Download a PDF copy.
Access

Booth: 2317
Contact:
Kiffer Davis
kiffer.davis@accessefm.com
214.272.0375
Access is the world’s leading electronic forms (e-forms) management, automation and workflow software provider. Our solutions transform any paper-intensive forms process into a paperless, collaborative workflow. Hundreds of hospitals worldwide are using Access solutions to improve patient care and safety, cut costs and enhance electronic health records (EHR), patient safety and downtime registration initiatives. Learn more at www.accessefm.com
Access Says: With Access solutions, you can print e-forms on demand with patient demographics and barcodes that auto index in ECM/EDM systems, paperlessly port clinical device and system output into EHRs, use online forms & electronic workflow to complete physician referrals and back office processes and complete eforms on the fly via mobile devices.
AdvancedMD Software

Booth: 1079
Contact:
BStone@advancedmd.com
801.984.9500
www.advancedmd.com
Practices, Hospitals, RECs, ACOS and Billing Services: If you need a technology platform that can interconnect the smaller private practice into the larger, health community – you need to talk with AdvancedMD, booth 1079. Easy-to-implement, integrated EHR+PM technology, with customizable visit templates for the most “particular” physician and strong revenue management tools for the experienced billing professional. No large upfront capital expenditure. No complex IT infrastructure. Pay-as-you-grow model, scales up and down with business fluctuations. Month-to-month contracts. Put your brand on our application. We invest in our business partners with sales and marketing support.
AdvancedMD Software Says: It takes more than technology to successfully migrate the independent physician into the age of interconnected healthcare. It takes a partner like AdvancedMD. Low cost of acquisition. Flexible technology platform. Marketing and sales support programs.
Allscripts

Booth: 2241
Contact:
Claire Weingarden, Public Relations Specialist
312.447.2442
claire.weingarden@allscripts.com
Allscripts provides innovative solutions that empower all stakeholders across the healthcare continuum to deliver world-class outcomes. The company’s clinical, financial, connectivity and information solutions for hospitals, physicians and post-acute organizations are the essential technologies that enable a connected community of health. To learn more about Allscripts, please visit www.allscripts.com, Twitter, Facebook and YouTube.
Allscripts Says: True care coordination, both inside your organization and throughout your community, requires a single patient record. The new Allscripts, formed by the merger of Allscripts and Eclipsys, has the largest connected provider network in healthcare and provides connectivity for one patient record, on the industry’s first open platform.
API Healthcare

Booth: 3463
Contact:
Scott Smith, Vice President of Global Sales
262.685.8309
scott.smith@apiheatlhcare.com
www.apihealthcare.com
API Healthcare is a leading provider of fully integrated healthcare-specific workforce management solutions. Full integration equates to a more satisfied, cost-effective workforce that is empowered to provide high quality patient care. Learn how your organization can improve workforce management processes – both in terms of the cost and quality of care delivered.
API Healthcare Says: Delivering the advanced integration capabilities that connect your workforce with your clinical and financial data, API Healthcare Synergy is the future of workforce management. Stop by and see how technology that fosters an alliance of goals between finance and nursing can achieve more positive clinical outcomes and a healthier bottom line.
Special Give-away Just for HIStalk Readers: API Healthcare will have a special drawing just for HIStalk readers for a Dell Inspiron Mini Netbook with an Intel® Atom™ Processor. Stop by booth #3463, mention HIStalk, and we’ll swipe the badge for chance to win.
AsquaredM

Meetings By Request
Contact:
Victor Arnold
www.asquaredm.com
info@asquaredm.com
573.256.1135
We specialize in working with hospitals and their physician partners to better align interest, rewards and operations. We provide game changing services in three areas:
– Finance Operations Advisory Services
– Revenue Cycle Improvement
– Integration with EHR Products
In each of these service areas we have a well defined methodology consisting of assessment, advice and transformation. Our mix of management and healthcare consulting experience helps you to choose a solution that works best for your unique organization to drive up revenue and increase operations efficiency.
AsquaredM Says: We "sat in the seat" of management before we ever became consultants. Therefore we understand what it takes to implement sustainable improvements in complex healthcare environments. Few others can actually make that claim.
Awarepoint

