Top News

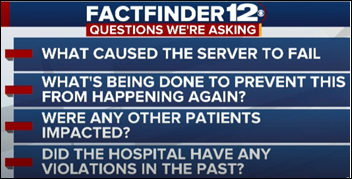
LabCorp shuts down its entire computer network when it detects that a hacker has penetrated its systems and is trying to access patient records.
The company says via an SEC filing that test processing and customer access was limited over the weekend. It will take several days to bring all systems back online, the company says, causing delays in results reporting.
LabCorp hasn’t yet said whether PHI was compromised.
The company does not use Twitter or Facebook, but its LinkedIn profile and its website don’t mention the outage.
Reader Comments

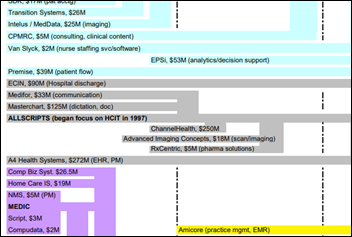
From Another Allscripts Casualty: “Re: Friday the 13th Allscripts layoff. Our VP used a lot of corporate jargon words like ‘synergy’ and ‘socialize the discussion’ to describe the streamlining process in which basically each manager had to remove one employee slot, even those with teams of just a handful of people. Team managers were notified only 30 minutes before the heads rolled. The cuts were not performance based, so producer worker bees were let go instead of middle layer fat. The McKesson EIS acquisition brought in a lot of overlapping people and I expect another round late this year or early next as more people are trained to be cross-functional. Allscripts is like the mythical Hydra – every time they lop off a head, another acquisition causes 10 more to pop up, and management is never lopping the right heads. I think some of the people at the top have a good idea of where they want to take the company, but the inertia of herding cats keeps them in the same rut.” Unverified. I’m not as confident that the company has a solid, rational strategy other than making undisciplined acquisitions that sometimes work out great (Netsmart, DbMotion) and sometimes just fizzle out quietly. That’s been the strategy all along, but other than a burst of investor enthusiasm that sent shares on a tear in 2000 (peaking then at more than six times today’s share price), it’s been a market-lagging stock that made headlines for mostly the wrong kind of reasons as it also came late to the post-MU EHR consolidation party by finally announcing that it would develop a new product, which is new territory for a company known for buying instead of building. Even with all that acquisition activity, Allscripts has a market cap of $2.2 billion, around 1/10 that of Cerner and one-third of Athenahealth’s market value. It has made some good deals, though – it paid just $185 million to buy the health IT business of a desperate and perpetually HIT-clueless McKesson, then sold off just the content management part to Hyland for up to $235 million.
From Fact Checquer: “Re: Allscripts. You mentioned the new EHR product Avenel. I find no mention of it on the company’s site.” It’s not listed on the physician EHR page with TouchWorks or Professional, but I found by Googling that it has its own site that says “machine learning” a lot and offers only a “contact us for more information” form.
From Bjorn To Be Wild: “Re: HIStalk theme music. I don’t know when you added it, but I love it. It improved an already wonderful daily morning reading and coffee experience.” I put up the prog rock “HIStalk Theme” a few weeks ago. That musical style isn’t to everyone’s taste, so I’m considering commissioning a light jazz sort of tune for a more mellow experience. It’s surprisingly inexpensive (in the $100 range) to have custom music created to spec.
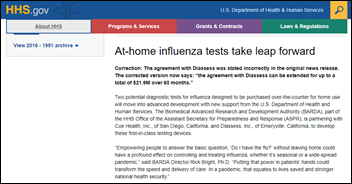
From RN Data Maven: “Re: National Guidelines clearinghouse shutdown. A tragic loss of a resource for practitioners to access evidence-based clinical practice guidelines. Fear of evidence-based scientific research or short-sighted funding decisions?” AHRQ says it can’t come up with the $1.2 million to keep the site running and thus took it down this week, but the non-profit ECRI – who managed the site for AHRQ — will bring it back in the fall with enhancements as a fee-based service. Some speculate that the site was doomed once then-Congressman Tom Price, MD (who later became HHS Secretary for a few months) demanded that AHRQ remove a study that was critical of a drug sold by one of his campaign donors.
HIStalk Announcements and Requests
Lorre has a backlog of inquiries for my annual “summer doldrums special” on new sponsorships and webinars, but she would still be happy to chat.
I was thinking today that Karl Marx’s “opiate of the masses” is no longer religion – now it’s actually opiates.
Webinars
July 26 (Thursday) 1:00 ET. “The Patient’s Power in Improving Health and Care.” Sponsor: Health Catalyst. Presenter: Maureen Bisognano, president emerita and senior fellow, Institute for Healthcare Improvement. Patients, even those with chronic diseases, only spend a few hours each year with a doctor or a nurse, while they spend thousands of hours making personal choices around eating, exercise, and other activities that impact their health. How can we get patients to be more engaged in their care, and help physicians, nurses, and healthcare providers transition from a paradigm of “what’s the matter” to “what matters to you?” This webinar will present stories of patients and healthcare organizations that are partnering together with tools, processes, data, and systems of accountability to move from dis-ease to health-ease.
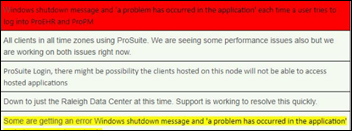
July 31 (Tuesday) 12:30 ET. “How to Proactively Troubleshoot End User Experience Issues in Healthcare IT.” Sponsor: Goliath Technologies. Presenter: Goliath Technologies engineering staff. An early warning system for EHR access problems helps prevent downtime and user access problems before they impacts patients and collects objective technical evidence of the issue’s root cause. This webinar will describe how hospitals protect their investment in Allscripts, Cerner, Epic, and Meditech EHRs by anticipating, troubleshooting, and preventing end user experience issues and collecting the technical data needed to collaborate with their vendors on a solution.
Previous webinars are on our YouTube channel. Contact Lorre for information.
Acquisitions, Funding, Business, and Stock

