Top News
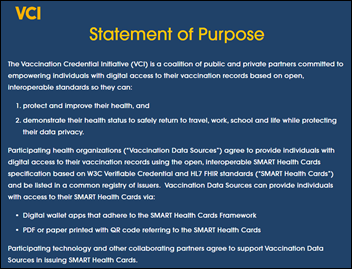
Health and technology leaders announce the Vaccination Credential Initiative, which hopes to provide digital access to COVID-19 vaccination records using the open SMART Health Cards specification.
Individuals could obtain an encrypted digital copy of their immunization credentials to store in a digital wallet or could receive a paper form containing a QR code.
The goal of the initiative is to connect to The Commons Project Foundation’s CommonPass, which is being used for travel and return-to-work vaccine verification.
Participants include CARIN Alliance, Cerner, Change Healthcare, The Commons Project Foundation, Epic, Evernorth, Mayo Clinic, Microsoft, Mitre, Oracle, Safe Health, and Salesforce.
Reader Comments

From Assign Me Up: “Re: email updates. Please enroll me at this new address and remove the old one.” I’ve been remiss in not providing self-service email signup instruction reminders in many months, so here’s a refresher:
- Sign up for updates here or using the “Subscribe to updates” menu option under Contact (desktop format) or the “Get email updates” menu option (mobile format).
- Watch for the verification email that follows since it may end up on your spam folder and you’ll receive no further emails unless you confirm this one.
- Review your email rules, whitelist, company email server setup, etc. if you aren’t receiving the emails you signed up for. The automatic sending of the emails is highly reliable, but the receiving of them is much less so and is not something I can control (spam tools have eliminated the reliability and timeliness of email delivery, unfortunately).
- Unsubscribe your old address by clicking the ‘”unsubscribe” link that is at the bottom of each email. Or, do nothing since your inactive old address will cancel itself even if you do nothing.
- Reminder: I do absolutely nothing with the email addresses, so all you’ll get as a result of signing up is a notice that I’ve posted something new. I collect only the actual email address itself, don’t use those addresses for anything else, and don’t make them available to others.
From Clog Queen: “Re: HIStalkapalooza shoe contest. I think that in these challenging times (don’t all emails start with that phrase these days?) you should do a virtual version.” Certainly the shoe contest would virtualize better than most conference components since judges would just need to review photos, perform their deliberations, then announce the winners. I bet closets are full of low-mileage yet stylish zapatos since they add no value to a Zoom call.
From Dunning Notice: “Re: HIMSS21. Are you doing a booth this year, assuming the conference goes on?” No. It’s been nice in the past to have a place to say hello to readers on the show floor, but it’s not worth the several thousand dollars that a microscopic 10×10 foot space costs when I have nothing to sell that would offset that personal expense. I’ll probably (not certainly as of yet) be treading the thick exhibit hall carpet as a paying attendee, using my HIMSS20 registration rollover, if HIMSS21 happens. Thank goodness I ended HIStalkapalooza in its 10th iteration at HIMSS17 since I would have faced financial Armageddon otherwise from the cancelled HIMSS20.
HIStalk Announcements and Requests
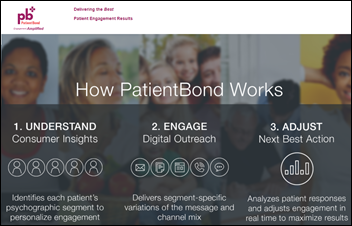
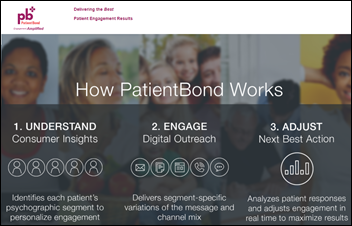
Welcome to new HIStalk Platinum Sponsor PatientBond. The Salt Lake City company applies consumer insights and innovative technologies to digital patient engagement. Its Digital Health Platform uses a proprietary psychographic segmentation model that allows health systems, urgent care facilities, and medical practices to personalize messaging and digital channels to each individual’s motivations and preferences, supporting market share growth (patient acquisition and loyalty, service line marketing, and social reputation management); improved patient outcomes (closing care gaps, improving medication adherence, and automating care coordination); and increased patient payments (reminders, online payments, digital statements, and card-on-file messaging). The cloud-based, API-driven platform requires no training, no software to install, and offers easy integration with most CRM, EMR, and PM systems. Discover which of its five psychographic segments you fit in as a patient by answering a 12-question survey. Thanks to PatientBond for supporting HIStalk.

