Justin Dearborn is CEO of PatientBond of Salt Lake City, UT.

Tell me about yourself and the company.
I started with PatientBond as CEO in January of this year. Prior to PatientBond, I was CEO of Merge Healthcare from June 2008 through October 2015, when Merge Healthcare was acquired by IBM and formed the basis for Watson Health for a while until their next big acquisition. I took a pause after that in healthcare, went and did a few other things in different industries, and then found my way back to healthcare.
I took your 12-question Patient Classifier psychographic segmentation survey. What are health systems learning about using consumer insights in their outreach and messaging?
I saw you took the classifier, so thank you. You and I are both priority jugglers at a high rate. You fall into multiple categories, and then we segment you based on the highest category, and you are very high and I’m very high on the priority juggler spectrum of the model.
What a health plan, payer, physician group, or specialty pharmacy is trying to activate in their client, member, or patient determines how they start using the psychographics and segmentation platform. Ultimately it is to trigger and activate positive behavior, such as keeping an appointment, filling out a survey, or all the way to collections or the financial side. It is triggering that process.
What all of our clients and most health systems are starting to realize is that they need to treat their patients similar to a consumer. One size does not fit all. Some segments of the population react well to physician-based messaging, where your doctor wants you to do X, Y, and Z. That segment of the population will do that without any other prompting or any other pushing needed. But a large portion of the population that doesn’t react the same.
A lot of healthcare is messaging is towards the one segment. We dynamically personalize it based on what segment we’re speaking to. The customer doesn’t need to understand the concepts, but they are seeing the results in better engagement with the patient, more engagement, and getting across the spectrum of things from marketing outreach to medication adherence to really involved specialty pharmacy workflows.
It really depends on the workflow you are trying to achieve. But the bottom line is better engagement with your patient or member because you are speaking to them in a modality they want to use, in language they want to hear, and in words that they need to see to be activated.
Do providers ask their patients questions specifically to create a more accurate psychographic profile, or do they infer it from existing information?
Our system learns. We think you want to be communicated this way, in this frequency, and using these words. If it’s an ongoing communication path, our system will learn. We thought you would like text messaging and you need to see one message a day to activate this behavior, but it turns out now that one message a week in an email is better. We can learn from that and personalize the communication path based on that.
Health systems have done a great job, and are getting better all the time, at using AI to harvest their claims data. If it’s an existing patient, they have that data. They might have some socioeconomic data or social determinants of health data. If the health system has those components, we say, great, let us append the psychographic segmentation model to that – it will be even smarter, better outreach because you’re going to have historical data, which is informative for sure.
But what psychographics really gets to is the why and the how. It doesn’t focus on the historical. The historical can be informative, and there are certain things you can tell from a ZIP code or a salary that might impact payment ability, but really what the psychographics does is get behind the why and the how. This came out of Procter & Gamble and a number of high-quality, consumer-facing companies have used this for decades to segment consumers on a mass scale, as well as individual, and we can do both as well.
The classifier allows us to segment you with 91% accuracy. If we didn’t have that relationship, or if you were doing a marketing outreach to attract patients that you don’t know, we would take a national compiler’s database and append our model to it. That would be three times more accurate than chance on segmenting you properly, but it’s still not the number we get if you do the 12 questions.
Many people heard of psychographics in relation to Cambridge Analytica or Facebook collating a lot of data without user knowledge or permission to study their behaviors. Did these examples teach us that psychographics does or doesn’t work, especially in healthcare where the results would be used to improve the individual’s outcomes instead of trying to influence them for less-noble purposes?
I’ll start with the last piece of that. We believe in the health systems that we are working with. We believe in the payers. It’s really about activating positive behavior — making sure you take your medication, making sure you do your annual physical, or prompting you the best we can to get your colonoscopy. I think we would all agree that these are healthy behaviors. We’re not showing the data. In that case of Cambridge and Facebook, if the hospital did license the Facebook data — which we did at Tribune Company, for instance — that would still be separate data. That would go more to the social determinants of health datasets, and we could still use that and append psychographics to that.
To the first part of the question, part of our challenge with PatientBond has been awareness. Since I came in with the Series C investment round, we have been doing more on the outreach, more brand-building. We have started engaging with KLAS and Advisory Board and things like that. Frankly, the company didn’t have the budget to do it in the past. Half of our engagements are evangelizing, so a couple of calls will involve explaining the psychographics model, the history and genesis of that, how we get the data, what the clinical efficacy is, etc.
Usually light bulbs start popping on. The client, the health system or payer, will start coming up with use cases. Could you do this? How do we operationalize it here? It’s a little bit of, I’ll say, free consulting and evangelizing. But once we get into a pilot mode, it pretty much takes care of itself. Then someone from the marketing or strategy group typically owns the project.
Absolutely awareness is still a challenge, but we’re working on that daily. There was a great paper put out by McKinsey about a month and a half ago that mentioned psychographics a number of times and the way they engage patients more effectively. That was unprompted by us. They found us and did the research and didn’t call us on it. Same with the Advisory Board. They put out a good case study with TriHealth and we were not contacted, but we were named. They both had some great results. So it really is about awareness.
Last year, of course, it was difficult to get mind share with the obvious situation at hand with the pandemic. This year is around awareness of PatientBond and the mission. It’s hard to say in healthcare IT. I was at Merge Healthcare and we had great products, but it’s hard to differentiate yourself. Most of the segments in healthcare are pretty crowded with vendors, but I can say there is no other company doing psychographic segmentation modeling and has our platform.
There’s a lot of M&A on the AI side that do claims data analysis. Systems will recommend what they think would be the outcome based on historical, which is good stuff as well, but really nobody uses psychographics. A lot of the situations we are in are not competitive, but involve evangelizing and explaining in the first couple of calls.