UnitedHealth Group reports Q2 results: revenue up 12 percent, EPS $2.98 vs. $2.32. The company’s UnitedHealthcare insurance business took in $46 billion as membership increased to 49 million people. Its Optum segment, which provides pharmacy benefits management and technology services, booked $1.8 billion in profit on $25 billion in revenue for the quarter.

Nashville-based post-acute care CRM software vendor PlayMaker CRM acquires post-acute market intelligence and analytics vendor ViaDirect Solutions and renames itself PlayMaker Health.
Sales
- CoxHealth (MS) chooses Kyruus to provide a digital provider directory and patient-provider matching technology for its website and call center.
- Southwest Mississippi Regional Medical Center selects Phoenix Health Systems for outsourced IT management and support.
- Australia’s Canberra Hospital and University of Canberra Hospital will implement Alcidion’s Electric Patient Journey Board to reduce length of stay and improve patient flow from the ED.
Announcements and Implementations
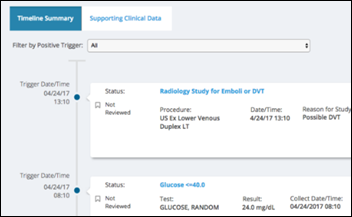
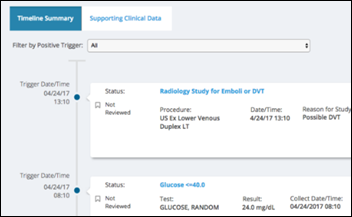
Health Catalyst launches a patient safety surveillance system and applies to become an AHRQ-certified Patient Safety Organization (PSO) that can offer clients a litigation-free environment for data analysis. The trigger-based system cost $50 million to develop. The company says EHRs offer limited surveillance capabilities and, unlike a PSO framework, are legally discoverable.
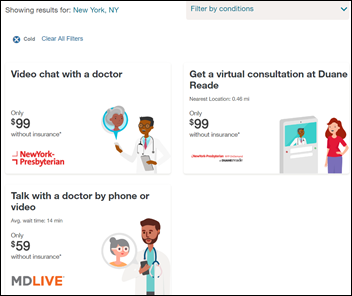
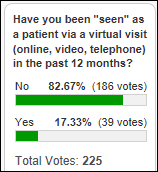
CompuGroup Medical launches its ELVI telehealth product.
Behavioral Health Network of Massachusetts goes live on ZeOmega’s Jiva population health management.
Government and Politics
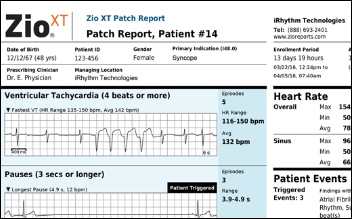
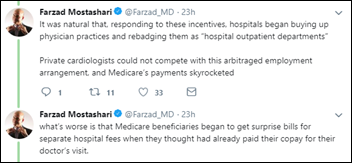
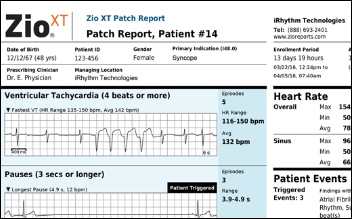
NIH Director Francis Collins, MD, PhD pitches IRhythm’s Zio arrhythmia monitoring patch for detecting unknown atrial fibrillation, although noting that while the results may get patients to visit their doctor and begin anticoagulant therapy, its long-term benefit in reducing strokes, ER visits, and hospitalizations remain unproven. Collins concludes that the clinical trial was interesting because high-risk patients were recruited by email, had the patches mailed to them, then mailed them back at the end without having met a researcher face to face. Less exciting is the fact that we have yet another high-powered diagnostic tool to detect diseases that we as a country can’t afford to treat because we refuse to control healthcare costs — those newly ordered anticoagulants cost $15 per tablet, meaning someone will be paying $5,000 per year for the rest of each new patient’s life, although maybe that’s cheaper than treating the subset of them that would have otherwise had strokes.
FCC will propose in its August meeting to fund a $100 million “Connected Care Pilot Program” that would promote using telehealth among low-income families and veterans by providing affordable broadband service. Up to 20 providers that serve low-income populations would receive up to $5 million in funding in partnership with a broadband services provider.
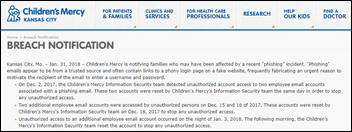
Privacy and Security
In Canada, home care provider CarePartners is hit by ransomware, with the hackers contacting CBC News with samples of the patient information they have stolen (the samples alone involve 80,000 patients).The cyberintruders, who say they found unpatched software that allowed them to penetrate the systems, are demanding unstated “compensation in exchange for telling them how to fix their security issues and for us to not leak data online.”
Change Healthcare introduces a kill switch for its HealthQX value-based care analytics suite that allows customers to instantly revoke access to their data as long as two of its authorized operators issue the command from separate locations as part of a “bring your own key” capability.
Other
A Quest Diagnostics survey finds that healthcare has made little progress toward value-based care since last year. More than half of health plan executives think physicians don’t have the tools they need to succeed under VBC arrangements, while 61 percent of doctors say their EHR doesn’t contain all the information they need to deliver patient care.
In Australia, 20,000 people opt out of sharing data with its My Health Record online system on the first day of the three-month opt-out period.
Western State Hospital (VA, rebranded from the more memorable Western State Lunatic Asylum) realizes that it hasn’t followed state laws allowing it to destroy the records of patients 10 years after their last date of service, forcing a three-year records review in which a single HIM employee examined 6,000 reels of microfilm dating back to the 1800s. And you thought your job was dull.
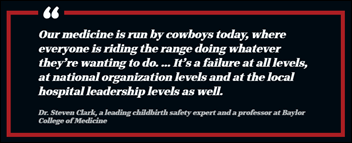
A New York Times report notes that rural hospitals are not only closing at alarming rates, they are eliminating OB services to the point that fewer than half of US rural counties still have hospitals that deliver babies. It notes that loss of OB services means that fewer women receive prenatal care due to the time and cost of traveling further, more of them deliver prematurely, infant mortality increases, and EDs deliver babies the best they can.

