News 5/8/24
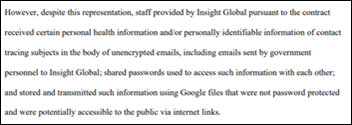
Top News

Multi-state hospital operator Steward Health Care files for Chapter 11 bankruptcy protection and seeks up to $300 million in financing to keep the doors of its 31 remaining hospitals open.
The company blames declining reimbursements from government payers, rising labor costs, and inflation for its current financial state.
The private equity sharks who looted the business and walked away with hundreds of millions of dollars weren’t mentioned.
HIStalk Announcements and Requests
Today I learned (by experimentation) that I can project photos on my phone to the Roku device and thus to our non-smart TV using AirPlay. Flipping through vacation and family pictures on the big screen is a lot more interesting than squinting at them in my palm.
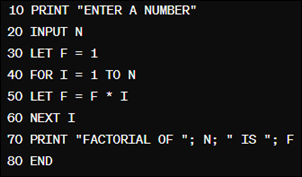
Happy 60th birthday to BASIC. Kudos to those keyboard warriors from the sepia-toned tech trenches of yesteryear who paid the bills or found new careers after mastering DIM, INSTR, and SHELL.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present or promote your own.
Acquisitions, Funding, Business, and Stock

Tech-enabled musculoskeletal care management company Livara Health raises $15 million in Series B funding. The company, formerly known as SpineZone, has raised $27 million since it was launched in 2014 by brothers and orthopedic surgeons Kian and Kamshad Raiszadeh.
Rad AI raises $50 million in Series B financing. The company, which has raised a total of $79 million, offers AI-powered radiology reporting workflow software.
Healthcare cybersecurity solutions vendor Blackwell Security raises $13 million in additional funding and hires Geyer Jones (Cylera) as its first CEO.
Nworah Ayogu, MD, MBA, general manager and chief medical officer of Amazon Clinic, has left the company to join healthcare-focused venture capital firm Thrive Capital.
Sales
- Geisinger Health Plan will implement OncoHealth’s value management and virtual cancer care services. The company’s CEO is industry long-timer Rick Dean.
People

Cone Health (NC) promotes Keith Jones, MHA to CIO.

Kyle Armbrester, MBA (CVS Health’s Signify Health) joins Datavant as CEO.

Dean Dalili, MD, MHCM (DispatchHealth) joins DeepScribe as chief medical officer.

Manifold hires industry long-timer Alex Akers (Health Catalyst) as VP of growth.

Nick Raup, MS (Optum) joins E4health as SVP of AI and automation solutions.
Announcements and Implementations

WVU Medicine Thomas Hospitals goes live on Epic.
Arrowhead Regional Medical Center (CA) works with Tegria to redesign its clinical decision-making governance structure.
MetroHealth (OH) implements Ovatient’s virtual care services. MetroHealth and MUSC Health (SC) created Ovatient in 2022.
NHS National Services Scotland goes live on Rhapsody’s EMPI, hosted in Microsoft Azure.
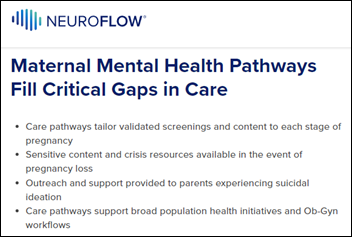
NeuroFlow, which offers behavioral health technology and analytics, launches perinatal and postpartum care pathways to support behavioral health after pregnancy.
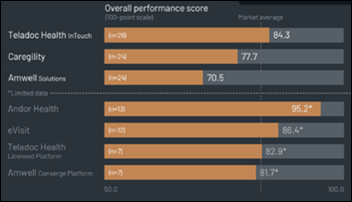
A new KLAS report on virtual care platforms finds that those that are offered by Teladoc Health and Caregility have seen broad adoption, with Teladoc Health’s InTouch seen as a critical tool for expanding specialty coverage. Customers of Amwell report problems with slow development, inadequate support, and high costs, with Epic clients in particular considering replacing it with Epic’s outpatient virtual care offering. Andor Health was noted as being especially flexible, while Best in KLAS 2024 winner for virtual care platforms EVisit is seen as solid for outpatient use cases.
Government and Politics
A health insurance broker sues several companies over a scheme in which a data marketing company gave consumers low-cost health insurance in return for allowing their internet and cellphone usage to be electronically tracked and sold to marketing companies. Customers complained after finding that their “junk” insurance plans offered little coverage.
Sponsor Updates

- AdvancedMD employees volunteer with numerous organizations during the company’s day of service.
- Atrys in Brazil selects enterprise imaging technology from Agfa HealthCare.
- Five9 publishes a white paper titled “Exact Sciences Achieves 45% Containment Rate.”
- Arrive Health publishes a new whitepaper, “The Crushing Weight of Prior Authorization – And What You Can Do About it Today.”
- Artera will exhibit at the OCHIN Learning Forum May 13-16 in New Orleans.
- Nordic publishes a new episode of its “In Network” podcast titled “Designing for Health: Interview with Farhan Ahmad and Jon Keevil, MD.”
- Ascom announces that Premier Inc. has awarded it national group purchasing agreement for its clinical workflow solutions.
- Care.ai adds new members to its Smart Hospital Maturity Model advisory panel.
- Clearwater Chief Risk Officer and Head of Consulting Services and Client Success Jon Moore authors “AI Governance and Strategy Alignment: Empowering Effective Decision-Making.”
- Symplr is recognized as a US Best Managed Company.
- Clinical Architecture releases a new episode of The Informonster Podcast, “Data Quality in Healthcare: Decoding the PIQI Framework.”
- CloudWave will exhibit at the HIMSS New England Chapter Spring Conference May 16 in Norwood, MA.
- Divurgent will present at the HIMSS Virginia Data and Analytics Symposium May 9 in Staunton.
- Healthcare IT Leaders announces it has been named a Workday Staffing Partner.
- The Pacific Islands Primary Care Association and partner HealthEfficient announce that three community health centers involved in their federally-funded Pacific Islands Electronic Health Initiative have implemented EClinicalWorks.
Blog Posts
- Cybersecurity Expert from Defense Weighs in on Healthcare’s Opportunities (CereCore)
- Igniting the Bottom Line to Spark Success for Healthcare Organizations (AGS Health)
- Exploring the impact of electronic patient records on Altera clients in the UK (Altera Digital Health)
- How to safeguard your healthcare data journey with data seatbelts (Arcadia)
- New Insights to Tackle Major Global Health Data Research Challenges (Aridhia Informatics)
- Meet the Clinician – Don Pearce (Ascom)
- Pioneering the Next Frontier of Bidirectional Data Exchange (Availity)
- How Holzer Improved Care While Progressing from Virtual Sitting to Virtual Nursing (AvaSure)
- Embracing Integrated Care Solutions for Mental Health (Bamboo Health)
- Introducing Recovery+ (Bardavon)
- The Quick Guide to Developing an AI Use Policy for Your Organization (Clearwater)
- The Role of Technology in Solving Nursing Challenges (Dimensional Insight)
- The Bots are Here to Help (EClinicalWorks)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.



























Fun framing using Seinfeld. Though in a piece about disrupting healthcare, it’s a little striking that patients, clinicians, and measurable…