Shawn DeWane is CEO of TransformativeMed of Seattle, WA.

Tell me about yourself and the company.
TransformativeMed focuses on the clinical workflows of physicians and nurses. Healthcare is a team sport and COVID-19 has made this a focal point. We are looking to bring a revolution to healthcare IT by delivering smart technology, smart algorithms, and the organization of clinical information in an intuitive manner so that clinicians can effectively and efficiently impact patient lives with a strong patient safety aspect.
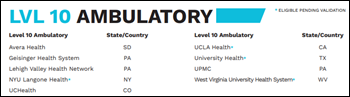
We got our start in rounding and handoffs, then moved into other smart care capabilities, such as diabetes. The focus of our company has always been around research and development, done in partnership with our customers. Some of those customers are among the most prestigious in the country, so we have some great thought leadership as a result. Clinician satisfaction is high, in the 95th percentile range. Our implementation experience is exceptional. The product is sticky and clinicians love it. We are in 26 health systems around the country and we have one overseas. We have over 170 hospitals that use the products. There are a lot of hospitals that we are not in and a lot of beds that we’re not servicing at the moment, so we have a lot of opportunity, a lot of green space in front of us.
I grew up in rural Northern Illinois in a Midwest farmland culture that emphasizes hard work and fair dealings. I’ve hade a successful career in healthcare IT and technology and have developed a system of sorts that I can assess, grow, and scale businesses with great talent. My focus has always been around relationships and a fundamental commitment to delivering success to customers and my teams. Some of the key bodies of work that are most significant for me in the past are a 13-year run with IDX, then McKesson, and most recently with Hayes. My wife of 37 years and I live in the Chicagoland area. We have three great kids, all adults and on their own.
How would you describe the relationship between Cerner and Epic and companies that develop embedded or connected apps that extend the capabilities of their core EHR products?
I’ve had a great deal of experience with large enterprise EMR production systems through McKesson and IDX. They typically can’t handle the level of precision a clinician needs for problem-based care. With the changing landscape that COVID brings to the table, it makes it even harder for an EMR system to be both nimble and effective in addressing patient care. Problem-based care and the precision of what the clinician needs is at the heart of why a company like TransformativeMed exists. Recently a CMIO of one of our customers, a large health system, told us that we come in with the eyes of a clinician and know exactly what they need. That’s really what it boils down to.
User testimonials on your website talk about how your product improves clunky EHRs, provides financial benefit, and increases clinician satisfaction. Do those comments get back to the EHR vendors in highlighting seeming shortcomings in their products?
Some of that probably does happen. My experience with large enterprise production systems do just that. It’s hard for them to be nimble and focused on the moment and the issue when you’re standing over a patient, whether you’re a nurse or a physician. The ability of a system to be able to gather information, suggest a treatment of care, and then document that back into the EMR — that level of efficiency in a fluid situation is difficult for a large production system to handle. At some point it is what it is, but we make the EMR what the user thought they should have gotten.
How much of clinician EHR dissatisfaction and burnout is caused by plain-vanilla implementations that avoid personalization for individuals and clinical specialties?
Each specialty has its own angle that they’re coming at in terms of the problem that the patient presents. You have to have smart care algorithms to address the unique needs of the specialty and by type. Not just the needs of the physician, but of the nurse as well. The cumulative nature of what happened, what is presented in the moment, what to do, and then the further documentation along the lines of that specialty is what TransformativeMed does, which is what users like the most.
Some issues are time-based, where I get 15 minutes extra a day or 30 minutes extra a day or two hours extra a day back into my life so I can see more patients. Bed capacity management, especially these days, is chronic. How do I treat the patient as effectively as possible and move them into a discharge status so I can make that bed available to another patient? All of that is expedited and made more efficient when you have specialty-based algorithms to provide them the information they need.
Does the underlying architecture of EHRs support real-time capabilities and user personalization?
EMR systems are sound technology to store batches of information like lab data, nurse documentation, or physician documentation, but it’s gathering up that into an efficient way to present those findings to the provider at the time of care for the patient. That efficiency of gathering that and presenting an algorithm for care is where TransformativeMed fits in. The ability to gather effectively, present it in a smart manner, and then — and this is the main thing — to be able to document back to the EMR while in the event, the moment with the patient. That’s the part that creates the efficiencies.
