Arcadia

Booth 2711
To arrange a meeting, click here.
Contact: Jasmine Gee, VP of Marketing
jasmine.gee@arcadia.io
Arcadia (arcadia.io), the leading population health management and health intelligence platform, is hosting several informative forums focused on how to revitalize your organization’s care and research with data-driven insights.
Lunch and Learn: Data science for clinical impact – building a predictive analytics ecosystem. Arcadia’s director of data science, Michael Simon, PhD, will help attendees think through the best way to implement predictive analytics for their populations — from the use of a massive, diverse, longitudinal data asset to modern approaches to modeling patient risk to a case study on the development of a predictive algorithm for behavioral health. Thursday, March 17, 11:15 –12:15, Room 203B. Registration required – request a lunch invitation here.
Forum: Accelerate value-based performance — even when the low-hanging fruit is gone. Hear from leaders at Rush Health, Summit Health, Castell, and other pioneering organizations via case studies and interactive panel discussions. Wednesday, March 16, 11:15 –12:15, Room 202A, and 3– 5:30, Room 202A. Attendance limited to value-based care leaders – request an invitation here.
Forum: Achieving interoperability takes more than an envelope: Leaders from KLAS, Arcadia, Rush Health, Castell, and IMSNY will share strategies and how to void interoperability “gotcha” moments for effective, outcome-driven information-sharing inside and outside your walls. Tuesday, March 15, 11:15 –12:15, Room 202C and 3– 5:30, Room 203B. Attendance limited to information technology and analytics leaders – request an invitation here.
Bamboo Health

Booth 4115, Interoperability Showcase Booth 8240-75
Contact: Alison Matthiessen, senior communications manager
540.230.9021
Bamboo Health will present and exhibit our suite of digital health solutions for interoperable care coordination at HIMSS. As part of the HIMSS Interoperability Showcase, Bamboo Health Vice President, Strategy & Corporate Development Jitin Asnaani will present a session on “Harnessing the Power of Interoperability to Cultivate Whole Person Care Collaboration Across Providers, Patients, and Payers” on Tuesday, March 15 at 2:45.
Visit the Bamboo Health booth 4115 to learn more about our progress against the behavioral health and substance use crisis through our Pings solution for real-time notifications whenever patients experience care events; OpenBeds provider-facing behavioral health solution for health systems, health plans, and state governments; and NarxCare analytics application and clinical decision support tool. Visit bamboohealth.com to learn more.
Giveaway: Visit Bamboo Health booth 4115 to participate in our raffle for a chance to win an Oculus VR headset!
Biofourmis

To arrange a meeting, contact Sandeep Pulim.
Contact: Sandeep Pulim, medical director
sandeep.pulim@biofourmis.com
617.334.5441
Biofourmis is a global health technology company focused on leveraging software and data science to deliver virtual care and develop novel digital therapies. Their Care@Home solution utilizes medical-grade wearables to continuously collect patient data, which is analyzed by Biovitals, Biofourmis’ clinically-validated, AI-powered, predictive analytics engine. Additionally, the company discovers, develops, and delivers clinically-validated digital therapeutics to support payers and providers.
Bravado Health

Booth 5349
Contact: Shane Andreasen, VP of Marketing
561.232.9720
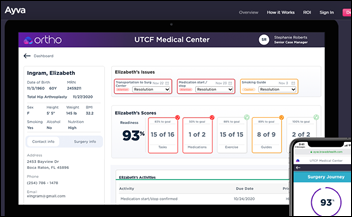
Visit Bravado Health at booth 5349 or schedule a meeting to learn more about Ayva, a patient engagement platform for every care journey.
Bravado Health’s award-winning designers created the dynamic patient engagement platform, Ayva, to simplify the care journey from preparation to recovery across the entire spectrum of surgeries, procedures, and disease management. Ayva packages care plans, educational videos, messaging, remote patient monitoring, and more into an accessible, Web-based experience that’s proven to engage patients, improve outcomes, and increase patient satisfaction. Ayva shares engagement data with the patient’s care team, helping clinicians make more well-informed decisions.
Clearsense