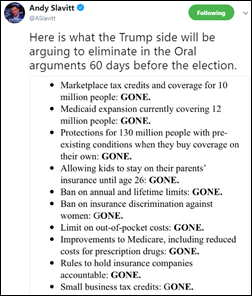
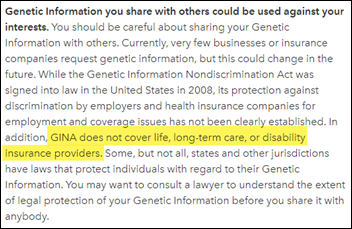
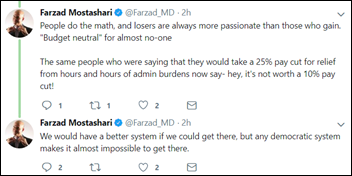
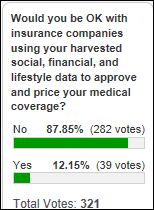
This is important as the White House dismantles ACA protections that prohibit insurers (including those who sell through employers) from denying coverage for pre-existing conditions or charging sicker people higher premiums. A ProPublica report finds that insurers are buying the lifestyle information of hundreds of millions of Americans from data brokers that includes race, educational level, TV habits, clothing size, net worth, credit, and social media activity, all of which are run through algorithms that predict how much that person’s healthcare will cost. The article notes that while the information is ostensibly used to manage population health, it could also be applied to premium pricing formulas. Experts say that while insurers can’t blatantly discriminate (at least for now), they have cherry-picked the healthiest people by choosing their geographic coverage based on population data, or as one data salesperson said, “God forbid you live on the wrong street these days.” An excerpt:
[LexisNexis] said it uses 442 non-medical personal attributes to predict a person’s medical costs. Its cache includes more than 78 billion records from more than 10,000 public and proprietary sources, including people’s cell phone numbers, criminal records, bankruptcies, property records, neighborhood safety, and more. The information is used to predict patients’ health risks and costs in eight areas, including how often they are likely to visit emergency rooms, their total cost, their pharmacy costs, their motivation to stay healthy, and their stress levels. People who downsize their homes tend to have higher healthcare costs, the company says. As do those whose parents didn’t finish high school. Patients who own more valuable homes are less likely to land back in the hospital within 30 days of their discharge. The company says it has validated its scores against insurance claims and clinical data. But it won’t share its methods and hasn’t published the work in peer-reviewed journals.
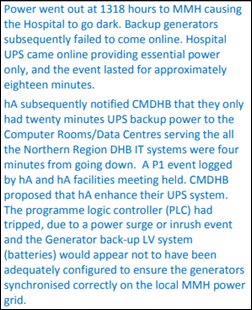
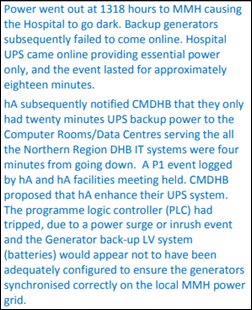
In New Zealand, an internal health board report finds that hospital generators failed to kick on after a power line was cut, with battery back-ups having just four minutes of power left when the power came back on. My experience with generators is not reassuring – even with regular testing and fuel monitoring, the switchover always seem to fail. What’s your experience?
In England, a nurse assistant is charged with fraud after submitting timesheets indicating that she had worked 242 shifts in 20 months instead of her actual 10, for which she was overpaid $66,000. She claimed that she thought she was entering the times she was available for work instead of logging her actual time. She had asked her manager to help her, which might have provided yet another clue to the manager that her entries were incorrect. The judge noted that the hospital makes such fraud easy.