How much of the company’s efforts will be driven by which EHRs you work with and how you work with them?
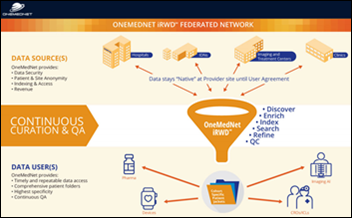
We are embedded at the EMR level through FHIR API kind of technology. It’s important to get that connection and linkage done correctly. It’s also important to make sure that all of the rich features and functions that the clinicians need are intact. We have some partnerships with clients to make sure that from a qualitative point of view, everything works the way it should. We have some other partners lined up to make sure that that happens.
Whether it’s Epic or Allscripts, the quality of the connection and delivery of the function for efficient problem-based care delivery are the focus. We are on that journey, it’s moving along pretty well, and we’re going to continue that journey. We are going to take a more qualitative approach and make sure that it’s done right.
Is it difficult to create or maintain a brand identity when clinicians may not be able to tell which parts of the system were provided by the EHR vendor and which parts came from TransformativeMed?
Because the embedded nature of the solution, the clinician really doesn’t know that they are in TransformativeMed, because it is just brought in from the Cerner screen or the Epic screen. There’s a seamless nature to it that is very attractive to clinicians.They don’t have to toggle in and out of one system to another.
From a branding point of view, CORES is the brand title. Physicians who have used CORES want to use it again. If physicians are thinking about getting a solution that CORES addresses, the referrals are made. We get inbound interest from clinicians who want CORES because their colleague used it at a different health system. There’s a seamless usage of that through the UI, but the CORES brand is very strong out there.
Has their been interest in making the company part of a vendor or consulting organization?
Valuation and general value are dependent on the revenue you have coming in, your customer satisfaction, and the breadth and depth of products that you have. Right now our focus is to grow the company in a sustainable manner. If our customers are happy, they will stay with us and our revenue will continue to grow. We will have to see from there.
Where do you see the company’s recent work with the VA in Puget Sound leading?
We are super excited and honored. I’m very excited to be able to have an impact on the care of veterans. It’s a nice mission for our company. We have a great culture, but it’s a special honor to be able to do this.
This initial site will go fairly rapidly. We should have some pretty good results in the next two or three months. With that said, as we make progress through the rest of the VA, we will have some great use cases as a result. We are looking for other avenues with the government as well. It’s going great so far and we expect great results and are looking forward to further use of the product throughout the VA.
How will the VA and your other customers determine the impact of implementing your product?
We always do a compare and contrast of the situation before we were installed and afterwards as a use case. We document what the problem was, what we did, and what the results were. We will be doing the same thing with the VA.
The specific aspects that we will look to impact here will be around rounding and handoffs, and also with diabetes care and management for both the physicians and the nurses. They will be permeated throughout the VA. We expect to chart and document those results.
In the short term, we will be able to coordinate care better. As I mentioned before, healthcare is a team sport. Statistically, you’ll see in a typical episode that maybe 50 clinicians of one sort or another are involved in a patient’s care. We’ll be able to coordinate that better. We’ll be able to hand off that information better and they will use their time more efficiently.
On the diabetes side, diabetes care is fluid and it’s conditional depending on a number of factors. We will be able to coordinate that better, especially with the CMS regulations that are coming out around performance and generally regulating diabetic care. We will be positioned to affect the diabetic care of the veterans that we’ll be serving.
Where do you see the company’s future over the next three or four years?
We are focused on adding new customers, keeping our customers happy as they typically are while expanding the footprint in our customer base. We are going to look to a lot of revenue growth, a lot of expansion into both the government and international markets. We will invest in additional product development, research and development for new modules to help support our customers. We are looking at not just solutions for residents, hospitalists, or endocrinologists, but a number of other areas to continue to expand our footprint.

























Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…