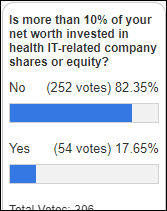
Thanks to the 2,000 folks who completed my once-yearly reader survey. Resultant factoids:
- 94% of respondents say they have a higher appreciation for companies they read about in HIStalk, while 82% have a higher appreciation for HIStalk sponsors.
- 94% say that reading HIStalk helped them perform their job better in 2020, which is a relief since that’s my most-valued metric.
- I’ve emailed the winners of $50 Amazon gift cards who were randomly drawn from participants. Thanks to all who completed the survey.
Webinars
January 28 (Thursday) 12:30 ET: “In Conversation: Advancing Women Leaders in Health IT.” Sponsor: Intelligent Medical Objects. Presenters: Tabitha Lieberman, SVP of clinical and revenue cycle applications, Providence St. Joseph Health; Ann Barnes, CEO, IMO; Deanna Towne, MBA, CIO, CORHIO; Amanda Heidemann, MD, CMIO, CMIO Services, LLC. IMO CEO Ann Barnes brings together a panel of female health executives for a results-oriented discussion on how managers and C-suite executives can address diversity and inclusion in their organizations. From STEM education to mentoring and networking, the “COVID effect” on women in the workplace, to matters of equity, there’s no better time to talk openly about these issues to help generate meaningful change in healthcare.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Provider and resource scheduling system vendor QGenda acquires Shift Admin, which offers shift-based specialty scheduling for emergency medicine, urgent care, and hospital medicine.
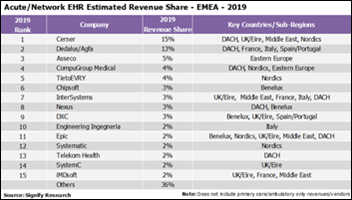
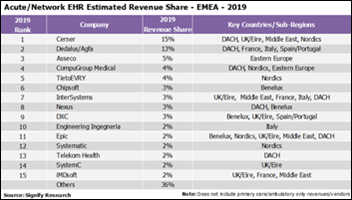
Signify Research says the EHR market in Europe and EMEA in 2020 was better than in the US, which declined due to COVID-related financial challenges. It also notes that consolidation is picking up in Europe, with Dedalus acquiring Agfa’s HCIS business, CompuGroup Medical buying parts of Cerner’s non-Millennium assets, and the merger of big Nordics vendors Tieto and EVRY.
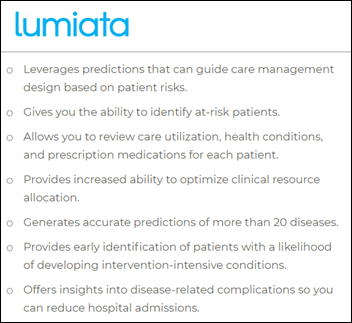
Lumiata — which applies AI to 120 million patients records to predict patient outcomes, clinical costs, and risks for providers and payers – raises $14 million in a Series B funding round.
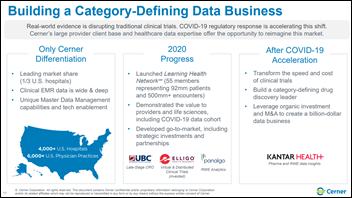
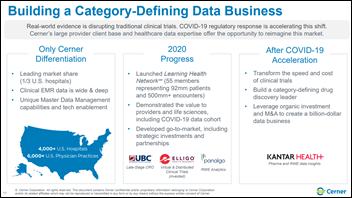
Cerner says in its J.P. Morgan Healthcare Conference investor presentation that it will create a billion-dollar data business in selling de-identified patient data as real-world evidence to drug companies, partly driven by its $375 million cash acquisition last month of Kantar Health.
