An HIT Moment With … Steve Shihadeh
An HIT Moment With … is a quick interview with someone we find interesting. Steve Shihadeh is founder of Get-to-Market Health of Malvern, PA.

Startups have been forced to adjust their strategies, execution, or expectations as investment activity dropped substantially. How will that change the industry over the next few years and how should companies prepare for a turnaround?
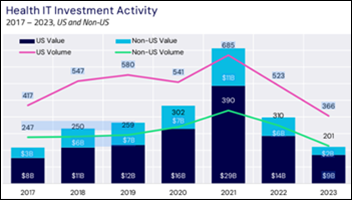
At the end of 2022, and throughout 2023, startups and most mid-sized companies shifted their #1 priority to conserving cash. Forecasts of possible recession and rising interest rates put a damper on spending of all types, and especially the more expensive industry events. Companies lowered expectations, cut staff, and tried to do more with less, or at least hold their own. In my opinion, industry momentum, risk taking, and progress on using tech to improve healthcare were all off course for the last 18 months.
2024 has a much different feel already, with several significant funding announcements and a renewed focus on growth. Digital health investors who showed lots of patience over the last year and a half are pushing for the returns they were promised when their funds launched. As a result, I expect attendance, new product announcements, and customer interest at the big national shows to be on the upswing.
The HIMSS conference has a new owner and competition from ViVE and HLTH, with an emphasis on hosted buyer programs by all three. How would you advise companies to plan their participation in these conferences for maximum return on investment?
HIMSS23 in some ways seemed a little dated. It was big as ever, but when compared to the feel of ViVE and HLTH, it needed a reboot. I guess HIMSS understood that, and I am really curious how the show will change this year under new leadership.
To get maximum returns on your tradeshow investment, I think my assessment last year mostly holds true. The top three of the top 10:
- Pick the most important show for any booth investments.
- Have a presence, even if just one key person, at as many shows that you can.
- Send only your best, most committed people.
What has changed in health tech marketing since the pandemic eased?
The pandemic pushed people to hone great digital marketing skills and tools. That is table stakes today, and now we have the full return to strategic in-person events like trade shows and targeted regional and bespoke events.
The vast improvements in marketing in our space continues to impress me. When I first started Get-to-Market Health in 2017, we presented to a CEO about how we would recommend he revamp marketing. He said something to the effect of, “I am going to just hire a grad assistant type instead.”
That was then. Now, to keep pace, most digital health companies have a strong marketing VP who is directly aligned with the sales VP. Awareness, public relations, lead generation, lead conversion, pipeline development, and deal closure are very much a team effort. Digital tools, social marketing, and micro-targeted outreach are mandatory today, and it is great to see companies taking full advantage of new ways to educate customers.
How will the increased healthcare involvement of big tech firms such as Microsoft, Oracle, and Google affect the ways that healthcare-only vendors run their business?
I was able to see firsthand the impact of a big tech firm committing to healthcare when I was with Microsoft about a decade ago. The company made large-scale market development investments, engaged in key policy discussions that smaller companies just can’t do, and along with Amazon, laid the foundation for the cloud business in healthcare as we know it today.
I am bullish that the big tech firms that stay committed to the space — “stay committed” being the key point — can really drive change and make a difference. I would advise our clients and friends in the space to carefully evaluate who has the staying power before they go all in with one of the bigger players.
What is your advice for health tech startups given the business and industry conditions that you expect over the next two years?
Assuming the general economy stays strong, I see a great run for the companies in our space who have most of these attributes:
- Differentiated products or services.
- Demonstrable ROI that holds up to CFO scrutiny.
- Company culture that your employees enjoy and your clients can feel.
- Sales and marketing teams that work together.
- A thoughtful plan of how to work with or around the big vendors.
Healthcare delivery in the US is complicated. but when it works, is the envy of the world. Technology improvements need to be made in all facets to drive down costs — the US is not the envy of the world on this point — and continually improve care. Every hospital in our country can benefit from all that tech has to offer, which is why I remain so positive on the runway in front of health tech companies.







































Give ophthalmology a break. There aren’t many specialties that can do most of their diagnosis with physical examination in the…