Top News

Private equity firm Patient Square Capital will acquire acute care telemedicine provider SOC Telemed for $3 per share, for a total of about $300 million.
SOC Telemed went public via a SPAC merger in November 2020 at $10 per share.
TLMD shares traded at a low of $0.58 in late January 2022.
HIStalk Announcements and Requests
A reader asked whether anyone visited the booth of First Line Software at HIMSS22, thinking that they operate in Russia. I received this response from Anatoly Postilnik, head of the company’s healthcare practice. First Line Software’s healthcare offerings include real-world evidence and data, health data management, AI/ML, systems development and integration, and clinical quality and safety systems. He clarifies:
First Line is a US consulting and custom software development company with a stellar reputation. We are headquartered in Cambridge, MA and have no affiliation with Russia or its government, which is currently waging a horrific war in Ukraine. We have offices on every continent and used to have a presence in Russia, but much like McDonald’s, Microsoft, and other respected US and International companies, we have aggressively pulled out of Russia and severed all ties with this country, relocating our employees to other countries and providing financial assistance to them to alleviate hardship.
Listening: Gilbert Neal, whose tracks I found randomly on Spotify and then played most of the day Monday. It is genre-bending excellence in singing and songwriting, every track highly listenable with smart, clear lyrics (not the usual love-and-lust prattling trying to pass as profound) and musicality that might at any given moment suggest Billy Joel, Steely Dan, Moxy Fruvous, or a 1970s prog rock band. I haven’t heard music this emotionally engaging for a long time. Website. The best phrase I’ve heard lately is Gilbert’s term for a group of his friends that would make a smashing band name– “a cabal of ne’er-do-wells.”
Webinars
April 6 (Wednesday) 1 ET. “19 Massive Best Practices We’ve Learned from 4 Million Telehealth Visits.” Sponsor: Mend. Presenter: Matt McBride, MBA, founder, president, and CEO, Mend. Virtual visits have graduated from a quickly implemented technical novelty to a key healthcare strategy. The challenge now is to define how telehealth can work seamlessly with in-person visits. This webinar will address patient satisfaction, reducing no-show rates to single digits, and using technology to make telehealth easy to use and accessible for all patients. The presenter will share best practices that have been gleaned from millions of telehealth visits and how they have been incorporated into a leading telemedicine and AI-powered patient engagement platform.
On demand: “Cybersecurity Threats Facing Healthcare Today.” Sponsor: Net Health. Presenters: Jason James, MS, CIO, Net Health; Monique Hart, MBA, CISO, Piedmont Healthcare; Jeffrey Rosenthal, , MBA CIO, Reliant Rehabilitation; David Jollow, MBA, CISO, Healogics. The panel of CIO and CISO leaders will discuss the cyberthreats that healthcare faces today. They will review security priorities for the increasingly complex healthcare IT environment that includes cloud-based applications, an increased number of endpoints that include connected devices and patient wearables, and patient portals.
Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock

Advocate Aurora Enterprises, the development and commercialization arm of the Illinois-based health system, acquires MobileHelp, which offers remote patient monitoring and personal emergency response systems.
Cloud-based analytics and value-based payments software vendor Clarify Health raises $150 million in a Series D funding round, bringing its total raised to $328 million. The company acquired analytics company Embedded Healthcare last month.
Nurse-1-1, a nurse chat software startup that works with digital health companies, raises $2.3 million in seed funding.
Home-based virtual care company HealtheMed, which focuses its services on Medicaid patients in Minnesota, raises $1.2 million in seed funding.
Sales
- Rady Children’s Hospital – San Diego will offer patients tech-enabled, home-based physical therapy services from Luna Care.
- Desert Oasis Healthcare (CA) will implement Lark Health’s digital cardiovascular coaching program.
- MemorialCare (CA) will integrate TytoCare’s AI-powered remote medical exam technologies with its telehealth services.
- HonorHealth goes live on Loyal’s Symptom Checker.
People


Protenus names Michael Baglio (Codametrix) CTO and Sonal Patel (DataBank) VP of professional services.