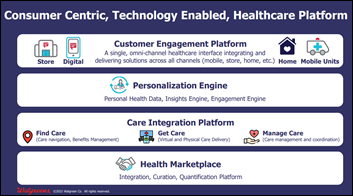
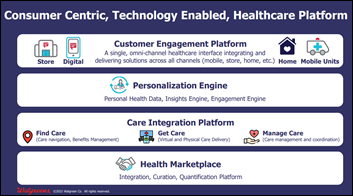
Walgreens says in its J.P. Morgan Healthcare Conference presentation that it will create a tech-enabled healthcare startup as a “company within a company” that will offer a customer engagement platform, a personalization engine, a care integration platform, and a health marketplace. The company says that neither a digital-only nor a physical-only platform can be successful. It will partner with best-in-class companies as an integrator. The company said in Q&A that it expects to be part of the care team in offering patients real-time information for managing conditions and recommending medication changes to doctors, enabled by the increasing scope of pharmacist practice in some states. Walgreens has seen a 40% jump in pharmacist involvement with medication therapy management. It adds that a patient with multiple chronic conditions is forced to log into multiple apps, a process that it intends to simplify.
NextGen Healthcare’s J.P. Morgan Healthcare deck highlights its December 2019 acquisition of telehealth platform vendor Otto Health for a reported $22 million, after which its virtual visits have increased by 68%, active user count has jumped from 300 to 13,000, and contracted annual recurring revenue has increased from $200,000 to $9 million.
Sales
- Virginia Department of Behavioral Health and Developmental Services chooses Cerner’s EHR for four additional behavioral health facilities.
- Konica Minolta Japan will use InterSystems IRIS for Health and its HL7 FHIR interoperability capability to connect its devices with other systems, such as the EHR.
Announcements and Implementations
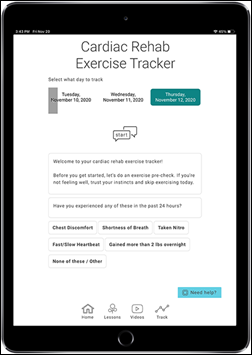
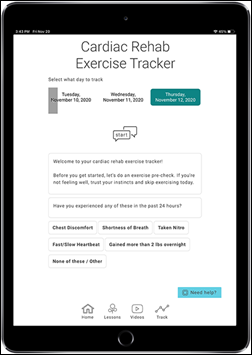
Healthwise announces five Digital Health Programs – for diabetes, cardiac rehab, colonoscopy and endoscopy, orthopedics, and pregnancy and newborn – that allow providers to send education and reminders and receive individual and aggregated analytics to monitor patient progress.
Meditech offers a short-form Quick Vaccination solution that allows hospitals to administer COVID-19 vaccine at high-volume locations and transmit vaccine data to state systems.
Specialty EHR vendor Modernizing Medicine acquires Exscribe, which offers an orthopedics EHR.
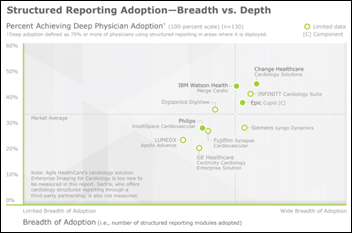
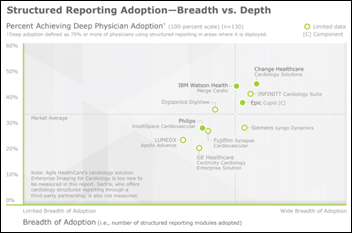
A new KLAS report on structured reporting in cardiology finds that Change Healthcare and IBM Watson Health lead in adoption, Epic saw the biggest adoption increase but Cupid still requires a lot of work and is missing some functionality, and customers of Lumedx are frustrated with poor training, support, and development.
Government and Politics
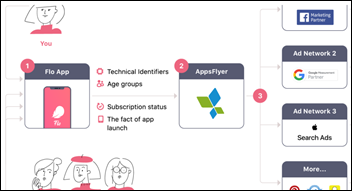
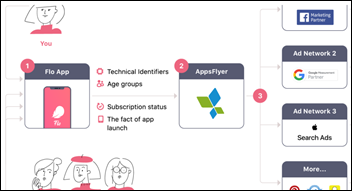
Flo Health settles FTC charges that its Flo Period & Ovulation Tracker app shared user information with Facebook, Google, and other companies while assuring users that it would keep their information private. The company will have its privacy practices independently reviewed and will get user consent before sharing user data. Some members of FTC’s panel dissented parts of the settlement, saying that FTC should have charged Flo with violating the Health Breach Notification Rule that would have required notifying individual users, while Commissioner Noah Joshua Phillips issued a statement saying that simply requiring a company to notify users isn’t worth much if those users have no remedial actions available to them.