Bizarre: a hospitalized prisoner who eats metal objects such as catheter clamp, thumbtacks, and screws racks up $1 million in medical bills, then is admitted under 24-hour watch to Loyola Medical Center in a stay that has added $500,000 to his tab as taxpayer-funded hospitals try to keep him from being admitted to their facilities and the hospital presses the prison for payment. The prisoner is a 6-foot, seven-inch former basketball player who has previously threatened hospital employees. The sheriff bluntly but accurately explains:
We have a guy right now that has cost us — has cost all the people in this room — close to a million dollars in health bills because he constantly eats the jail. Across the country, the easy thing to do was cut mental health services, and they’ve done it. So people don’t get better. They don’t get treatment. They go to jails and prisons and emergency rooms.
Welcome to a country run by lawyers. In Las Vegas, Mandalay Bay Hotel’s corporate parent MGM Resorts International sues 1,000 concert-goers injured in the Route 91 Harvest festival shooting last year, hoping to force a decision that it can’t be held liable because it hired a security firm that was certified by the Department of Homeland Security for protecting against mass injury. A lawyer representing some of the victims says the company – which also owns the concert venue — is “judge shopping” in trying to push any case into federal instead of state court.
Sponsor Updates
- PatientKeeper publishes an e-book titled “Attending to Physicians: Why Healthcare Must Focus on Improving Physician Experience” and a video titled “PatientKeeper Charge Rescue Service.”
- Buffalo Business First profiles Hamish Stewart-Smith, CTG’s managing director of sales for its North American healthcare business unit.
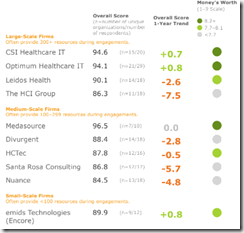
- Huntzinger Management Consulting Group earns high rankings in the KLAS HIT Assessment & Strategic Planning 2018 report.
- FDB releases a new video to help people understand how its Opioid Risk Management Module supports safer opioid risk management and prescribing.
- Divurgent publishes its “Windows 10 Upgrade Benchmark Report.”
- Optimum Healthcare IT publishes a white paper titled “Change How You Approach Change in Healthcare.”
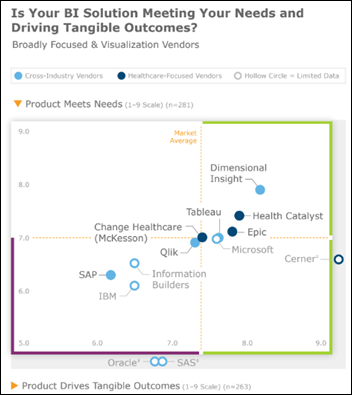
- Dimensional Insight VP George Dealy earns CHIME’s CFCHE credential.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates. Send news or rumors.
Contact us.




























































































































![image[30] image[30]](https://histalk2.com/wp-content/uploads/2018/07/image30.png)





















Thank you for the mention, Dr. Jayne — we appreciate the callout, the kind words and learning more about the…