Meeting Place MP9101
Contact: Leann Williams, marketing manager
lwilliams@clearsense.com
904.334.7500
Join our Lunch and Learn on “Advanced Analytics Empowering Change: Transform Your Data into Actionable Results in Real Time.” Join Michelle Reed, product manager of AI and analytics, and Patrick McDaniel, solutions engineer, strategy of AI and analytics, for this interactive session and learn how the Clearsense Data Platform takes your data to the next level with predictive analytics. Clearsense will present a use case around renal failure by creating a patient grouping and using advanced analytics tools.
Discover how powerful advanced analytics can be when in the hands of everyday users, including domain experts, clinicians, analysts, and researchers. This innovative, data-first approach offers the flexibility to learn and adapt. Dive into the functionality of the feedback loop, ask questions regarding a variety of use cases, and see real-time changes you can make today to impact tomorrow’s outcomes. Lunch and refreshments will be served. Registration is required to attend. Please visit https://bit.ly/3uR1WRp to learn more.
CloudWave

Booth 3633
Contact: Christine Mellyn, director of marketing
cmellyn@gocloudwave.com
781.636.8169
Visit CloudWave at HIMSS22 to learn how we help healthcare institutions architect, build, and integrate a personalized solution using managed private cloud, public cloud, and cloud-edge resources to guarantee uptime, easy access, and strong security.
Join us for our brief educational presentation sessions at 11, 1, and 3 each day on the exhibit hall floor, in booth 3633, and earn a chance to win a pair of Apple AirPods. Topics include “Enterprise Imaging in the Cloud,” “A New Approach to the Cloud Edge,” and “The Value of Immutable Backups.”
CloudWave’s team will be available to lead conversations around the relentless data tsunami that can either transform care for the better or threaten existing infrastructure if not handled correctly. Whether you want to operate your IT systems in your data center, in the cloud, or a combination of both, CloudWave can help. Learn how we deliver EHR and enterprise cloud services to over 235 healthcare organizations in six countries.
Current Health

Booth 4859
Contact: Lauren Levinsky, VP of marketing
lauren.levinsky@currenthealth.com
650.799.7315
Current Health offers an enterprise care-at-home platform that enables health systems to deliver safe and effective care from the comfort of a patient’s home. We bring together remote patient monitoring, telehealth, and patient engagement into a single, flexible solution that allows organizations to manage all patient populations within one platform. With our recent acquisition by Best Buy, we’re excited to be able to leverage their best-in-class supply chain, logistics, and in-home support to help deliver that last mile of care in the home.
Visit our booth for an end-to-end demo of our solution, get a first look at our exciting new product features, and meet members of the Current Health and Best Buy team.
Diameter Health

To arrange a meeting, visit diameterhealth.com/events.
Contact: Josh Salazar, marketing manager
jsalazar@diameterhealth.com
765.409.4515
Diameter Health upcycles raw clinical data into a standards-based, interoperable asset using Fusion, our FHIR-enabled technology engine. Our comprehensive, automated data integration, normalization, and enrichment technology delivers high-quality data to streamline workflows, inform decisions, and accelerate interoperability, at scale.
Divurgent

To arrange a meeting, contact Joe Grinstead.
Contact: Joe Grinstead, principal
joe.grinstead@divurgent.com
214.533.9313
Divurgent won’t be exhibiting, but we’re eager to meet up! We’ll have some of our most senior subject matter experts on technology, digital, and data innovation. Rather than giveaways, we’re opting for meaningful conversations – if you’re interested in solving problems and accelerating your business priorities, we’re here for that!
Divurgent is a solutions provider focused on what matters most to our client partners. We disrupt the typical value equation by using data-infused, flexible, and scalable solutions that demonstrate and quantify value for our partners.
Ellkay

