Kevin Coloton, MBA, MPT is founder and CEO of Curation Health of Annapolis, MD.

Tell me about yourself and the company.
We formed Curation Health in 2018. The primary objective is that the recognition that value-based care is extremely complex, and often a more difficult transition for organizations to take migrating from fee-for-service than many expect. It is particularly challenging for the providers at the front line of care delivery.
We are obsessed with solving for the experiences that our end users need. In our case, that’s the providers and the support they need to have sustainable success in value-based care. We recognize who they are and what they need, and we design tools and solutions to make it easier for providers to do the right thing when engaged in value-based care activities.
The end result of that is we have built a clinical decision support platform that facilitates provider workflow with the goal of elevating care delivery and receiving the appropriate clinical and financial outcomes for good work being performed.
I’ve had the great privilege of working in the healthcare industry for the past 25 years in various roles. Specifically, in patient care as a physical therapist, hospital administrator, management consultant, technology executive, and entrepreneur. I’m also fortunate that we have been able to assemble a team at Curation Health of industry veterans that have served organizations in health technology, consulting, and value-based care for a long time. They hail from organizations like Evolent, Optum, and The Advisory Board Company in Clinovations. In many cases, I’ve had the great privilege of working with a host of my colleagues for a very long time.
We’ve heard for years that value-based care is just around the corner, but most providers continue to make most of their revenue and profit from fee-for-service. How will that change?
The evolution of value-based care is slower than many expected, but is making progress. One of the most interesting, catalyzing events has been COVID and the pandemic. If patient volumes decrease in a purely fee-for-service environment, the clinical and financial implications of care for patients is pretty significantly impacted. Many organizations have recognized the need, despite the fact that they have a primary focus on fee-for-service. A balanced portfolio across fee-for-service and value-based care makes good sense to allow organizations to have sustained success.
We are seeing the march to value-based care taking a dramatic turn in the last nine months, where organizations are seeing appropriately that they need to start building the infrastructure and participating in value-based care. In some cases in their regional and local markets, the health plan and provider collaborations have greatly encouraged migration to more value-based care. It’s an important effort for almost all organizations, regardless of their payer mix, to have begun investing in value-based care infrastructure, capabilities, and knowledge.
How do the clinical decision needs of providers change as they start to see patients under a value-based care arrangement?
When you reflect on what’s different between fee-for-service and value-based care, most organizations today — unless they are purpose-built for value-based care — rely on a fee-for-service infrastructure. Their operations, their scheduling process, their patient contact. Even the clinical operations themselves of registration, check in, rooming the patient, seeing the patient, and allocating time for visits are all very different if you’re in a fee-for-service environment versus value-based care.
The provider challenge is that they are attempting to have more intensive, longer value-based care interactions with patients where they are reviewing the complete chart and trying to prioritize, what is the clinical focus for our time today? They are balancing that with fee-for-service interactions, which are typically 10 minutes or less and focused on the reason for the visit. Why is the patient here today? Certainly they take care of other healthcare priorities as well, but it’s a very different mindset and operational approach.
Our goal is to simplify, to take some of that cognitive load away from identifying which patient is in front of me today. Which plan are they associated with? If they are in a value-based care arrangement, what should be my clinical priorities to address today for this patient, oriented to the highest clinical impact? If I only have time to do one thing today, what’s the most important thing for me to do? Or, what are the top two priorities I should focus on to achieve with this patient today?
The other big transitional difference is that value-based care is managing thousands of patients over a calendar year. Fee-for-service is typically prioritized and focused on, what are the priorities for the 30 patients I have scheduled tomorrow or the patients I have scheduled across the next few days? It’s a pitching and catching delta, where value-based care is a strategic approach across the calendar year and fee-for-service has a tendency to be more reactive, where patients are coming to the clinic, in the home, or in a telemedicine visit with a particular urgent or emergent need or acute need. Those are very different operational approaches. We aim to simplify that.
