Monday Morning Update 12/21/20
Top News
Imaging worklow vendor Intelerad acquires Digisonics, which sells cardiovascular and OB/GYN information systems.
Reader Comments
From Money Heist: “Re: investment. Why the sudden overabundance of investment news in HIStalk? Are your interests changing?” Health IT investment activity is soaring, especially with the sudden popularity of backdoor IPOs via special purpose acquisition companies (SPACs) that are required to complete a deal within two years or give investors their money back. Accordingly, acquisition prices are way up and expectations from folks who paid high per-share prices will follow, meaning it’s important to see how customers and competitors are affected by these financial gyrations. There’s only so much to say about the Big Three inpatient EHR vendors now that the HITECH land grab is over (unless they make an acquisition, of course), so the industry is focused on new sectors and new players, especially those that aim to pick the deep pockets of insurers, pharma, drug store chains, and even masses of consumers who are happy to lay out cash for whatever prescriptions, diagnostics, and treatments they want in bypassing the usual gatekeepers. Healthcare is, unfortunately, almost entirely driven by profits, the actions of big companies, and the heavy involvement of government as an insurer, provider, and legislator — the rest of us, including patients, are just gawking bystanders.
HIStalk Announcements and Requests
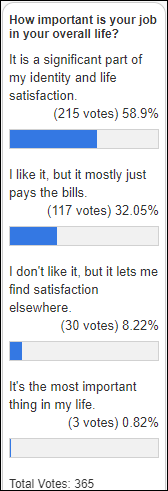
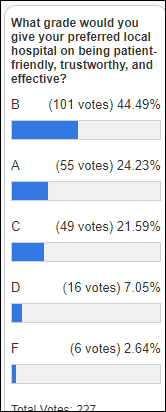
Many poll respondents say that their job represents a big part of their identity and life satisfaction, which I guess is a good news-bad news sort of situation where they are happy with the work that contributes so heavily to the perceived quality of their existence, but that perhaps dangerously makes them dependent on an employer whose goodwill is situational (my personal experience is that a new boss, company sale, financial stumble, or backstabbing colleagues can end those happy workdays quickly). Look down the road as well to unintentional unemployment or retirement, when the well-meaning but misguided question of “What do you do?” (meaning, “to whom do you sell time and for doing what as your primary identity?”) has no easy, pat answer.
New poll to your right or here: What are your COVID-19 vaccination plans?
I’m fascinated by the argument over whether someone who has earned a non-medical doctorate should use the title of “Dr.” and in what setting. Even with medical doctors it’s not cut and dried — UK doctors earn an MBBS, which is a professional bachelor’s degree that is equivalent to MD, and I’ve heard that they called generalists “Dr.” and specialists “Mr.,” although I’m too lazy to look that up. I say we stop calling everyone Dr. as part of their name since that term is vague (I’m thinking of those chiropractors who place “Dr.” in front of their name instead of “DC” after it in their ads, hoping for some beneficial confusion.) Meanwhile, I’ll defer to the AP Stylebook, which says to use Dr. in the first reference to someone who holds specific medical degrees such dentistry, allopathic or osteopathic medicine, podiatry, or veterinary medicine – notice that list does not include pharmacists, doctorate-level nurses, physical therapists, or PhDs. Actually, I’m not sure that we even need any titles as part of names in our stridently informal society, especially with the gender-signifying issues that result – does someone really need to be Mr. Smith instead of just John? Meanwhile, feel free to address me as Reverend Doctor HIStalk since I bought those credentials from the Universal Life Church with college work-study money in hoping to created a higher-power aura that women would find irresistible (pretty much like a lot of people who wave their “Dr.” titles in the faces of strangers, in fact).
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Tenet Healthcare will sell 87 of its CareSpot and MedPost urgent care centers to FastMed Urgent Care for $80 million as it refocuses on the 45 ambulatory surgery centers that it is buying for $1.1 billion. North Carolina-based FastMed operates 104 locations in Arizona, North Carolina, and Texas. Googling suggests that CareSpot and MedPost use NextGen, while FastMed announced in January 2020 that it was implementing Epic in all of its locations.