Booth: 1901
Contact:
Valerie Fritz, Senior VP of Marketing
858.345.5009 | 1.888.860.FIND
www.awarepoint.com
www.awarepointblog.com
vfritz@awarepoint.com
Analogous to indoor GPS, RTLS solutions are used in hospitals to locate key equipment and maintain optimal inventory; track patients and personnel (to impact throughput, improve workflows and track exposure to infection); and for condition monitoring to meet regulatory compliance requirements such as in temperature controlling equipment (refrigerators, freezers, warmers). Today, Awarepoint leads the enterprise-wide RTLS in healthcare industry, with more hospital sites, more assets under management and more square footage of RTLS network coverage.
Awarepoint Says: Effective Hospitals are Aware. Is Yours? We encourage you to visit Awarepoint at HIMSS Booth #1901 to experience our complete line of RTLS solutions, latest innovations and see a live demonstration to learn more about how hospitals can account for equipment, patient, personnel and processes throughout the enterprise, as well as understand resource status, usage and availability in more depth. And, Awarepoint’s dedicated ZigBee®-based RTLS eliminates threats of data loss and other IT complications to your Wi-Fi network – because interference, interruption and downtime are not an option. If we miss you at HIMSS, contact us at info@awarepoint.com for your unique RTLS Impact Analysis summarizing projected quality, efficiency and cost savings using your hospital’s specific data and Discover the Awarepoint Difference.
Billian’s HealthDATA/Porter Research

Booth: 4579
Contact:
Jennifer Dennard, Social Marketing Director
678.569.4872
www.BilliansHealthDATA.com/
www.PorterResearch.com
jdennard@billian.com
Billian’s HealthDATA is a provider of comprehensive information on healthcare contacts and facilities across the continuum of care, including healthcare IT, via its Portal online sales prospecting and lead generation tool. Partner Porter Research offers in-depth market research services for the healthcare industry.
Billian’s HealthDATA/Porter Research Says: Looking for accurate, real-time healthcare information on facilities across the United States that is updated daily and accessible anywhere – including via phone? Stop by booth #4579 to view a live demo of how the Billian’s HealthDATA Portal can help your sales team stop wasting time on finding qualified leads and start generating sales. Be sure to ask how partner Porter Research’s market research services can help take BHD data to the next level – whether that be via Bulletin Board Focus Groups for new product development, Win/Loss or Competitive Analysis, or White Paper Development, among many other services.
Special Give-away Just for HIStalk Readers: We’ll be offering Snack Packs to the first 100 people to stop by and mention they are a HIStalk reader.
CapSite

Meetings By Request
Contact:
Leela Hauser
802.922.9961
leela.hauser@capsite.com
www.CapSite.com
CapSite™ is a healthcare technology research and advisory firm. Our mission is to help our healthcare vendor and provider clients make more informed strategic decisions that will enable them to accelerate the growth of their business. The CapSite™ database is the trusted, easy-to-use online resource providing critical knowledge and evidence-based information on healthcare technology purchases. CapSite™ provides detailed transparency on healthcare technology pricing, packaging and positioning.
CapSite Says: Schedule time with us to check out our latest industry research reports (including our Ambulatory EHR & Practice Management Study and Revenue Cycle Management Study) or for a quick demo of the CapSite Database.
CAP STS

Meetings By Request
Contact:
Joe Schramm, Director, Business Development Services and Operations
224.223.5464
jschramm@cap.org
CAP STS (SNOMED Terminology Solutions™), a division of the College of American Pathologists (CAP), is a professional services provider with a diversified service offering related to health IT strategy and planning; clinical health information management; and health care standards. CAP STS is committed to improving patient care through the advancement of interoperable EHRs and works with provider organizations, hospitals, health IT vendors, health information exchange initiatives, universities, research centers, and government agencies throughout the world. CAP STS’ DIHIT (Diagnostic Intelligence and Health Information Technology) team advances health IT standards, practices, and tools, such as the CAP Diagnostic Work Station initiative; and standardized electronic reporting, including the CAP electronic Cancer Checklists (CAP eCC).
CAP STS Says: CAP STS is committed to improving patient care through the advancement of interoperable EHRs—and helping clients navigate complex issues and meet Meaningful Use and HITECH Act.
Capsule

Booth: 1931
Contact:
Karen Jimenez
978.482.2340
www.capsuletech.com
karenj@capsuletech.com
For more than 14 years, Capsule has been the world’s leading, award-winning provider of solutions for medical device connectivity. Our leadership is made possible through our 510(k) cleared software and medical grade hardware products, our unique expertise in device protocols and firmware, and our strong partnerships with nearly every major medical device manufacturer and HIS company. Our proven Enterprise Medical Device Connectivity Solution, chosen by over 650 facilities, features a patient-centric, vendor neutral design that allows hospitals to connect virtually any medical device, to any information system, in any unit of the hospital. Featuring the innovative Capsule Neuron™ platform, the solution actually integrates with existing technologies and infrastructures and works within the established or planned caregiver work processes. Furthermore, Capsule’s solution is completely flexible and scalable thereby allowing a hospital to grow as their needs grow to meet their short and long term connectivity, patient care, and safety needs.
Capsule Says: Capsule’s proven Enterprise Medical Device Connectivity Solution, chosen by over 650 facilities worldwide, features a patient-centric, vendor neutral design that allows hospitals to connect virtually any medical device, to any information system, in any unit of the hospital.
Carefx