The technology requirements of that “feet in two boats” situation, where a given patient may be covered by fee-for-service or a value-based care arrangement, must be complex.
Massively complex. The attribution of patients alone is a massively complex undertaking. Which patients in my care are mapped to which value-based care program? We have some clients that have four, five, or six different value-based care contracts with different health plans. That complexity is massive.
Our goal is to greatly simplify that by having the provider focus on one simple workflow, and have that workflow be agnostic to whatever plan they’re mapped to. We focus our technology to simplify, to say that “this patient has these priorities that would benefit from being addressed in this interaction for the provider” instead of the provider trying to figure out which health plan it is, and of that plan, which subset a VBC contract is aligned with that. What have I already taken care of this calendar year? We seek to greatly simplify it by producing insights that are prioritized by clinical impact and greatly simplified into the handful of items that the provider can take care of to maximize the health of the patient.
In some cases, they are not even aware of which value-based care contract that patient is mapped to, because they don’t need to be. Their focus is on rendering awesome clinical care for the patient. Having one simple workflow enables them to focus on what matters, which is, this patient needs my help in these areas.
The healthcare technology industry has a tendency to focus on what we describe as data maximalism, which is this mindset that bigger is better. It’s really the identification of massive amounts of data that holds limitless potential value, and it’s candidly the easiest and most exciting approach to take. You can use incredibly modern and precise technologies to harvest a tremendous amount of data at a patient level or across your whole community of patients you’re serving.
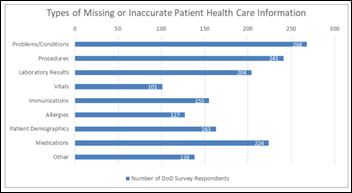
When we launched Curation Health in 2018, we learned the hard lesson of having a data maximalism approach. The problem is that when you’re analyzing a massive amount of data — and in our case, we also compile this dataset with human review to find more and more items of opportunity — the results we found were counterintuitive. The more accurate and voluminous the data that we found and sent to providers, the less they acted on it.
We quickly learned that the value is not on the potential of this information and what it could do to transform provider success. The only thing that matters is what information they are going to use when managing a patient’s health. Therefore, we came to this realization that value-based care, healthcare technology analytics and reporting, and clinical decision support are not really technology problems to solve. It needs to be a clinical workflow problem to solve. How do you make it easier for the provider to do the right thing?
We evolved this concept of data minimalism, which in our mind is the minimum dataset required for a provider to use to enhance the health of their patient. Instead of bigger is better, which is the data maximalism approach, data minimalism is that less is more. Once we prioritized and contextualized the information that we were sending to physicians, we saw adoption and use skyrocket. It was a really powerful lesson for us. It revolutionized the way we design our technology platform, how we build our user interface, and how we choose the information that we are serving. It made it simpler for providers to act. We learned more and more of the power of simplicity and the direct correlation with provider adoption and use.
How much detail and complexity is contained in a provider’s value-based care contract that is translated into plan-specific clinical decision support?
The contracts themselves are incredibly complex. They are very different from agreement to agreement. Some prioritize risk adjustment performance HCCs and related measures, RAF particularly. Some prioritize quality, HEDIS, and Stars. It is very dependent on the region, the health plan, and the provider partnership. Because of that, we spend a lot of time with our clients helping demystify the agreement that they are participating in. What would be the analysis of the return on investment clinically and financially for the organization? What are the KPIs that the provider group needs to focus on to achieve the results they’re hoping to achieve? If they have limited time, where would they emphasize their focus and dedicate their attention to serving particular metrics, measures, or activities that help everybody win in this equation?
The premise with this equation is that if we can prospectively manage the patient’s health and outcomes, then we can improve their health, and everyone wins in this model. The health plan, the provider organization, and ultimately the patient. The goal is to also understand that this particular value-based care contract prioritizes certain investments of energy and time and making sure that everybody is aware of those and keeping appropriate attention on those items.
How does the pre-visit review differ under a value-based care arrangement?