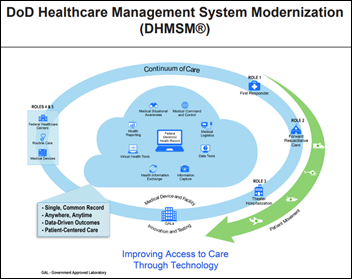
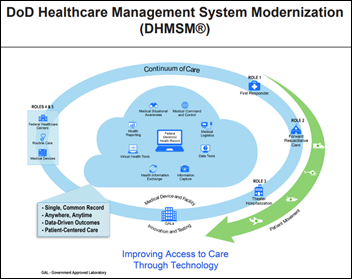
A Department of Defense annual review of its MHS Genesis Cerner implementation (thanks to reader Vaporware? for sending the link) finds that:
- MHS Genesis “is not operationally suitable because training remains unsatisfactory, dissemination of system change information is inadequate, and usability problems persist.”
- The system is operationally effective for basic operations in conventional clinics, but not for some specialty clinics and business areas.
- Performance scores increased from 45% of tested performance measures to 78%, with improvements needed in medical readiness, provider referrals, business intelligence, billing, coding, and reporting.
- System usability improved from “unacceptable” to “marginal-low.”
- The project has 158 open high-priority issues.
- Information exchange with required external systems was “sporadic, and the data were sometimes inaccurate and complete.” AHLTA-housed patient allergies, meds, and immunizations didn’t transfer to Cerner 13% of the time and care was sometimes delayed because of the manual reconciliation that was required.
- Cybersecurity experts found the system to be “not survivable in the complex, cyber-contested environment of a major medical facility.”
- Testing has not yet been performed to determine if the system can sustain the expected number of users at full deployment.
COVID-19
US COVID-19 hospitalization numbers dropped a bit on Wednesday, with 130,383 people in hospital beds with COVID. Daily deaths were also below record numbers at 4,022. Hard-hit UK and Ireland, which have high B117 variant activity, also showed a sharply reduced number of cases. CDC reports that 11 million vaccine doses have been administered of 31 million distributed, leaving two-thirds of them sitting unused.
The COVID Tracking Project warns that it will no longer report “recovered” patient numbers since not all states report that number and the term “recovered” has no standard definition and thus is reported in different ways by individual states. It also notes that many people who have had COVID-19 still don’t consider themselves to be free of symptoms.
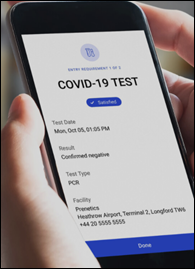
CDC will require all travelers who are entering the US – including US residents — to show either (a) their negative coronavirus test results from within the previous three days; or (b) proof that they have recovered from COVID-19. Airlines will be instructed to not allow boarding to any passengers who cannot provide the documentation.
China locks down 22 million residents of several cities following a COVID-19 outbreak. The entire country of 1.4 billion people is reporting 109 new cases per day, while the US has that many new cases every four minutes with one-fourth of China’s population.
A Public Health England pre-print study finds that people who have already had COVID-19 are 83% less likely to get it again and are probably protected for at least five months.The researchers note that nobody knows if they can still spread infection to others.
People from Canada and Argentina are traveling on private jets to Florida to get COVID-19 vaccine, taking advantage of the state’s policy to vaccinate anyone over age 64 regardless of residency.
Stormont Vail Health disables its employee COVID-19 vaccine sign-up site after discovering that outsiders were able to sign up for shots using links that employees had shared with them. The hospital will now require those who are being vaccinated to show their badges, which it wasn’t doing before.
The former president and CEO of Canada’s London Health Sciences Centre sues the hospital for $2 million, claiming that he was fired this week for making five trips to the US despite Canada’s ban on non-essential travel across the border. Paul Woods, who is a Canadian citizen who holds permanent resident status in the US, says the hospital’s chief counsel approved his request to visit his daughter and his fiancée in Michigan as long as he self-isolated afterward. The hospital’s board chair resigned the day after the lawsuit was filed, admitting no wrongdoing.
