EPtalk by Dr. Jayne 3/10/22
Healthcare workers are still at risk for COVID infections. Even though vaccines have been proven to reduce hospitalization and death, there’s still risk of infection and the potential for subsequent disability. A growing body of evidence shows long-term cardiovascular and neurological complications from even mild cases of the disease, and an estimate of over 1.5 million adults in the US who are seeking permanent disability determination following infection.
During my recent visit to the hospital as a patient, I don’t recall seeing hospital employees wearing anything other than surgical masks. Some patients were wearing KN95 masks, but it made me wonder whether wearing surgical masks was an employee choice or whether there is still a supply shortage for respirators or other types of masks.
With that in mind, I wasn’t surprised to learn that OSHA plans to increase healthcare facility inspections to assess preparedness for the next COVID-19 variant that might emerge. The initial focus will be on facilities that were previously cited or had complaints filed against them. OSHA is supposed to be finalizing an infectious disease standard for worker protection, and for the healthcare workers who have been permanently impacted by the pandemic, it can’t come soon enough.
I’m a history buff, so was quite excited to see the announcement that Ernest Shackleton’s ship Endurance has been located nearly two miles below the surface of Antarctica’s Weddell Sea. It’s remarkably well preserved due to the extremely cold waters and the lack of wood-damaging organisms. The technology needed to locate the wreck is pretty remarkable, but so is the determination of those who worked in difficult conditions to make it happen. The ship’s resting place is protected as an historic monument under the 1959 Antarctic Treaty, so nothing was disturbed in the exploration of the wreckage. Kudos to the anonymous donor who financed the $10 million mission.
Healthcare news and announcements are at a minimum this week, other than Epic’s announcement regarding Garden Plot. My inbox is full of poorly worded but jargon-rich emails practically begging me to visit various HIMSS booths. Having more than three buzzwords in the first sentence dramatically lowers my chances of actually showing up.
I’ve also received some tips on pretty cool things that will be revealed next week but am sworn to secrecy, so you’ll have to follow along for the news as well as our on-the-ground reporting. Mr. H is doing the short version of the conference, but I’ll be there Sunday through Thursday, so we’re leaving a gap in reporting Friday’s keynotes. Both of them looked interesting, but I know from experience that by Friday I would be too exhausted to care and prefer to sleep in my own bed rather than dropping another $200 on a hotel room.
I’m experiencing a last-minute flurry of work prior to the conference, however. It seems my clients must have some kind of fear that I’m going to run away to Florida never to return, because a couple of them have decided they want to accelerate projects that haven’t been on their priority lists for weeks. I was able to accommodate some because they were close to completion and just waiting on a few details from the client, but others are just going to have to wait. I may address some of them on the plane, depending on my mood and the surroundings, but no promises were made.
The farther I get in my career, the more I’m likely to engage the rule that “no is a complete sentence.” I don’t mind going the extra mile when someone has an unexpected need or something out of the ordinary happens, but I don’t make a habit of running around crazy when it could have been avoided.
I’m also doing some last-minute shoe shopping, having decided that in 2022 footwear comfort is much more important than style. HIMSS was already becoming more casual the last time I attended in person, and based on the numbers of us who are used to working at home in hiking pants and pullovers, I’m sure the casual ethos will extend to the exhibit hall. I’ll still be looking for good shoe photos, though, so if your feet are young and you’re feeling sassy, I’ll keep an eye out for you.
As far as packing, it’s also a good 50 degrees warmer in Orlando than it is for me at home. Although I’m looking forward to breaking out the spring and summer clothes, I hope it’s not completely sweat-inducing next week in Orlando since I’ll be doing a lot of walking from my hotel out in the cheaper part of town. Maybe some day I’ll hit the big time and be able to stay right across the street, but that wasn’t in this year’s budget.
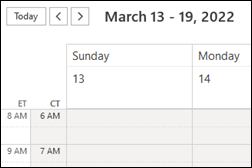
The biggest challenge of the week has been an issue with my Outlook calendar, which Microsoft assures me will be fixed once the time change actually occurs on Sunday. This week looks normal, as does the week following HIMSS, But starting Sunday, the system has gone wonky when converting between good old Chicago time and the East Coast. Fortunately, my administrative assistant is reconfirming all my meetings and creating a backup document in case things don’t go as well as we hope on Sunday morning.
I have a new friend joining me on the party scene this year and am looking forward to connecting with old friends as well. It’s been a long depressing winter for me, so if you see the blond-haired person in sunglasses sprawled out on the lawn in front of the convention center, it just might be me. I have to enjoy it while I can, since HIMSS23 in Chicago won’t likely lend itself to lounging on the grass.
Are you packed and ready for HIMSS, or still knee-deep in ViVE? Or are you just glad to be staying home in your yoga pants and quarter-zip while the rest of us head to the boat show? Leave a comment or email me.

Email Dr. Jayne.







Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…