EPtalk by Dr. Jayne 4/15/21
It’s a good day to be a clinical informaticist when you can put your knowledge to work and try to help people understand complex clinical topics. The recent pause in administration of the Johnson & Johnson COVID-19 vaccine made today one of those days.
I put on my statistics hat and was able to deliver a quick educational webinar for one of my clients, helping the team understand the reason for the pause and what is being done to better understand the situation. The reported blood clots are cerebral venous sinus thromboses and present with low platelets in addition to the clot. They have occurred in women aged 18 to 48 within two weeks of vaccination, so we should be able to look at administration data to watch those patients more closely. Should our clinicians suspect one of these potentially vaccine-related clots, the treatment is significantly different than that for a “regular” blood clot, so we’re starting to talk about clinical decision support tools to make sure physicians check vaccine status before giving a potentially harmful drug. For my family members who don’t understand what I do when I’m not “being a regular doctor,” this is it.
When I sat for my clinical informatics board exam in 2014, a significant part of the potential content was in the realm of public health informatics. If we’ve learned nothing else during the COVID-19 pandemic, it’s that shortchanging funding for public health hasn’t done anyone much good. The Centers for Disease Control and Prevention released annual sexually transmitted disease surveillance data for 2019, and for the sixth straight year, diseases are at an all-time high. More than 2.5 million cases of chlamydia, gonorrhea, and syphilis were reported. Although the CDC data is older, we definitely saw a boom in STDs in 2020 especially during the initial lockdown phases of the pandemic.
It’s clear that “six feet apart” means different things to different people, but it’s always good to see the visits, because it means people are being tested and treated. People underestimate the impact of STDs and their unintended consequences. While syphilis is up 74% from 2015, congenital syphilis (passed from infected mothers to their babies) is up 279%. Understanding the power of data is a big part of what I do and I’m glad to be in clinical informatics.
Since the recent requirement to make hospital pricing data public, there have been allegations that organizations are using code to block pricing data from appearing in web searches. The House Energy and Commerce committee sent a letter earlier this week to the Department of Health and Human Services, asking for strict enforcement of the price transparency rules. The letter includes a citation from a recent analysis that shows more than 3,000 sites using search-blocking code. Given competing priorities, it remains to be seen how quickly any enforcement efforts will unfold. I’ve seen news stories where physicians who violate federal controlled substance rules are hauled out of their offices by the DEA, so seeing hospital administrators being escorted out in handcuffs would make my day.
With the recent regulations requiring release of visit notes to patients, a corresponding article in the Journal of the American Medical Informatics Association was timely. It focused on patient and family experiences after identifying what they perceive as serious errors in visit notes. The data was from a 2016 survey of patients at two academic medical centers, and although it wasn’t recent, many of the principles likely still apply today. The authors found that among more than 8,000 patients who read at least one note, 17% identified at least one mistake. More than 40% of those patients felt the mistake was serious, and 56% contacted their providers. Barriers to reporting perceived mistakes included not knowing how to do so and concerns about being thought of as a troublemaker. Study participants also had the opportunity to provide suggestions and recommendations for how medical centers can partner with patients and families.
Some of the suggestions included making sure that the reporting process is clear; reassuring patients that there will be no retribution; making reporting templates available; normalizing the idea of patient feedback; and otherwise making feedback easier for patients. Other suggestions included creating some kind of sign-off that would show that a patient had read and approved a note, or the ability for patients to easily add an addendum to a note. Given the resistance of physicians and healthcare organizations to releasing notes in the first place, I think it will be some time before there is support for the latter suggestions. Organizations are much more likely to make the reporting process clear or create reporting templates before they will let patients write in their own charts.
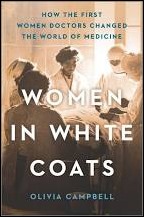
I just finished reading a book about women doing unspeakable and unladylike things. “Women in White Coats” by Olivia Campbell chronicles the lives of some of the first women physicians in the US and the UK during the 1800s. The first female medical students had to endure all kinds of harassment, including being pelted with mud and physically blocked from attending class by their male classmates. Even after earning degrees and entering practice, they encountered landlords who refused to rent office space to them because it was felt their actions were unseemly. Despite the energy spent simply enduring the experience, early women physicians brought new perspectives to medicine, including a focus on public health, hygiene, and educating mothers on how to keep their families healthy. I enjoyed the read and it definitely added perspective to my career, especially since my medical school class was the first in my institution to have more women students than men and my residency class was all women.

Rideshare service Uber has teamed up with PayPal, Walgreens, and the Local Initiatives Support Group to create the Vaccine Access Fund. The goal is providing free transportation for patients who don’t have the ability to get to a vaccine site. Funds will be directed to local nonprofits who are working to ensure vaccine access.
I have some friends working towards this locally and there are still significant barriers for some patients, including long shifts at work and lack of paid time off. There are also plenty of people juggling multiple jobs and that certainly doesn’t make it any easier. I’ve made jokes about this, but it’s starting to sound more like something that could actually work: a hybrid food truck / vaccine delivery platform. It would be an ideal way to raise interest and could be routed to a different workplace every day. Throw out some lawn chairs and a couple of pop-up shelters and your clients can enjoy sliders while completing their 15-minute observation period. Who’s with me?

Email Dr. Jayne.


Sounds reasonable, until you look at the Silicon Valley experience. Silicon Valley grew like a weed precisely because employees could…