Top News

Walgreens Boots Alliance is struggling with the performance of primary care chain VillageMD, in which it is the majority shareholder.
Walgreens has closed 27 of the 60 underperforming locations that it previously announced and will focus on marketing the practices in hopes of boosting patient panels that are lower than expected.
Walgreens said in last week’s earnings call that it will take advantage of its strong neighborhood presence “to help payers, providers, and pharma achieve their goals.” The company is freeing up pharmacist time to allow more meaningful patient interaction via health screenings, immunizations, diagnostic testing, and treatment and has contracted with 25 drug companies to recruit clinical trials participants.
The CEO concludes, “We are going to be a major community-based, neighborhood point of engagement for patients with human beings touching human beings, which I believe in the long term is how how healthcare in this country is going to evolve.”
Reader Comments
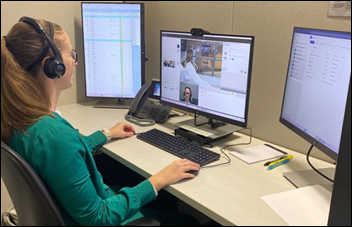
From Conferencius: “Re: conferences. Is your skipping the HIMSS conference for the first time in years an early indicator of a trend? I find myself being less interested in attending conferences in general.” I’m not sure a trend exists, although the newer, glitzier conferences may spread the attendance and exhibitor wealth around. Attending conferences without employer expectations can be fun, but I question the ROI for the patients who foot the bill for days of socializing, expensive meals, and splashy entertainment under the guise of “networking” that at least in my experience, never paid off for my employer. However, I learned early as a health system IT executive to grudgingly approve the cost of sending high-value employees to conferences without expectation of ROI beyond stroking their egos and leaving them vaguely “inspired.”It’s funny that as an industry, we assure patients that we can deliver life-affecting health services via telehealth and remote patient monitoring, but we can’t do our paper-pushing jobs without expensively traveling with the herd to a publicly traded company’s equivalent of a destination wedding. The COVID-era failure of virtual conferences proves that it was never about education. Your question inspired a poll (below).
From KC Masterpiece: “Re: David Feinberg. Finally found another company who needs a selfie-taker.” Feinberg isn’t leaving Oracle Health as chairman, at least not at the moment. He has taken an additional paying job as an advisor to a VC firm. People still ponder how it came to be that he took over as Cerner president and CEO (but not board chair) on October 1, 2021 and the board agreed to sell the company to Oracle 80 days later, netting him dozens of millions for having done nothing except choose office furniture. We don’t know if the acquisition was sealed by his hiring and if he knew in advance that it would swell his pockets mightily. I’m not clear on what his day job as “chairman” of a company’s single operating division even means since as far as I know, Oracle Health doesn’t have its own board for Feinberg to chair and I’m not sure he even has direct reports.
From Rascule: “Re: HIMSS Accelerate. The HIMSS VP who ran it is now the head of marketing at HLTH.” Verified from LinkedIn. HIMSS launched the Accelerate online discussion platform in mid-2021, the seemingly ideal time to provide an alternative for COVID-halted conferences, but it never caught on. HIMSS also created the similarly timed and named HIMSS Accelerate Health, whose purpose wasn’t clear but seemed to involve conference tracks and a podcast, but that seems defunct as former links go to 404 pages or to HIMSS TV. I sure would like to see a current HIMSS 990 form that tax-exempts are required to post publicly to get a better idea of the business structure, but they haven’t filed one since FY2020.
From Pivoteer: “Re: consulting. You should do a poll on how many readers lost or quit jobs and tried to morph themselves into a consulting firm until finding a job.” I’ll do that poll next time. I try not to be cynical about folks whose career goes from a seat at the table in the board room to one in the dining room, with intentions ranging from lofty “this is my new passion and life’s work” to the more realistic “this will hopefully pay the bills while I try to get someone to hire me.” I’m only critical when corporate-fueled ego spills over into gig work (I’m thinking about my former boss, who fled back to a health system job before the paint on his consulting company shingle had dried) in the form of of prestigious-sounding company names, splashy websites, and a CEO title for their one-person contract work, and then when the contracts don’t materialize, redirect their unplanned free time into social media and podcast punditry. Still, we all have bills to pay and people to support, so if hanging out a consulting shingle for the short or long term does the job, then be proud of taking the shot with humility, which is required since the phone doesn’t ring nearly as often when you’re a seller instead of a buyer.
HIStalk Announcements and Requests
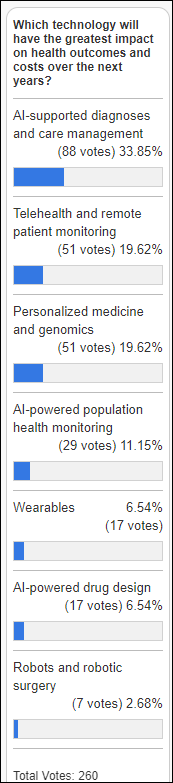
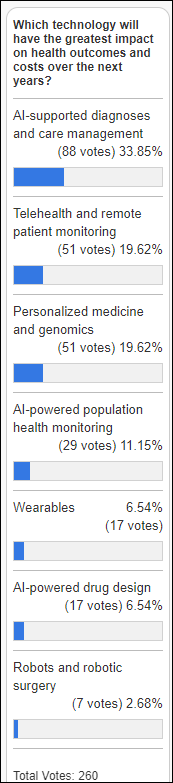
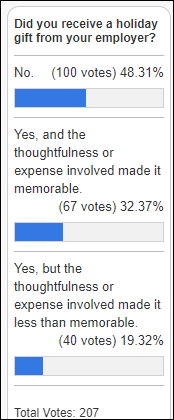
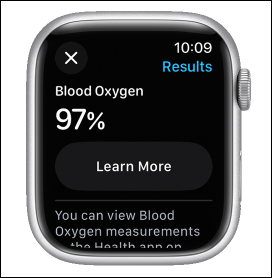
I ran a similar poll to this one nearly a year ago and only the finishing order has changed – the top vote-getters then and now were AI, precision medicine, and remote patient monitoring. Respondents back then showed insight in ranking AI high long before ChatGPTback triggered a now-obvious AI ubiquity.
New poll to your right or here: Provider employees: did your employer see a hard-dollar ROI within a year of funding your attendance at a national conference?
Thanks to these companies for recently supporting HIStalk. Click a logo for more information.