Booth: 4543
Contact:
Amy Ferretti, Vice President of Marketing
480.833.5010 ext. 446
www.carefx.com
aferretti@carefx.com
Carefx is a leading provider of interoperable workflow solutions and supports healthcare organizations in achieving their vision of advancing the quality and safety of patient care delivery. Carefx supports more than 700 hospitals, health systems, regional health information organizations (RHIOs) and health information exchanges (HIEs) across North America and Europe.
Carefx Says: Come by the Carefx booth to learn how customers are responding to industry and regulatory changes—all while achieving High-Performance Healthcare (pick up a copy of our newly released White Paper on the topic). See Carefx’s new Business Intelligence dashboards (originally developed and implemented at Cleveland Clinic). Of course, our booth is always good for a little bit of fun, too.
CareTech Solutions

Booth: 1831
Contact:
Anne Santori, Public Relations Manager
248.823.0908
248.312.8385 (M)
anne.santori@caretech.com
www.caretech.com
CareTech Solutions, Inc., an information technology and Web products and services provider for more than 150 U.S. hospitals and health systems, creates value for clients through customized IT solutions that contribute to improving patient care while lowering healthcare costs. From implementing emerging technologies to supporting day-to-day IT operations, CareTech offers clients expert health information management services across the entire patient data lifecycle earning it the 2008, 2009 and 2010 Best in KLAS award for IT Outsourcing (Extensive) as ranked by healthcare executives and professionals in the Top 20 Best in KLAS Awards: Software & Professional Services report. For more information, please visit www.caretech.com.
CareTech Solutions Says: You could win a $1,000 donation for your hospital foundation when you stop by CareTech Solutions’ booth and enter the raffle drawing that celebrates healthcare’s extraordinary people doing extraordinary things. To learn more visit http://www.caretech.com/HIMSS_Raffle.
Clairvia

Booth: 3123
Contact:
Phillip Madden, Vice President, Client Services
919.382.8282 ext.231
pmadden@clairvia.com
info@clairvia.com
www.clairvia.com
Clairvia serves more than 1,200 healthcare organizations, medical facilities, nursing departments, and group practices with advanced software solutions for patient and staff management. Clairvia Care Value Management (CVM) is a comprehensive software suite that empowers healthcare providers to deliver the right caregivers to each patient – at the right time – to achieve the next, desired level of wellness. In more than 200 successful implementations, Clairvia CVM has driven measurable improvements in quality of care, patient safety, patient throughput and financial performance, as well as patient, staff, and physician satisfaction. The complete Clairvia CVM solution includes the following software products: Staff Manager | Care Cost Manager | Demand Manager | Patient Progress Manager | Outcomes-Driven Patient Acuity | Demand-Driven Patient Assignment | MobileConnect | ShiftAlert Mobile.
Clairvia Says: Clairvia’s Physician Scheduler software automates the demanding, time-intensive task of creating an equitable schedule based on the complex rules of individual physician groups, while ensuring an equitable share of call and adequate coverage.
Culbert Healthcare Solutions

Meetings By Request
Contact:
Brad Boyd, Vice President
Culbert Healthcare Solutions, Inc
781.935.1002 ext 13
bboyd@culberthealth.com
www.CulbertHealth.com
Culbert Healthcare Solutions specializes in assisting healthcare organizations with strategic planning, interim management, revenue cycle, clinical transformation and information technology services. Our team of experienced healthcare professionals thrives on implementing best practices, optimizing technology and guiding clients through the change management process.
Cumberland Consulting Group

Booth: 6943
Contact:
Jim Lewis, Managing Partner
615.373.4470
www.cumberlandcg.com
jim.lewis@cumberlandcg.com
Cumberland Consulting Group is a national technology implementation and project management firm serving ambulatory, acute, and post-acute healthcare providers. Through the implementation of new technologies, Cumberland works with providers to advance the quality of care delivered, and improve business performance. Named one of America’s Best Small Firms to Work For by Consulting Magazine in 2008, 2009 and 2010. Cumberland Consulting Group offers an invigorating, positive work environment and a commitment to superior talent acquisition, development and retention.
Cumberland Consulting Group Says: Make meaningful use of your time at HIMSS 11. Stop by and learn why Cumberland doubled in size in 2010. Cumberland has an excellent delivery record, straightforward implementation methods and lean operating model that delivers big company results at a very attractive price. Be sure to catch partner Dave Vreeland’s presentation on designing EMR programs for Voluntary Medical Staff: Session 223 on Thursday at 11:15.
Special Give-away Just for HIStalk Readers: Mention our listing in the HISTalk HIMSS Guide and be entered for a chance to win the top-of-the-line 64GB WiFi Apple iPad!
CynergisTek
Booth: 4118
Contact:
Caroline Kirby, Director of Marketing & Business Development
512.402.8550
caroline.kirby@cynergistek.com
www.cynergistek.com
CynergisTek delivers a powerful combination of information security consulting and proven technologies that enables organizations to efficiently protect their information and comply with regulatory requirements. With decades of experience in the healthcare and IT security industries, the company offers its clients authoritative guidance for practical, data-centric approaches to solving specific security challenges, from fundamental HIPAA compliance to the complex, evolving regulatory requirements associated with the HITECH Act and healthcare reform.
dbMotion