Booth 5645
Contact: Auna Emery, VP of marketing
auna.emery@ellkay.com
520.481.2862
As a nationwide leader in healthcare connectivity, Ellkay has been committed to making interoperability happen for nearly 20 years. Ellkay empowers hospitals and health systems, providers, diagnostic laboratories, healthcare IT vendors, payers, and other healthcare organizations with cutting-edge technologies and solutions. Ellkay is committed to ongoing innovation, developing cloud-based solutions that address the challenges our partners face. Our solutions facilitate data exchange, streamline workflows, connect the care community, improve outcomes, and power data-driven and cost-effective, patient-centric care. With over 58,000 practices connected, Ellkay’s system capability arsenal has grown to over 700 EMR/PM systems across 1,100+ versions. To learn more about Ellkay, please visit Ellkay.com.
Start your morning off right by grabbing a complimentary cup of coffee with Team Ellkay the first hour each day at booth 5645. Ellkay will also host Happy Hour on Tuesday, March 15 and Wednesday, March 16 from 4:00-6:00. Stop by to discuss connectivity, interoperability, and strategies to reach your data management initiatives. And, of course, our popular LKHoney will be available at the booth!
Everbridge

Booth 821
Contact: Cristin Carr, senior marketing programs manager, healthcare
cristin.carr@everbridge.com
781.859.4129
Trusted by more than 6,000 global customers including 1,500 hospitals and healthcare organizations, the Everbridge Critical Event Management platform helps physicians, nurses, and emergency response teams overcome the challenges of clinical care communications by simplifying workflows, leading to faster clinical responses and improved patient outcomes. Similarly, during critical events such as active shooter situations, severe weather conditions, or critical business events including IT outages or cyberattacks, the CEM platform automatically gauges the severity and context of the situation, quickly activating the right staff and mitigating the risk of a disruption in hospital operations and patient care.
Stop by our booth or schedule a meeting with us here, and enter to win an Apple Watch. To learn more about CEM, visit everbridge.com.
EVisit

Booth 1909
Contact: Vanessa Sierra, VP of marketing
vsierra@evisit.com
EVisit, the leading enterprise care delivery platform built for modern health systems and hospitals, will announce the launch of EAnalyze at HIMSS22. EAnalyze is a powerful reporting dashboard that provides EVisit customers with valuable data insights, including usage, patient wait times, virtual visit traffic, duration and drop-off rate, and other key adoption metrics, prompting proactive changes that can improve the patient consumer experience and reduce costs. In addition, EVisit plans to reduce the burden on providers by integrating the most advanced medical diagnosis API into its end-to-end platform.
To learn more, please plan to attend: “Care Navigation: Getting Patients to The Front Door.” Presenter: Dave Lovecchio, product manager, EVisit. 1:30 on March 15 and 16. EVisit booth 1909
First Databank

Booth 3659
Contact: Steve Normile, director of strategic alliances
snormile@fdbhealth.com
503.598.9739
New Solution To Be Announced: FDB will launch an industry-changing new solution that touches every major segment of the healthcare industry on Tuesday, March 15.
FDB PatientFirst Solutions Yield Benefits: FDB will share how solutions within our FDB PatientFirst suite are delivering targeted and patient-focused context and drug information to help clinicians make precise, evidence-based decisions:
- How to Access Patient-Specific Medication Guidance When It Matters Most with FDB Targeted Medication Warnings.
- How to Leverage Actionable Insights to Boost CDS Effectiveness with FDB CDS Analytics.
- How to Provide Evidence-Based Drug-Gene Guidance Within the Workflow with FDB Pharmacogenomic CDS.
- Presentation: Anna Dover, PharmD, BCPS, director of product management with FDB, and Harvard-trained medical geneticist Marsha Fearing, MD, MPH, MMSc, with Meditech, will discuss why and how genomics is about to change healthcare in the near term. Meditech booth 3311, Tuesday, March 15 at 2 and Wednesday, March 16 at 11:30.
Additional Solutions:
- How to Tune Medication Alerts with FDB AlertSpace.
- How to Address Patient Medication Adherence and Understanding with Meducation.
- How to Combat Supply Chain Disruption with FDB Prizm.
Reception: Attendees are invited to attend FDB’s reception at our booth, 3659, for conversation and prizes on Wednesday, March 16, from 5-6. Co-hosted by FDB, Zynx Health, and MCG. Complimentary gourmet popcorn gift to all attendees Drawing for $1,000 Amazon gift card.
Fortified Health Security