In Canada, Telus Health acquires virtual care provider EQ Care.
Sales
- The State of Virginia will spend $10 million in federal coronavirus aid money to implement Unite Us to connect the EHRs of health systems and medical practices to manage social services referrals.
- Highmark Health chooses Google Cloud in a six-year deal to develop Highmark’s Living Health Model, described by Highmark marketing committees who flung buzzwords like a zoo monkey’s feces until this vague “Curated Design” description earned the most colored sticky dots: “Our new design will have health care operating differently — better. It will become an experience that is simple, easy, and streamlined for all parties.” Highmark says it is changing a broken healthcare system (in which it profitably participates with $20 billion in annual revenue and an $8 million CEO) because of its sudden realization that “it’s the right thing to do.” Remind me to check back in a couple of years to see if Highmark makes good on its promise that its relationship with Google will end healthcare-related stress, confusion, fragmentation, reactive processes, complexity, and high cost.
- NHS Greater Glasgow and Clyde Health Board join the TriNetX global health research network, which has presented 7,800 clinical trials opportunities to 170 healthcare organizations in 30 countries.
- Ochsner Health chooses Loyal for patient self-scheduling and website live chat.
People

Jason Dvorak (Hillrom) joins Lohman Technologies as president.
Government and Politics
HHS OCR publishes guidance on how HIPAA allows covered entities and business associates to disclose PHI via HIEs for public health activities. High points:
- Covered entities can send patient data to HIEs when disclosure is required by law, such as sending infectious disease lab testing data.
- Covered entities can assume that whatever information the public health agency requests is minimum necessary, such as the Common Clinical Data Set, without making their own determination. CDC’s request for COVID-19 patient data via Electronic Case Reporting and state influenza reports are examples.
- Covered entities may disclose bulk PHI to public health agencies via an HIE without individual patient approval as long as they verify that the agency has permission to collect the data.
- OCR will not impose penalties on business associates or covered entities that transmit PHI for public health activities, regardless of whether their business associate agreement specifically permits such disclosure.
- Covered entities must provide requesting individuals with an accounting of disclosures that includes public health reporting.
COVID-19
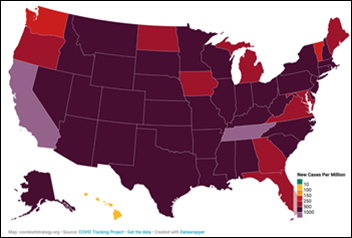
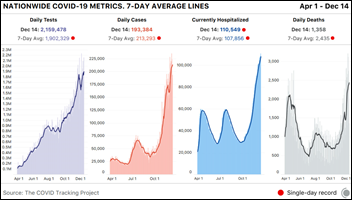
Friday set a US COVID-19 hospitalization record of 114,751 and another 2,751 deaths. Tennessee has the world’s worst infection rate per capita at 1,300 per million residents and rising, joining California as the only state whose rate exceeds 1,000. Tennessee announced Saturday tat it has passed 6,000 deaths, has 2,893 people hospitalized, and is showing a test positivity rate of 30%. COVID Tracking Project keeps having to make up new colors in extending beyond red to illustrate the uncontrolled US coronavirus spread.
A newspaper investigation concludes that Florida stopped reporting backlogged deaths from October 24 to November 17, creating big drop in the death count right before and after the election. Governor Ron DeSantis has changed the reporting requirements multiple times and is accused by fired state COVID-19 data scientist Rebekah Jones of falsifying the numbers to support the state’s aggressive reopening, which he denies.
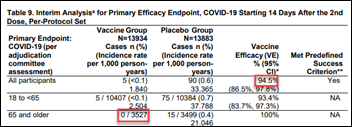
FDA issues its Emergency Use Authorization to Moderna’s COVID-19 vaccine, with the first doses to be administered Monday.
A CDC panel recommends that people over 74 years of age and 30 million frontline essential workers get COVID-19 vaccine first, with Monday’s expected approval of those recommendations being sent to states as guidance. CDC says that 556,000 people in the US got their first shot in the past week.