Webinars
January 19 (Friday) 1 ET. “Unlocking Reliable Clinical Data: Real-World Success Stories.” Sponsor: DrFirst. Presenters: Alistair Erskine, MD, MBA, CIO/CDO, Emory Healthcare; Jason Hill, MD, MMM, associate CMIO, Ochsner Health; Colin Banas, MD, MHA, chief medical officer, DrFirst. Health system leaders will describe how they are empowering clinicians with reliable patient data while minimizing workflow friction within Epic. They will offer real-world experience and tips on how to deliver the best possible medication history data to clinicians at the point of care, use clinical-grade AI to infer and normalize prescription instructions in Epic, and encourage patient adherence to medication therapies for optimal outcomes.
January 24 (Wednesday) noon ET. “Medication Management Redefined.” Sponsor: DrFirst. Presenters: Nick Barger, PharmD, VP of product, DrFirst; Caleb Dunn, PharmD, MS, senior product manager, DrFirst. Clinical workflow experts will paint a reimagined vision for e-prescribing that offers enhanced patient adherence, customizable clinical support, intelligent pharmacy logic, and data integrity and safety. Join this first chapter of an ongoing conversation about what medication management should be, how to deliver greater benefits today, and how to prepare for the future. Elevating your solution and customer benefits isn’t as hard, scary, or economically challenging as you may think.
Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock
France-based GPT clinical note generator Nabla raises $24 million in a Series B funding round that values the company at $180 million.
Marshfield Clinic and Essentia Health cancel their planned merger.
Doctors express wariness about drug maker Lilly’s announcement that it will sell some of its drugs directly to consumers using third-party providers of telehealth and pharmacy fulfillment services. The CEO says LillyDirect will make it easier for patients to obtain prescriptions without resorting to compounded or counterfeit versions of products such as its $1,000-per-month weight loss drug Zepbound, but an expert says that LillyDirect is the next step in direct-to-consumer advertising where patients may not learn about treatment options that don’t involve Lilly’s products, also predicting that other drug companies will follow Lilly’s lead. The American College of Physicians responded to the announcement on Friday, expressing its concerns about patients ordering drugs directly from their manufacturer and the approach of “primarily oriented around the use of telehealth services to prescribe a drugmaker’s products.”
Sales
- Brant Community Healthcare System signs up as the first Canadian user of Meditech Expanse as a cloud-based subscription.
People

Kidney testing app vendor Health.io hires Geoff Martin, MBA (Olive AI) as CEO. He takes over from founder and former CEO Yonatan Adiri, who will move to president.
Government and Politics
A home health agency pays $10 million to settle Department of Justice charges that it fraudulently billed the federal government for in-home nursing care that actually involved telephone calls. The cost was billed to a Department of Energy compensation program for people and their survivors who were exposed to radiation from the government’s building of nuclear weapons in the 1940s and 1950s, including employees and nearby residents, that caused long-undetected cancers and birth defects. The program, which was created in 2001, has paid out $23 billion to 137,000 people.
NHS England is reviewing the planned use of social media influencers by Palantir, to which it recently awarded a $415 million contract to develop and operate a national NHS data-sharing platform. The US company says it explored but didn’t actually launch a campaign with New Zealand-based digital agency Topham Guerin, which previously ran Conservative Party campaigns. Palantir’s contract prohibits using NHS’s name without approval. The company planned to pay for posting videos and tweets to correct what it thinks is misinformation about the project, with specific instructions to influencers to not mention Palantir by name or hashtag. The legal non-profit Good Law Project says Palantir is “possibly the dodgiest company ever to gain access to our medical records.”
Online mental health provider Cerebral will pay $540,000 in refunds to New York patients in a settlement with the state’s attorney general, who says the company intentionally made it hard for patients to cancel the subscriptions and instructed its employees to submit fake positive reviews. The AG says the company told subscribers they could cancel via email, but required completion of a survey and then put the cancellation on a multi-day hold while sending them retention offers in hopes of changing their mind. The company also charged customers when it had no providers available to treat them.
Other
In England, a nurse’s hospital employer calls her in for emergency floor coverage, then writes her an $89 parking ticket because her car didn’t have a $50-per-month employee parking pass. She had applied for the sticker, but the hospital admits that it is backlogged on sending them and suggests that employees instead take public transportation.
Sponsor Updates

- Netsmart staff volunteer at the Cornerstones of Care gift gallery to help distribute and wrap gifts for children within the organization.
- CereCore releases a new podcast, “Fostering a Culture of Innovation and Growth.”
- Nym achieves excellent customer satisfaction scores for the second consecutive year.
- Nordic releases a new podcast, “Designing for Health: Interview with Kevin Dufendach, MD and Andy Spooner, MD.”
- The “That’s Derm Good!” podcast features RxLightning founder and CEO Julia Regan.
- Symplr expands its golf sponsorship program with the addition of four-time PGA Tour winner Russell Henley.
Blog Posts
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.







































The New Yorker cartoon of Readers Write articles.