Other
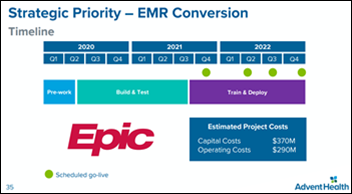
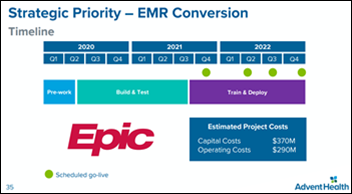
AdventHealth’s replacement of Cerner, Athenahealth, and Homecare Homebase with Epic will cost $370 million in capital cost plus $290 million in operating cost, according to its J.P. Morgan Healthcare Conference presentation. AdventHealth, the former Adventist Health System, says Its first go-live will be in Q4 of this year and the last will be finished a year later. The Florida-based system has 50 hospital campuses in nine states, 2,300 employed physicians, 80,000 employees, and $12.5 billion in annual revenue.
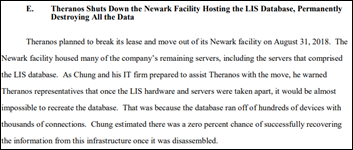
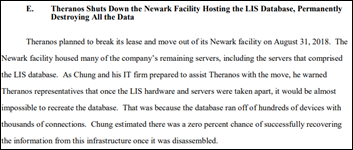
Prosecutors say that Theranos destroyed the SQL database of its laboratory information system when it closed its New Jersey facility in 2018, making its patient records unavailable for use in the federal government’s fraud case. The company paid a firm that was run by an associate of former Theranos COO Sunny Balwani $10 million over seven years to administer the database. Theranos provided the government with three versions of the backup before the company shut down, but all of them were encrypted with a password that everyone involved claims they have forgotten. Prosecutors hoped to use the database to prove their claims that tests offered by Theranos were unreliable, including one thyroid test whose failure rate was over 50%. The government also asked the court to deny the motion by former Theranos CEO Elizabeth Holmes to exclude what she calls “anecdotal” test results since the company destroyed the database while under subpoena.
A public hospital in China becomes the first to bill a patient using its blockchain-based invoicing system, which allows patients to review their medical and billing records on their phones.
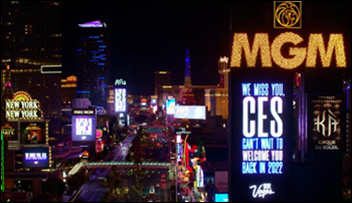
HIMSS21’s home of Las Vegas, which has the highest unemployment rate of major US metro areas at 11.5%, is taking another hit this week with the move of the Consumer Electronics Show to a virtual format. CES was supposed to be the first event in the $1 billion expansion of the Las Vegas Convention Center, which remains unused. CES expects its show to return in 2022, but most likely in a partially digital form.
Talk about positive patient ID: Denver police arrest the wrong woman for burglary after being told their suspect was an inpatient at St. Joseph’s Hospital, which they confused with Denver Health, where they arrested patient Sarah Cook in her hospital bed. Cook, who is a nurse, spent two nights in jail until police checked surveillance footage and realized that the brown-haired Cook wasn’t the blonde suspect they were seeking. The police department apologized, the officers were suspended for 10 days for failing to positively identify Cook before arresting her, and Cook is suing the police department.
Sponsor Updates
- The United States Park Police and the District of Columbia government will use Everbridge software to provide subscribers with safety, weather, traffic, event, and emergency alerts leading up to and during the presidential inauguration.
- Experity offers updates on state-based COVID-19 vaccine provider enrollment information.
- The HCI Group Chief Digital Officer Ed Marx will speak at the HIMSS Dallas/Forth Worth Chapter’s Annual C-Suite Panel January 29.
- Konica Minolta Japan selects InterSystems IRIS for Health for rapid, FHIR-based data integration for imaging devices.
- Nordic is named a leader in Everest Group’s Healthcare IT Services Specialists PEAK Matrix Assessment 2021.
- Ten health system customers of Kyruus are using its COVID-19 vaccine scheduling capabilities and have booked 100,000 appointments in the first month.
- The local paper profiles the way in which a Medical University of South Carolina student used Jvion’s technology to find patients at risk for COVID complications.
- Meditech offers customers access to its complimentary Quick Vaccination solution to reduce the burden of COVID-19 mass vaccination distribution.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.
































I generally follow AP Stylebook style guidelines: Do not use all-capital-letter names unless the letters are individually pronounced: BMW. Others…