Kiosk 300-26 in the Cybersecurity Command Center
Contact: Judy Cooper, director of marketing
jcooper@fortifiedhealthsecurity.com
615.600.4002
Fortified Health Security is Healthcare’s Cybersecurity Partner – protecting patient data and reducing risk throughout the healthcare ecosystem. As a managed security service provider, Fortified works alongside healthcare organizations to build tailored programs with high-touch engagements and customized recommendations that maximize the value of investments and result in actionable information to help reduce the risk of cyber events.
Stop by kiosk 300-26 in the Cybersecurity Command Center to find out how we have become healthcare’s best cybersecurity partner.
Medhost

Booth 3858
Contact: Holly Evans, SVP of customer success & marketing
holly.evans@medhost.com
615.293.0714
Medhost, a leading EHR and healthcare IT solution and service provider, will showcase key offerings from their enterprise, departmental, and digital health solutions catalog at the HIMSS22 Annual Conference and Exhibition in booth 3858, March 14-18.
In addition to their full range of services and solutions, Medhost will showcase new offerings that will enhance hospital end-user experiences and help streamline hospital workflows. The three new solutions include but are not limited to Medhost Anesthesia Experience, Medhost Mobility Physician, and Medhost Cloud-Based Analytics. Built to complement the perioperative platform, Medhost Anesthesia Experience is a comprehensive, clinician-driven application that supports anesthesia providers. The mobile solution, Medhost Mobility Physician, provides a complete view of patients’ charted data and includes a HIPAA-secure messaging tool, all from a handheld device, offering physicians greater digital freedom and flexibility in their workflows. Medhost Cloud-Based Analytics is an out-of-the-box, browser-based analytics product that adds simplicity to capturing a holistic view of a hospital’s essential performance metrics with drill-through capabilities initially in financials, revenue cycle, and payor performance. Learn more about our solutions by visiting us at booth 3858.
Medicomp Systems

To arrange a meeting, visit: medicomp.com/himss22/ or email himss@medicomp.com.
Contact: James Aita, director of strategy & business development
jaita@medicomp.com
647.207.0080
Medicomp will showcase innovations in clinical usability and documentation workflow improvement, including clinical intelligence for EHRs to mirror the way clinicians think, enhanced FHIR/interoperability tools to make sense of incoming data by problem in health systems, breakthroughs in speech and NLP, taking “freetext” to structured data, and improvements in real-time compliance at the point of care.
Meditech

Booth 3311
Contact: Jason Patnode, marketing manager
jpatnode@meditech.com
781.774.5746
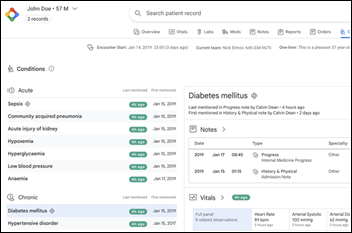
Meditech has driven EHR innovation during every stage of the industry’s evolution. Today, we’re helping healthcare organizations around the world expand their vision of what’s possible with Meditech Expanse. Meditech’s Expanse EHR delivers native, cloud-based mobility that keeps providers connected to each other as well as to their communities. See why KLAS rates Meditech Expanse the #1 EHR in three segments and a Top Performer in three others, including Overall Software Suite.
Stop by Meditech booth 3311 to speak with fellow clinicians and Meditech executives, or to catch a demonstration of our latest solutions, including Expanse Genomics, Expanse Care Compass, Expanse Patient Connect, and Expanse Ambulatory — now available to independent physician practices. You can also find us at the Interoperability Showcase and CMIO Roundtable, which we will be moderating.
Nordic Consulting

Booth 3965
Contact: Gwen Cantarera, marketing director
gwen.cantarera@nordicglobal.com
484.678.0264
Interoperability continues to be top-of-mind across the healthcare industry, and Nordic would like to help you connect the dots to create a pathway to interoperability. Stop by our booth and let’s talk about the challenges you face with interoperability. With our deep expertise across all major EHR systems, we take a platform-based approach to enable connectivity. It’s time to turn your technology into an enabler, not a roadblock.
PatientBond

