I'd never heard of Healwell before and took a look over their offerings. Has anyone used the products? Beyond the…
News 3/17/23
Top News

VA officials testify before the Senate Veterans Affairs Committee that its Oracle Cerner system has been linked to six incidents of severe patient harm, including four deaths.
Sen. Patty Murray (D-WA), who chairs the Senate Appropriations Committee, threatened to withhold funding for the system’s implementation until problems have been addressed.
Sen. Jon Tester (D-MT) raised questions about why Cerner was awarded a no-bid, $10 billion contract that lacks adequate accountability for patient harm or system downtime. Tester urged the VA to continue its implementation efforts but to renegotiate its contract, which is set to expire on May 17, for more favorable terms. The VA’s top contracting offer responded, “That’s absolutely the plan.”
Sen. Marsha Blackburn (R-TN) said of VA employees, “I have never in my life seen such resistance to modernizing a program. You’ve got a vendor sitting right next to you. They’re making a good faith effort to bring something forward. Why can you not tell employees, ‘This is your job. If you don’t want to do this, go work somewhere else?’”
Reader Comments
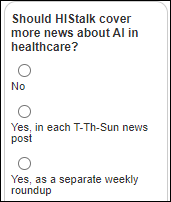
From Bread Zeppelin: “Re: AI in healthcare. Would readers other than me like to have that section added to the HIStalk news posts, similar to the COVID-19 news coverage?” Let’s ask them in this poll, which I’ll also post on LinkedIn to see if anyone notices.
HIStalk Announcements and Requests
I’ve decided that LinkedIn will serve my social media needs best, especially given its significant participation by my decision-making readers, so follow the HIStalk page for updates there. Or stick with Twitter since I’m not abandoning it.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Senior care software vendor PointClickCare acquires Patient Pattern, which offers a value-based care EHR and care management platform.
White-label telehealth services vendor OpenLoop raises $15 million in a Series A funding round. It offers provider staffing as well as services to assist with regulatory monitoring and credentialing. Co-founder and CEO Jon Lensing, MD graduated medical school in 2020 and started the company instead of pursuing a residency.
Maribel Health, which offers solutions to support hospital-at-home and community-based palliative care programs, raises $25 million in a Series A funding round.
Interoperability platform vendor Zus Health raises $40 million in funding and announces that EHR vendor Elation Health will integrate Zus Aggregated Profile to allow clinicians to view expanded records.
Microsoft and its Nuance business announce a Copilot AI-powered feature for Nuance Mix Builder that allows teams to build intelligent chatbots with minimal technical skills. In other AI news, both Microsoft and Google announced that they have added generative AI to their Office and Workspace apps, respectively, that will create draft documents from a user’s description of what they need.
Sales
- UR Medicine Highland Hospital will implement Medaptus Assign to manage inpatient physician assignment.
- FQHC Access Family Care (MO) chooses EClinicalWorks EHR and related modules.
- Lakes Region Mental Health Center will expand its 33-year relationship with Netsmart by adopting its CareFabric platform.
- Zuyderland signs a 10-year renewal with Sectra and will move to its cloud-based enterprise imaging solution.
People


Industry long-timer Peter Butler, president and CEO of MDaudit, retires. He will be replaced by COO Ritesh Ramesh, MS, MBA.

Athenahealth hires Caleb Anderson (Netsmart) as chief sales officer.