Are health systems reluctant to apply marketing techniques to patient relationships that are more intimate than just consumer awareness campaigns? Or have their marketing folks not been involved and that will change with the new emphasis on consumerism as overseen by C-level executives?
I truly believe it’s the latter. It’s just coming of age. I’ve spent 10 years in healthcare and I can remember growing up that you didn’t see marketing from health systems, your doctor, or your hospital. I grew up around Northwestern Hospital and they didn’t advertise, but they do now. They have marketing budgets. They have data scientists.
That has evolved for the better. How to engage. How do people want to be communicated with, like text messaging versus email or IVR? Or, do you need to talk to a human being? We are informing them on how to best communicate.
That has been going on in CPG, consumer packaged goods, for 30 years. CPG used it effectively. Proctor & Gamble are masters at consumer marketing, but they don’t necessarily have the one-to-one relationships that can be built at health systems. You’re not as intimate when you’re buying Tide detergent, so when they are applying psychographics to something like Tide, it is more of a carpet bombing. They’ll profile an area and say, this area is over-indexed for priority jugglers, and here’s the messaging, here’s the labeling, and here’s what we need to do to resonate here.
But with health systems, it is truly one to one. Once they are a member or patient client, it’s one to one, and we truly personalize it for each one. That’s a huge, huge upside and more productive.
I truly believe it is awareness. In none of the calls that I’ve been on in the past six months — and there have been a lot — did the chief marketing or chief strategy officers not get it, not believe in it, or decide that “we’re good with what we’re doing.” It’s more of, this is really intriguing,. How would we operationalize this? How does this work with our CRM? How does it work with our EMR? There’s has been a lot of great commentary, feedback, and follow-on loops.
I would say it’s coming fast. We probably would have seen a bigger uptake last year but for the pandemic, but as hospitals get back to normal a little bit, it is all about treating the patient as if they have choices, which they do. Probably this year or maybe next year, people will be paying 50% out of pocket for their total healthcare costs. We’ve been talking about it for 10-15 years, but the patients will be in charge. They are starting to make decisions somewhat based on price, how they like doing business, and how they like the relationship. That has been evolving for a while, but it’s going to cross the 50% threshold here very soon, and patients will act like consumers. It’s coming and it’s going to come fast.
We’re seeing that increasing COVID-19 vaccine uptake isn’t a simple as informing people who are uninformed, so now we are trying to understand their beliefs and nudge them accordingly. Has that raised awareness that targeting patients who meet some criteria and hitting them with cookie-cutter messages probably won’t work?
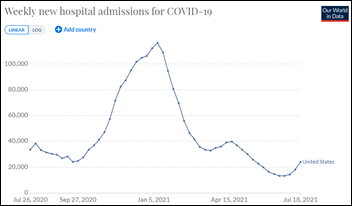
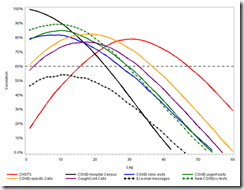
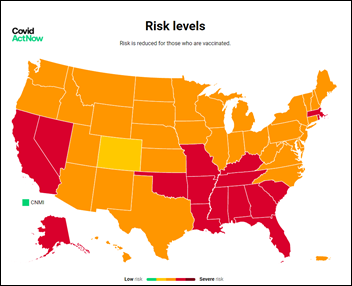
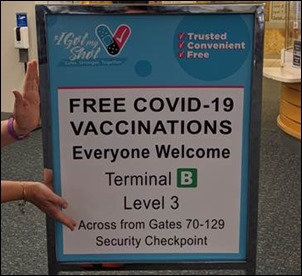
That’s a great analogy. We surveyed 4,000 people with 400 questions around motivation for vaccination. We came out of that with a ton of data. It is coming to light right now that you can’t treat everybody the same. It’s not all about just being an anti-vaxxer. There are other motivations and other things you can point out, and it’s information. Some people need more information. Some need to have their clergy talk to them about it. It’s all starting to come out as we hit the wall. We predicted four months ago that we would hit the wall in June at about 65%. We were spot on. We had this great data built into the platform as how to basically get people who are close over the hump and off the fence.
We have been trying to get that data out there. The challenge is who ultimately is motivated and incentivized to get people who aren’t vaccinated to get vaccinated. Now it has become more of a public service. For health systems, it’s for the common good, but do they even have a relationship with people who aren’t vaccinated their community? Not always. Early on, employers were being hands off because it was a hot potato. It was hard for us, and it still is hard for us, to find a group that has the incentives to get behind this.
We are willing to share the data and share our insights on how we feel that you can move the needle on that. But that has been a challenge because there has been no ownership. The federal government is supportive of it, but other than making it free, there’s really not much else. To your comment, we are absolutely, definitely informed that you can’t treat everyone the same. You can’t have one billboard. That’s not going to resonate with all the groups.
What will the company’s strategy be over the next few years?
It’s about marketing awareness. We’ve tripled the go-to-market team, the sales team, in the first six months of the year. We’ll grow 100% this year, and I think we’ll continue that path. The really attractive piece for me coming in was that we have a somewhat “friends and family” board of directors. There’s really only one entity of professional money, which is First Trust, who has a legacy investment and is a great partner. The rest are family office and individual. It allows me to manage the company for growth and to see this thing through.
We have a huge runway ahead of us. I don’t have any investor pressure. There’s no timeline. We have enough of a platform, and it keeps growing weekly, that we can remain private and self-funded for eternity. Eventually we’ll come to a decision point in a couple of years about an IPO or something else, which is the natural evolution of an early-stage growth company, but the good piece for me was not having external pressure from traditional venture capital investors.
Comments Off on HIStalk Interviews Justin Dearborn, CEO, PatientBond
































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…