Matt Wilson is SVP of healthcare strategy for Infor of New York, NY.

Tell me about yourself and the company.
I’m a healthcare IT lifer, with 27 years in the industry. It’s kind of a family business. My father was an HIT executive going back into the 1970s, so I have been in and around this business for my whole life. I am fascinated in the way it has evolved and I enjoy watching its trends. It’s a pleasure having the opportunity to participate.
Infor is a global cloud computing company with deep investments in industry-specific lines, executives, and products, such as Infor Healthcare.
How has adoption of cloud technology in healthcare changed?
Adoption of cloud technology gives us an opportunity to manifest a remote workforce, which we’ve seen through the pandemic, and we will see more of that. Cloud provides the ability to rapidly respond to customer needs with updates that don’t require the same kind of effort as on-site, on-premise solutions. We can engage our customers more consistently and more rapidly, which is an enormous benefit of cloud in addition to the reduced costs of maintenance.
Are you seeing a new urgency for agility in your customers since the pandemic started?
We are. Customers need us to be agile, especially in areas such as supply chain and real-time location services. Our objective has been not to get in our customers’ way, but simply to make ourselves available for what they need. We have found that our greatest opportunity to help has been engaging with something that takes a couple of weeks instead of the months and months that we’re used to with typical implementations.
How do you see the synergy between EHRs and enterprise resource planning systems?
Infor as a company, and I as an individual, are focused on how create a more balanced ecosystem. We have spent years and years, decades in fact, investing in EHRs. I was a beneficiary of that, as I helped build Cerner through the late 1990s and early 2000s. The lack of commensurate investment in ERP has created an imbalance.
We believe we can move the industry by modernizing the technology, driving a set of functionalities that contribute to the core mission of patient outcomes and a better system of health and wellness. You must have world-class systems and functionality across the core pillars of finance, supply chain, and human capital management. The way that we use interoperability and the way we orient ourselves to that core mission is critically important.
What is left to accomplish with ERP?
We need to bring together those investments to orient themselves to a single goal. We have tended to think about upgrades and technology as an ability just to upgrade the tech itself. The future holds orienting towards making one leverage off of the other, creating that ecosystem and integrating some of the billions of dollars we spend each year on management consulting on transformation. That transformation creates change. Tech should be used to sustain change. As you are moving forward with big transformation projects, how can you use your clinical solutions, your revenue solutions, and your business solutions to sustain the efficiencies, cost reductions, and tech advancement? That will be critical as we move forward, and we can play a big role in that.
As EHR and ERP vendors get bigger, does the opportunity still exist for smaller vendors to offer an ecosystem of wrap-around products?
Our Cloverleaf solution is the most widely implemented integration engine. True interoperability creates a wire that connects both traditional and nontraditional data sources and care venues, but should be used to facilitate small tech, where the gating factor for cool, innovative companies to have their products used by big health systems is the IT organization. They don’t have the time and resources to complete the interfaces, or there’s a lack of understanding around anything from security standards to interoperability.
Big platform companies like Infor and the large clinical software vendors should think about how we can facilitate the inclusion of that other cool technology that can help drive value. How can we more easily connect them into that ecosystem for the purpose of creating balance? That should be one of the central themes that we as big platform vendors should be thinking about. I think a lot about that in my role at Infor.
How do you assess the federal government’s interest in interoperability?
The Cures Act has laid down to the letter the requirement to interoperate. Vendors often give lip service to how they’re adhering to that, and some vendors continue to push back. We are seeing an absolute requirement to go do that. We’re looking to facilitate it.
What we need is an attitude change. While it can legitimately be an impediment to competitiveness, what we should be thinking about is how we’re working together to advance an industry right now that is not in the best of shape, an industry that is critical to us as a society. We need to take that signal, act on it, and find ways to include others. We are seeing those signals from life sciences, big lab testing companies, and payers that they need to be a part of that as well. They are developing standards that are oriented towards meeting those federal guidelines and making data liquidity a prime imperative in healthcare.