Brian White, healthcare partner with LogicSource and long-time health system executive, died Sunday. He was 48.
Announcements and Implementations
Google introduces Open Health Stack to help Android developers create FHIR-based digital health solutions.
An Urban Institute survey of adults ages 18 to 64 finds that 15% of their families have past-due medical debt, most of it involving hospital bills. About 80% of those with overdue medical bills had insurance when the expense was incurred, and while one-third of them were offered a payment plan by hospitals, few hospitals offered to discount the total owed or offered to help them apply for Medicaid. Overall, 100 million US adults have medical or dental bills that they are paying off over time or that are overdue.
TytoCare receives FDA clearance for its AI-powered wheeze detection for remote diagnosis.
Other
I ran across a testimonial from Laurence Beer, MD, chief clinical officer at Transitional Care Physicians of America, on the company’s use of free Chrome browser productivity extension Magical to boost documentation productivity. He set up variables so populate patient details into the EHR note, saving one hour per day per user. He says that clinicians needed six mouse clicks to use an EHR shortcut to start a physical exam note that says “well-nourished, elderly male in no acute distress” while Magical did it with one. The organization distributed the shortcuts as a team list to standardize documentation.
Denmark-based Be My Eyes – which links mobile-connected volunteers to people with vision problems to complete such as identifying a product or navigating an airport — develops a GPT-4 powered Virtual Volunteer version. The new assistant, which is in beta testing, helps users identify household items, avoid fall hazards, hear a summary of web page and search content, and navigate public transportation.
Sponsor Updates
- Metrigy recognizes Five9 as a Contact-Center-as-a-Software MetriStar Award Winner.
- Fortified Health Security names Melissa Schroeder (Oracle) security compliance advisor.
- GHX recognizes North America’s 2022 50 best healthcare providers for supply chain excellence.
- Healthcare Triangle confirms that it does not hold any cash or maintain any accounts at Silicon Valley Bank.
- InterSystems releases a new Healthy Data podcast, “Clinical Staffing – Patient Ratio & Documentation Burden.”
- Konza National Network will present at the AHIMA Advocacy Summit March 20 in Washington, DC.
- Kyruus will exhibit at AMGA March 28-30 in Chicago.
- Kingman Regional Medical Center (AZ) moves toward eradicating hepatitis C with support from Meditech Professional Services.
Blog Posts
- VBC Can’t Work Without Specialists on Board (Enlace Health)
- High Acuity Patients in Urgent Care: Defining and Solving Acuity Degradation (Experity)
- ‘To Err is Human’ Update Finds Inpatient Adverse Events Still a Challenge (First Databank)
- Inefficiencies in EHR Systems Can Cause Healthcare Worker Burnout (HealthTech Resources)
- How to Improve Care for Spanish-Speaking Patients (Healthwise)
- Innovation, Partnerships Driving Nationwide Interoperability to Address Healthcare’s Top Challenges (Surescripts)
- Oracle Cerner RevElate Common Questions and Implementation Tips (Healthcare IT Leaders)
- Rapidly Evolving and Increasing Cyberthreats: Why You Need an IT Assurance Service Program (Impact Advisors)
- 9 HIT conferences to attend in 2023 (Intelligent Medical Objects)
- MEDITECH continues moving health IT forward (Meditech)
- Advancing Interoperability in the Age of TEFCA: An Interview with CommonWell’s Executive Director, Paul L Wilder: Part 2 (Medhost)
- Myndshft Advocates for Da Vinci Standards in Public Comments to CMS Proposed Prior Authorization Rule (Myndshft)
- The Power of Pairing EHR and MDS Data Together for SNFs (Net Health)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.