Konica Minolta Healthcare Americas promotes Fumihiko Hayashida to president and CEO.

Kelly Ostertag (Pivot Point Consulting) joins Continuum Health IT as VP of operations.

Kyruus hires Gail Airasian, MBA as GM of emerging markets.

Edward T. A. Fry, MD begins his term as president of the American College of Cardiology. He helped launch Ascension-owned data quality management company Navion Healthcare Solutions.


Orbita hires Sara Inman, MA (Press Ganey) as SVP of sales and Elizabeth Glaser (2bPrecise) as SVP of marketing.

Madaket Health promotes Martin Cody to VP of sales.

Tiffani Misencik (Intelerad Medical Systems) joins Greenway Health as chief revenue officer.

Craig Richardville, MBA (SCL Health) becomes SVP/CIO of Intermountain Healthcare as it completes its acquisition of SCL Health, expanding Intermountain to 33 hospitals, 385 clinics, and 59,000 employees with operations in seven states.
Announcements and Implementations
Amerimed Medical Solutions implements Bamboo Health’s Pings and Spotlights real-time care notification and performance metrics technologies.
A survey of community mental health center executives conducted by Owl and MCHA finds that top priorities are staff training, delivering treatments to the right person at the right time, expanding care access, delivering evidence-based guidelines, and measuring individual outcomes.
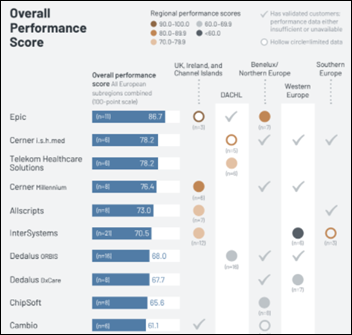
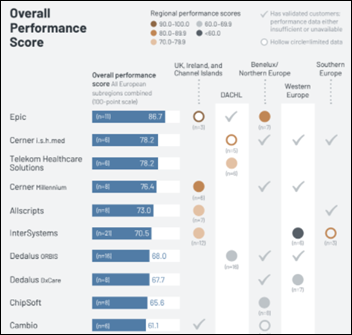
A new KLAS report on the EHR market in Europe finds that Dedalus and CompuGroup Medical expanded their market share via acquisitions, with Cerner selling its Selene and Medico products to CGM in shifting its focus to Millennium and I.S.H. Med. Software Medical and Epic had the largest organic growth, while Epic’s performance score topped the list. Low-scoring vendors are ChipSoft and Cambio (Benelux and Northern Europe) and InterSystems and Dedalus (Western Europe), although InterSystems TrakCare has high user satisfaction in Southern Europe, particularly Italy.
Government and Politics
ONC publishes the agenda for its 2022 Virtual Annual Meeting February 2-3 (education sessions) and April 13-14 (panel sessions, exhibit hall, and networking).
Other
In Germany, a 60-year-old man is arrested for forgery for receiving COVID-19 vaccine injections 90 times to obtain vaccination proof cards to sell. He was caught when he showed up at the same vaccination center on consecutive days.
Sponsor Updates
- The HIT Like a Girl Podcast features Ascom Americas VP of Sales & Business Development Shelly Bond.
- CareMesh publishes a new white paper, “5 Things Hospitals Can Do to Turn Epic into a Powerful Care Coordination Platform.”
- GHX will hold its 2022 Summit May 9-12 at the Diplomat Beach Resort in Hollywood, FL.
- Cerner releases a new podcast, “Breaking down bulk APIs.”
- CHIME and HIMSS pay tribute to health IT visionary David Garets.
- Clearwater publishes a new whitepaper, “The Guide to 405(d) Health Industry Cybersecurity Practices.”
- Diameter Health will present at the virtual NLP Summit April 6.
- Clearsense releases a new Tech Talk video, “The Rise of Clinician Data Scientists.”
- Sonifi Health releases digital whiteboard features that enhance the patient experience in hospital maternity units.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…