I had the great privilege of running ambulatory clinics for a period of time in a predominantly fee-for-service environment, so I have a good sense of how that works. The value-based care pre-visit activities are dedicated to figuring out ahead of a clinical interaction, what are the top clinical priorities that this patient is challenged by? Then, focusing the provider attention on those priorities.
In the traditional model, physicians would quickly scan the chart and go into the room, if it’s a clinic setting, and ask the patient something along the lines of, “What brings you to see me today?” to make sure that they are aligning what they see as the priorities with what the patient priorities are. That’s good practice.
In a value-based care world, it’s a little more complex, because you have to understand what you’ve already done that calendar year. What items remain to be managed? Also, what are the priorities that you haven’t yet covered with the patient that would greatly improve their health and wellness?
That concept of pre-visit is leveraging good technology to discern clinical opportunities from the thousands and thousands of lab values, radiology reports, HIE data sets, EMR data, and claims data and narrow it down to a specific set of high priority items that the patient would benefit from having managed. In some cases, the pre-visit review also involves a human reviewing the output of the technology or the reports to further refine the data that gets to the physician. Ultimately, the goal is that when the physician enters the room with the patient, they are well aware of the clinical priorities that need to be addressed, but they also have the context as to why these are priorities.
One of the big challenges of working in a fee-for-service and a value-based care world is that providers are challenged by capacity, time, and resources in most cases. They have limited time with the patient. They may not have a lot of technology tools or humans to participate in that pre-visit analysis. So when they review the clinical opportunity while sitting in front of the patient, they often don’t have enough time to validate them, to go through the EMR and understand when this lab value is drawn and what this comorbidity and this medication might lead to. The goal with pre-visit is to take all of that clinical administrative research and have most of it conducted before the patient is being seen by the provide so that the provider is able to focus their attention on validation and action rather than just pure research.
Do patients know that they are being covered by a value-based care arrangement? Do they need to be educated about their role in it?
It varies. In some cases, patients are well aware of the program that they are participating in. They are able to make determinations of which network they want to participate in or who the provider group they want to have administering their care. In other cases, it’s more of an administrative function that happens in the background, and patients may or may not be aware of it or have much information or insight into what it means and the potential delta of how the physician may be managing their clinical interaction.
I think Medicare Advantage has become the largest area of focus in the value-based care realm. A lot of patients are becoming more understanding of why it’s important to have more of a prospective care approach than a retrospective care approach or a fee-for-service, real-time engagement.
It definitely varies by region, by plan, and by other elements. But I have seen many cases where patients are very aware of it. I think you’re right, though, that the onus is on the provider, the practice, the organization, or the health plan to educate the patient as to the change in the model of care being delivered. From the feedback we hear, patients have appreciated the value-based care approach, because it feels like their care is being holistically managed and sometimes a bit ahead of time. We are biased, but we believe it’s a better model of care delivery where you’re trying to anticipate future need by focusing on current challenges and engaging the patient in that journey more directly.
What factors do you see impacting the company’s strategy in the next three or four years?
Several elements are going to be impacting our strategy. We highlighted one of them at the beginning of our conversation, which is how quickly organizations are adopting value-based care. Some organizations are in the early phase of their journey, while others have been doing this for some time. That progress directly impacts our ability to serve and elevate performance for those organizations. The ever-changing nature of the value-based care design model and contracts definitely are impacting how we do what we do. Every year we are constantly scanning regulatory changes. Compliance is a huge priority for us. Our clients are relying on us to greatly focus on that. We need to be very current, and the only constant in the value-based care structure to date has been change.
The other element is care model delivery has been greatly changing. We’re having a real increase of organizations focused on in-home primary care, in-home specialty care, and virtual care. How all of those align with value-based care models has been interesting and fun for us to design and partner with. I think that will keep us busy for some time.
Comments Off on HIStalk Interviews Kevin Coloton, CEO, Curation Health


































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…