To arrange a meeting, contact Todd Helmink.
Contact: Todd Helmink, SVP of strategic partnerships
todd.helmink@patientbond.com
312.391.4233
The PatientBond patient engagement platform leverages healthcare consumer psychographic segmentation and machine learning to target interactions based on personal motivations and channel preferences that drive patient behaviors, delivering truly personalized, multi-channel engagement that drives better outcomes for health systems, payers, and life sciences vendors. We are the opposite of the one-size-fits-all approach to driving patient and member behavior.
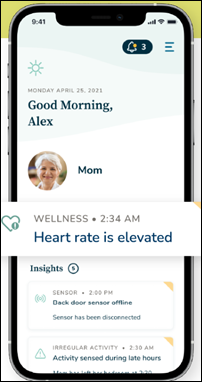
Quil Health

To arrange a meeting, contact Ashley Stevens.
Contact: Ashley Stevens, VP of provider sales
sales@quilhealth.com
Quil is the digital health joint venture between Comcast NBCUniversal and Independence Blue Cross. We help people organize and navigate their health in partnership with their providers, health plans, and loved ones. We’re shaping the future, using technology to personalize and transform the experience of navigating health and care. The Quil solutions model best practices from the entertainment industry to revolutionize the way providers, patients, and loved ones are supported throughout their care journeys leveraging Quil Engage, the care engagement platform for health systems and patients.
Meet our team at HIMSS to get a live demonstration of the care engagement platform that informs, guides, and activates patients in their care, in partnership with their providers, payers, and loved ones. VP of Provider Sales Ashley Stevens will be taking meetings throughout the event to discuss Quil Engage and share demos of our patient engagement platform.
ReMedi Health Solutions

To arrange a meeting, contact GP Hyare.
Contact: GP Hyare, managing director
g.hyare@remedihs.com
281.413.8947
ReMedi Health Solutions is a nationally-recognized, physician-led healthcare IT consulting firm specializing in peer-to-peer, physician-centric EHR implementation and training. We’re a clinically-driven company committed to improving the future of healthcare.
Our Physician Executive team is attending HIMSS to connect with fellow industry members and friends, and share more about our virtual solutions that have generated a major impact for our healthcare partners. Feel free to reach out and schedule an EHR strategy session with our team during the event.
RxRevu

To arrange a meeting, contact Ryan Smith.
Contact: Ryan Smith, SVP of business development
ryan.smith@rxrevu.com
440.708.3683
RxRevu will be at HIMSS to talk care access and how we help providers access reliable data at the point of care to make informed decisions. Join us on March 16 at “The Use of FHIR to Accelerate Innovation in Healthcare,” a panel moderated by Cerner that features our CEO with Microsoft and MU Health Care panelists. We’ll also discuss RxRevu’s solutions at the Cerner booth on March 15 and 16.
Sphere

Booth 1733
Contact: Ryne Natzke, SVP of growth & strategy
rynen@spherecommerce.com
657.383.7967
Sphere will showcase its digital-forward TrustCommerce end-to-end patient payments platform at HIMSS22, highlighting the solution’s new digital wallet support within Epic MyChart, and its expanding network of digital healthcare solution partners. In addition, Sphere will demonstrate new Advanced E-Billing and collections capabilities within its Health IPass platform. Stop by Sphere’s booth to enter to win an Apple Watch.
To learn more, visit trustcommerce.com/verticals/healthcare/.
Tegria

Meeting Space 9417
Contact: Kevin Kutz, VP of public relations & external communications
kevin.kutz@tegria.com
Tegria provides consulting and technology services to help organizations of all sizes humanize each healthcare experience. Founded by Providence, with teams throughout the United States and internationally, Tegria is comprised of more than 3,500 colleagues who help their customers integrate technology, transform operations, accelerate revenue, and optimize care. We meet you where you are in your journey to transform healthcare. Our team is ready to listen.
Come and meet with the Tegria team at meeting space 9417 located in Hall F. For all inquiries, please reach out to Kevin Kutz.
We invite you to meet Tegria experts at their presentations on cloud strategy and patient access, growth, and retention. Breakfast Briefing: Thursday, 7:15-8:15. Topic: EHRs to the Cloud: Lessons from the Field. Speaker: Chad Skidmore, VP of managed services, hosting & infrastructure. Location: Room 203C, Orange County Convention Center.
Industry Solution Session: Thursday, 8:30-9:30. Topic: Patient Access Growth and Retention. Speakers: Rodina Bizri-Baryak, director of patient access and technology, and Emily Tempels, director of patient access. Location: Room W208C, West building of the convention center.
Lunch & Learn: Thursday, 11:15-12:15. Topic: EHRs to the Cloud: Lessons from the Field. Speaker: Chad Skidmore, VP of managed services, hosting & infrastructure. Location: Room 203C, Orange County Convention Center.
TigerConnect