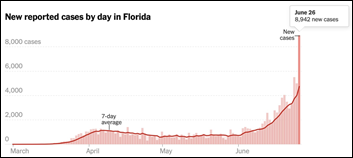
What was your reaction when you saw that the information that is needed for pandemic-related public health reporting was being sent by fax machines and emailed worksheets?
It’s just such an incredibly inefficient process. There is regulation to begin phasing out fax machines, but we need to move more quickly. That’s an area that we think will evolve quickly, even potentially with stimulus, in the area of supply chain and public health reporting. Those are necessary when something goes wrong, such as a once-in-a-generation pandemic.
The billions and billions that we’ve spent were sufficient in areas such as telehealth, but didn’t get us where we needed to be in terms of a fractured and disrupted supply chain and using antiquated technology to quickly report on outcomes. Interoperability becomes a central theme, and while we have had so many attempts with CHINs, RHIOs, and the rest of the alphabet soup, we still haven’t effectively created a true system-wide capability to normalize data and move that data around for those purposes that you’re describing. That’s critical as we move forward.
Are customers asking for new capabilities or guidance to help them stabilize their supply chains?
We asked clients what they need most. We responded quickly by developing supply chain dashboards for PPE. We are proud of how we were able to participate in a bit of a solution. We think that will be an ongoing need, the requirement to connect disparate supply chains and to develop functionality to find clinically equivalent alternatives when a particular supply, device, or PPE item becomes unavailable. We have to evolve with our use of AI, machine learning, and physically connecting suppliers. We will work closely with our customers as we go forward because it will be critical if we experience something like COVID-19 again.
What product opportunities do you see with AI?
For us, again as a platform company, we have so many opportunities to advance and help. It’s really listening to the market. What we are hearing from caregivers and business operations associates is that supply chain becomes a huge issue. We saw human capital management evolve and the role of chief human resources officer created around the country, and we expect to see more senior executive supply chain personnel taking roles in the strategy of the organization.
We also see a huge need around real-time location services in contact tracing, to be able to efficiently understand where a diagnosed patient has been, what equipment they have touched, and where that equipment is at the moment. Apple and big tech companies are working on that for consumer. We have solutions, but more importantly, we need to continue to evolve that inside of the hospital system. It’s critical when you have something like COVID-19 or Ebola that you know where things are, whether they are usable, and who is coming in contact with them.
The pandemic seems to be accelerating the health system acquisitions that create sprawling regional or even national enterprises. How do you respond as your customers get bigger and move into business areas that don’t involve traditional hospital operations?
You respond by listening, even though that is a bit of an obvious answer. We also try to educate ourselves to become healthcare experts. We spend a lot of time talking to outside interests, outside experts, and trying to understand where we should push, advance, and lead through thoughts and action.
We saw two things advance during the pandemic. We saw not only telehealth and the inevitability of pushing healthcare out more directly into the community, but we also saw an evolved need for inpatient facilities. We had been moving away from that over the last decade as we attempted to decentralize healthcare, but all of a sudden, we saw this need to ramp up quickly.
As a software vendor, the key is flexibility. Are we making core investments in the things that we do well today? Are we making core investments in technologies that allow us to be flexible, like contact tracing and interoperability, things that allow us to move where healthcare is and to bring our solutions and services where our customers need them, not where we think we’ve designed them to operate? That’s a critical piece.
Do you have any final thoughts?
We hope that investors and users will give us the opportunity to display how a traditional ERP company can become central to a mission. It’s not enough to upgrade technology, create a better user look and feel, and deliver greater functionality in its traditional sense. We can be accretive to the broader picture of healthcare by providing this healthcare operations platform that helps balance out that ecosystem, works together with clinical, and advances the overall mission of the organization. That’s what Infor is looking to do, and we invite others to speak with us and give us that chance.
Comments Off on HIStalk Interviews Matt Wilson, SVP of Healthcare Strategy, Infor

































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…