Regarding the VA/Cerner acclaimed deaths. Blaming an EMR solution for a death is a BIG deal and hard to accept. Doctors and nurses enter orders, tests are ran and interpreted but human intervention (Doctors, Nurses etc) is required to validate and check results for acceptable ranges. Radiologists interpret results based on scans, x-rays etc. Again , doctors look at results and make a diagnosis and prescribe medications, treatment plans etc. Humans treat humans, machines don’t and never should.
I think you may have never used an EHR, or if you did, you did not like it.
I think you may have never used a CPOE and understood how much of the treatment of patients is placed in the EHR/CPOE systems.
Yes, there are instances of stupid where a clinician should have known better as Math described — but if a clinician puts an order in the system, the system accepts the order — then the order being silently swallowed and lost is not the clinicians fault. And would you blame the clinician for not double and triple checking to make sure that the order was not silently failed? There is also the idea that the system is there to help the user, but if the user has several failures in the system, then how do you trust that it is working?
There is also the idea of referential integrity errors. I see the patients chart, but unbeknownst to me, I am actually seeing part of the patients chart, and part of another patients chart. Two, or even three charts displayed under the same patient banner. Who is that diligent that they would double/triple check to make sure the chart they are seeing is for the patient in the banner? Especially if the patient isn’ awake and “that” alert that they understand the questions you are asking.
There are also instances of patient followups that failed to persist. The clinician sees a patient, sets a plan, and sets a followup to go over the results of the plan — 6 months later, is it the responsibility of the clinician to identify the loss of the followup appointment when the system silently dropped the appointment? You seem to expect much of your clinicians.
Now, let’s go to the ED, your patient comes in and is not responsive to questions, you pull up the chart and the wrong information is in the chart — medications unreconciled, problems out of date, procedures as active when they are decades old, adverse reactions listed as full blown allergies, etc. And those mistakes you want to put on the clinicians lap. Interesting.
These things have happened at the VA in the Oracle-Cerner implementation. This may be harsh, apologies if it comes across that way, but you should be looking at data, facts, and events and not subjective opinions about the acceptance of an EHR/CPOE system.
21 years working with the Oracle/Cerner system at many organization sites. Never once have I seen an order get placed and silently swallowed. If you don’t know what chart you have active, there is a preference which can be set BY the VA to limit the number of charts open to only 1 at a time. And for every doc that wants one chart only, 784 docs want some other configuration. This is a VA decision. This is what they will be maintaining for years to come and if their pointing the finger at “the System” now…they’re in for a rude awakening
Yes, let me be clear about my statements. These things have happened at the VA, and these things have caused harm. But, as an example, If the “system” is not well suited to multiple charts being open at a time (that isn’t what was reported — but for arguments sake…) then that needs to be made clear to the implementation team and it needs to be addressed in implementation as a limitation. Again, the reported error was that patient A’s banner was present, along with most of their record, except for a few elements that were from patient B. The failed order problem was something that was reported to have occurred at Banner health in ’17 — but certainly appears to be an uncommon problem.
I am quite sure that Cerner, as a solution in the regular hospital system market, is completely sufficient to task. It is certified and has a pretty loyal base. The implementation of Cerner at the VA is what I am discussing. And, there appear to be multiple causalities to these failures. One is the system is not designed for the needs of the VA. Second, is the idea that each VA VISN is its own unique thing, with different enumerations, settings, value sets, etc. Meaning that each VA VISN will migrate from that VISN into the overall solution as a bespoken migration. Third, by all reports, the implementation team is treating the VA like a regular US based healthcare system, and it isn’t. Fourth, the VA is not particularly good at requirements definition, change control, project management (this is from experience). Fifth, sixth, seventh…
There is plenty of “blame” to go around — and it certainly isn’t just the “system” — but, if we are going to fix the issues as opposed to placing blame, then we will need to address all the causalities or this migration will fail. It is an important migration for a number of reasons, but if the migration is “red” then it needs to be adjusted. Those adjustments need to occur throughout the causality paths: System, Migrations, Definition, Requirements, Workflows, Training, Performance, Change Control, Patient Safety, Validation & Verification, and monitoring.
I hope, that helps clarify my position and thoughts
This term swallow brings back the days of coding on mainframe. Each record entered were tallied at the end of the shift to ensure they all made it to the system. Nowadays who ever heard of a record being swallowed..If u entered a chart and it did not get saved, the system is gonna scream is out in every possible alert/message/pop-up till u a supervisor grade human/role does not get to the the bottom of it with. Most systems provide caching the data entered and not many wait for the user to enter all data before saving.The users of mainframe era need to understand that younger users have more trust with the system. All system can be better..specially EMRs. but please swallowing record is so old school..Does not happen now even if all electricity and battery fails.
That truly cracked me up, thank you.
And yes, that is probably where I got the term, as the Bezier taxonomy of defects is pretty old, but still completely relevant. You can call it “swallowed”, incorrectly transitioned, having an incorrect status, I truly don’t know what the root cause of the events were as they are rarely shared outside of the development groups involved.
But the unintended ‘loss’ of an order is serious as are also the referential integrity and medication prescribing errors. The other errors reported are also serious.
And, the loss of life (4) and catastrophic harm (2) are things that need to be addressed.
I truly don’t want this to fail, as I am a veteran myself, and I know there are large gaps in VistA that need to be addressed. But, if we don’t acknowledge the errors in this implementation then they will not be fixed — regardless of causalities.
I think these congressional reps. should meet with end-users — doctors and nurses on what has happened with all the Cerner implementations. They might learn something very necessary for their comments and decisions.
End users don’t like EMR’s, never have, never will. Talk to any nurse or doctor and if they are not on the record, they will state, “don’t like any EMR as it takes them away from the bedside and patient interaction”.
EMR’s have the ability to have alerts built into them, so much so that alert fatigue is frequently referenced and clinicians will often state they disregard alerts. Other statements such as “the EMR let me do it or it didn’t stop me” has resulted in one respect dependence on the EMR and clinicians moving forward with orders/ actions that should have resulted in human intervention and on the other hand ignoring when convenient. Workflows may be more complicated than necessary but blaming an EMR that is just a set of algorithms when educated clinicians should be using their knowledge to interpret appropriateness of patient care should be addressed before lack of trust in the medical delivery of care is created. The process of checks and balances still needs to be maintained, if a medication order is inappropriate pharmacy should be the next check point and then the one administering the medication.
This reminds me of that story a few years ago where a doctor placed an order in mg/kg instead of mg, had to password override a warning, then the pharmacist got the order, called to verify with the doctor that the dose was correct, then had to password override to fill the order, then a nurse sat down with the (peds) patient and fed him like 30 pills, and after all of that, they blamed the EMR.
I think you’re referring to this: https://www.wired.com/2015/03/how-technology-led-a-hospital-to-give-a-patient-38-times-his-dosage/
It’s a fascinating example of the swiss cheese effect, and should be required reading for every EMR vendor employee and analyst in the world.