EPtalk by Dr. Jayne 5/20/21

Since I’m no longer providing in-person clinical care, my schedule has a different level of flexibility and I’m trying some new things both personally and professionally. Today I enjoyed attending a medical school’s Grand Rounds presentation from the comfort of my bed, which was much nicer than being in a subterranean auditorium. I’ll be doing some travel and sampling the digital nomad lifestyle a bit as well as trying my hand at Locum Tenens coverage.
For HIStalk, I’ll be adding some interviews with women leaders and entrepreneurs in health IT. I’ve already identified a couple of potential candidates but am looking for suggestions. Drop me a note with your nominee and why they would make an interesting interview. I’ll start running them in June, so stay tuned.
Lots of chatter around the virtual water cooler this week about a Kaiser Health News writeup addressing parking charges for cancer patients receiving care. The article references a research letter in JAMA Oncology last summer that looked at parking fees at National Cancer Institute-designated cancer treatment centers. Although the idea of charging cancer patients to park while they undergo treatment is particularly odious, we should be looking at the broader idea of charging patients to park, period.
I recently had care at a major institution that has billions in its endowment, but can’t afford to allow patients to park for free. Given the preponderance of organizations getting on the facility charge bandwagon as a way to increase their bottom lines, one would think that parking should be part of those facilities. As a healthcare insider, I know that many organizations run on razor thin margins, but I would argue that if you can still afford to build marble foyers with fountains and landscaping, you should take a serious look at whether charging patients to park is the right thing to do.
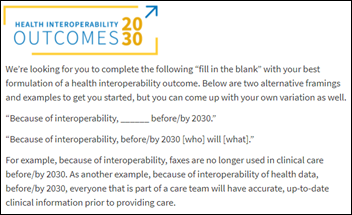
Kaiser Health news also ran a piece this week looking at patient reaction to having greater access to health data. Patient-side stories include patients who were anxious when seeing laboratory results without the benefit of a clinician’s explanation and those who felt offended or judged after reading physician notes. Another story mentioned a patient receiving biopsy results on the weekend, blindsiding both the patient and the physician with a cancer diagnosis. Organizations including the American Medical Association are encouraging adjustments to the rule, allowing delays for certain tests (such as biopsies) to allow physician annotation prior to release.
For some organizations, this change has not been an issue since they already provided access for more than 50 million patients. Others are creating reference guides for patients to better understand their results. My former employer is in violation, although most of the providers at the practice don’t realize that greater accessibility is now a requirement. It will be interesting to see what enforcement on this looks like.
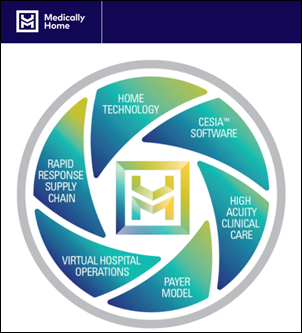
The last water cooler conversation piece was the recent JAMA Viewpoint editorial that offered suggestions for designing successful capitated payment models for primary care physicians. I agree with the seven design elements proposed by the authors (my favorite healthcare IT crush, Farzad Mostashari, MD included). However, in order for capitated contracts to succeed, we need better support for interoperability around healthcare data in order to facilitate patient care through home health, remote monitoring, and better coordination of specialist care.
Despite what the integrated delivery networks think, there are still a good number of independent physicians out there. As a family physician, I need easy access to all the information my referral specialists hold on my patients, whether we’re part of the same network or not. Despite information blocking regulations, large health systems continue to not play nicely with anyone outside of their network and patients pay the price, not only financially through duplicated services, but medically through poor care coordination.
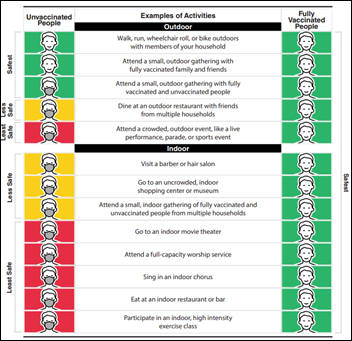
The Journal of the American Medical Association published a recent article that looked at whether COVID-19 vaccine registration websites were accessible to those with disabilities. The authors looked at 54 official websites in the US and compared them against the Web Content Accessibility Guidelines (WCAG) 2.0 and 2.1 guidelines. They found “suboptimal compliance” with the guidelines among the sites evaluated, with only two meeting the WCAG 2.1 standards. They call for greater availability of text-to-speech functionality to better meet user needs along with better use of color, contrast, spacing, and other presentation features to improve visual understanding.
Navigation challenges were also specifically called out in the analysis, with recommendations for improved titles, headers, labels, and links. They also recommended user testing that involves people with disabilities and ongoing evaluation as websites are updated. None of these findings are surprising to me, as I regularly have to call out technology developers for non-ideal use of color and contrast when they’re creating user-facing screens. Accessible UX design helps everyone, and I would encourage those companies that don’t have experts on staff to consider using consultants who can get the job done.
I had to break down and try to find a primary care doc recently and the whole process was only describable as a disaster. Most of the family physicians in my community aren’t accepting new patients and those that are taking new patients have a greater than six-month wait. I finally broke down and reached out to a colleague directly to see if he’d make an exception to the “no new patients” policy, which fortunately he did.
I had to play some phone tag with the office, and since this was an exception situation, the appointment line couldn’t book my appointment. Instead, they needed to me to speak directly with the physician’s medical assistant. However, they made me go through the full verbal COVID screening questionnaire before they would transfer my call, even though the appointment I was trying to book was for a month or two out. If they’re doing the verbal screening for every patient who calls regardless of what they are trying to book, it seems like a lot of wasted energy collecting screening information that will be long invalid by the time the patients arrive.
How is your institution managing COVID-19 screening in the new era of vaccines? Have things changed? Leave a comment or email me.

Email Dr. Jayne.





























Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…