Booth 5959
Contact: Betsy Berken-Zaslav, senior content & event manager
bzaslav@tigerconnect.com
954.579.3934
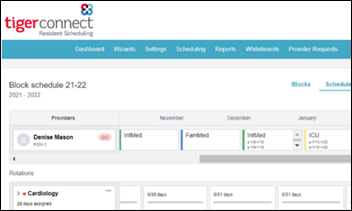
TigerConnect offers the healthcare industry’s most widely adopted and integrated communication platform, bringing together all aspects of care collaboration, physician and resident scheduling, patient engagement, and alarm management into a single, scalable, and mobile solution. HIPAA-compliant and HITRUST-certified, TigerConnect delivers 99.99% verifiable uptime and is trusted by more than 7,000 healthcare organizations.
Stop by the TigerConnect booth for demonstrations of how the platform integrates with EHRs and other systems to unify communication, streamline workflows, reduce costs, and improve patient outcomes. In addition to demos of its solutions, TigerConnect is offering pens, sunglasses, blue light blocking glasses, and bags to carry all your additional HIMSS giveaways!
TransformativeMed

Booth 3224
Contact: Robert Kerzman, chief growth officer
robert.kerzman@transformativemed.com
331.223.7840
TransformativeMed harnesses the data in your EHR to create an intelligent digital workspace that dramatically improves the usability of EHRs, with specialty-specific and disease-specific workflows embedded within the EHR.
The Cores Work Manager Platform, Cores Notify, and Cores Diabetes securely synchronize clinical workflow, tasks, alerts, notifications, and messages to harmonize the care team and create seamless communication across all care providers, using any device, including mobile. We believe your EHR should work the way you always thought it would. Visit us at booth 3224 to learn more.
Upfront

Booth 6545
Contact: Patrick Dienes, VP of sales
pdienes@upfronthealthcare.com
504.214.8169
Upfront delivers dynamic, digital care navigation to improve patient experience, increase necessary visits, reduce no-shows, and improve population health performance. Its flexible, omnichannel communication capabilities, combined with personalized patient content and calls-to-action, eliminate common barriers to patient engagement and enable Upfront to support a nearly unlimited number of use cases and deliver a world-class patient experience while driving a significant return on investment for client partners.
Visage Imaging

Booth 921
Contact: Brad Levin, GM of North America
blevin@visageimaging.com
540.454.9670
Visage Imaging is a global provider of enterprise imaging solutions that enable PACS replacement with local, regional, and national scale. The Visage 7 Enterprise Imaging Platform is proven, providing a fast, clinically rich, and highly scalable growth platform deliverable entirely from the cloud or on-premise. Visage 7 supports the simplicity of a One Viewer philosophy that enables diagnostic, clinical, specialty, research, and mobile imaging workflows from a singular platform. Visage 7 also offers modular scalability and future-proof flexibility with enterprise workflow (Visage 7 Workflow), vendor-neutral archive (Visage 7 Open Archive), and artificial intelligence (Visage AI Accelerator) solutions, all 100% native. Visage 7 can also be experienced in the Amazon Web Services booth 1041.
Zen Healthcare IT

To arrange a meeting, contact Dan Benson.
Contact: Dan Benson, client engagements coordinator
danb@consultzen.com
949.617.1797
Marilee Benson, president, will be attending HIMSS22 and is scheduling time to meet with folks in the Interoperability Showcase. Please email DanB@consultzen.com to request a meeting time.
Zen Healthcare IT is an Interoperability Solutions company focused on removing healthcare data exchange barriers for our clients. We provide a secure, enterprise-class interoperability platform used by a wide range of HIE, provider group, hospital, and HIT vendor organizations. Our platform enables faster and more reliable data exchange. We have an excellent reputation in the interoperability space – schedule a meet up with Marilee to find out why.
Comments Off on HIStalk’s Guide to HIMSS22















 .
. 



























































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…