us at booth 2030 to find out how we can make an impact together.
TransformativeMed

To arrange a meeting, contact Rodrigo Martinez.
Contact: Rodrigo Martinez, chief growth and clinical officer
rodrigo.martinez@transformativemed.com
303.301.4175
TransformativeMed is thrilled to once again attend HIMSS – such an exciting venue to learn about the latest and greatest in technology. We’re already providing EHR-embedded solutions that are solving some of today’s most challenging problems – physician burnout, satisfaction, and efficiency, thus enabling better patient outcomes. We’d enjoy connecting with our current and future clients. Our specialty-specific clinical workflows are rich in content by specialty, intuitive to the clinician’s natural workflow, and deeply embedded in the EHR. Our disease-specific workflow platform provides the care team with disease-specific workflows such as diabetes management, thrombolytics, etc., enabling more effective management of their patients across the care team(s). We will also have a CHIME focus group on Tuesday, March 10 from 4-5:30pm on the next generation of mobility for the health system and clinician.
Waystar

Booth 1421
Contact: Tina Newman, events director
Tina.Newman@waystar.com
Waystar provides next-generation, cloud-based technology that simplifies and unifies the healthcare revenue cycle. Our platform removes friction in payment processes, streamlines workflows, and improves financials for providers in every care setting. Waystar has scored Best in KLAS for claims and clearinghouse every year since 2010, and has earned multiple #1 rankings from Black Book surveys since 2012.
Waystar is proud to introduce Hubble, its new AI + RPA platform. We look forward to sharing how Hubble can help our clients achieve more efficient workflows, fewer rejected claims, and a better bottom line. Stop by booth 1421 to see a Hubble Demo!
Zen Healthcare IT

Booth 8145
Contact: Brian KIsanov, solutions manager
brianK@consultzen.com
949.396.0361
Zen Healthcare IT is 100% focused on the challenges associated with moving data through the healthcare ecosystem. We simplify interoperability by bringing our expertise together with our Gemini Integration as a Service Platform. Designed for big or small healthcare messaging problems, Gemini offers a very flexible platform to meet a wide variety of healthcare interface needs. Zen’s clients include providers, hospitals, HIEs, healthcare vendors, agencies, and payers.
Interested in learning more about the national trusted exchange networks? We will have our EHealth Exchange/Carequality experts in the booth to answer your questions. Zen is a Carequality Implementer and has onboarded many healthcare organizations to IHE-based exchange.
Comments Off on HIStalk’s Guide to HIMSS20
















































































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…