Stanford Medicine medical residents and fellows protest at being mostly left out of its COVID-19 vaccine distribution plan, as only seven of the 1,300 made the list even though many of them are frontline COVID-19 caregivers. The health system and medical school apologized, explaining that their algorithm prioritized recipients based on work unit and age, but nobody noticed that house staff were skipped over because they don’t have an assigned location that indicates their involvement with COVID-19 patients. Stanford University is of course a globally recognized Silicon Valley center for AI excellence, but perhaps its humans – especially the non-executive ones — needed to be more involved in double-checking how its AI evaluates equitable access.
In the UK, Boris Johnson imposes a full emergency lockdown of London and southeast England following the rapid spread of a new COVID-19 strain that is responsible for 60% of new infections, which doubled in London in the past week. The new strain is no deadlier and offers no new vaccine resistance and is therefore curious but not alarming to epidemiologists, but it does appear to be more contagious.

A United Airlines passenger with COVID-19 symptoms dies on a flight from Orlando to Los Angeles, which his wife says he was able to board because he lied that he was symptom-free on the passenger declaration form. Three fellow passengers performed CPR for an hour until the flight landed in New Orleans after being diverted, and one of them is now experiencing COVID-19 symptoms.
Other
University Hospital (GA) says that hackers are attempting to penetrate its Epic MyChart system 550 times each day, while its email security system is rejecting 20% of incoming email due to security threats.
Seattle-area drugstore chain Bartell Drugs will pay $800,000 to settle DOJ charges that it failed to implement a computer system to verify prescriber licensure, which allowed pharmacists to fill 400 opioid prescriptions that were issued by doctors whose licenses had been suspended, some of whom had been sanctioned or indicted for federal violations. The chain is being sold to Rite Aid for $95 million.
Sponsor Updates
- Pivot Point Consulting releases its new Quarterly Pivot report, focusing on trends to watch in Q1 2021.
- Pure Storage makes available Pure as-a-Service in the AWS Marketplace, and launches its Cloud Block Store Efficiency Guarantee to improve cloud economics.
- Zynx Health publishes a review of COVID-19 vaccine administration guidelines as the FDA authorizes emergency use of the Pfizer/BioNTech COVID-19 vaccine.
- Meditech customer Sunderland Royal Hospital becomes the first hospital in the North of England to earn HIMSS Stage 7 recognition.
Blog Posts
- Trends to Watch in 2021: Telehealth, Consumerization and AI-powered Clinical Decision Support (Nuance)
- 2020 Year in Review: Pharmacy is the Answer (OmniSys)
- Top 4 trends for digital transformation in Life Sciences in 2021 (OpenText)
- Preparing for the 2021 E/M code transition begins with education (Nordic)
- Making Software More Inclusive to Improve Patient Care and Safety (PMD)
- The ABCs of ACOs (Premier)
- Virtual Visits are More Important Than Ever. Is Your Practice Ready? (QliqSoft)
- 12 Healthcare Solutions for our Favorite Holiday Songs (Redox)
- Building a telemedicine training program for clinicians (SOC Telemed)
- Spirion employees recognized for taking local action during global pandemic (Spirion)
- 3 ways to optimize your hospital’s directory and on-call schedules to reach providers faster (Spok)
- Understanding the mRNA COVID-19 Vaccine (Krames)
- Three Ways Healthcare Technology is Accelerating (Surescripts)
- Health AI University Recap (SymphonyRM)
- RSNA 2020: Visage’s Top Five (Visage Imaging)
- Nurses and Other Frontline Workers Need Our Support Now More Than Ever (Vocera)
- The future of Medicare Advantage: what providers need to know (Waystar)
- 10 Ways to Cultivate a Positive Culture in Your Clinic (WebPT)
- Well COVID-19 Vaccine Tip Sheet (Well Health)
- Here Are Some Opportunities to Enhance the Virtual Healthcare Experience (Wolters Kluwer Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…