Booth: 2063
Contact:
Kate Kolbrener, Sr. Marketing Mgr, N. America
412-802-2248
www.dbmotion.com
katek@dbmotion.com
dbMotion is an innovative provider of health interoperability solutions for connected healthcare. The dbMotion™ Solution is a proven SOA-based platform that enables healthcare organizations and HIEs to meaningfully integrate and leverage information assets to drive improvements in the quality, safety and efficiency of patient care.
dbMotion Says: You will not want to skip a visit to the dbMotion booth this year at HIMSS! There you will have the chance to speak with our clients who are enjoying the benefits of truly connected healthcare such as genuine care coordination embedded within the caregivers’ workflow, mobility, payor/provider integration, analytics, ACO – all enabled by dbMotion’s technology.
Digital Prospectors Corp

Booth: 968
Contact:
Chris Roos, Principal
603.772.2700 x201
croos@dpcit.com
DPC provides healthcare organizations with project management, implementation, integration, end user training and legacy systems support. Over the last eleven years DPC has helped dozens of hospitals achieve their IS goals and stay within their planned budget. Integrity, reliability and delivery of outstanding results are the key factors for the continued success of DPC’s HIS practice. Our Consultants are experts in Epic, Siemens, Eclipsys and Quovadx. Come visit us at Booth #968 and register to win an ipad.
DPC Says: Work with DPC when you need reliable, experienced and certified consulting resources to help manage, implement, customize and support your EHR/EMR and HIS Financial systems.
DIVURGENT

Meetings By Request
Contact:
Colin Konschak, Managing Partner
info@divurgent.com
757.213.6875
www.DIVURGENT.com
DIVURGENT, a healthcare consulting firm focused on providing advisory services, revenue cycle management, project management, and clinical transformation services, will be attending the 2011 HIMSS conference Saturday, Feb. 19 – Thursday, Feb. 24. They look forward to meeting new healthcare industry leaders and sharing insight on trending topics. DIVURGENT will be presenting at 11:15 am on Thursday the 24th; Presentation # 229. Reach out to info@DIVURGENT.com if you are interested in meeting.
e-MDs

Booth: 5669
Contact:
Mike DeMuth, Executive VP of Sales
512.257.5200
sales@e-mds.com
www.e-mds.com
e-MDs delivers the most highly rated EHR/Practice Management solution in the United States. e-MDs, with over 30,000 users nationwide, offers affordable, easy to use products for small practices and enterprise organizations alike. As a physician informaticist led EHR company, e-MDs is committed to demonstrating how biomedical knowledge, coupled with powerful, simple to configure and customize HIT products, can improve the quality of healthcare. Through the accurate coding and practice optimization tools of e-MDs Solution Series™, many providers realize marked revenue enhancements well in excess of the HITECH incentive payments.
e-MDs Says: Visit us at Booth# 5669 and see why e-MDs IT-friendly integrated solutions received 2010 Best in KLAS in the Ambulatory EMR (2-5 physician) category, and 2010 Best in KLAS for Practice Management (2-5 physician). And get a sneak peek at our Mobile Solutions coming soon!
eClinicalWorks

Booth: 2311
Contact:
866.888.6929
www.eclinicalworks.com
sales@eclinicalworks.com
eClinicalWorks offers a comprehensive EHR and practice management solution, allowing practices to improve efficiency and enhance patient care. With more than 50,000 providers and 225,000 medical professionals across all 50 states using its technology, customers include physician practices, out-patient departments of hospitals, health centers, departments of health and convenient care clinics.
eClinicalWorks Says: At booth 2311, eClinicalWorks will be showing Version 9 of its Comprehensive Electronic Health Records and Practice Management Solution, along with 100MillionPatients.com and eClinicalWorks P2P, our new integration platform.
EDIMS

Booth: 2031
Contact:
Jamie Kohl, VP Marketing and Strategy
973.220.9577
www.edims.net
kohlj@edims.net
EDIMS 2.6 is CCHIT and MU certified –an advanced emergency department EHR, fully interoperable and ready to install out of the box with over 1000 evidence based medicine templates and order sets. EDIMS experienced team of ED professionals provides peer-to-peer training and support, optimization, customization and express implementation options. With industry leading clinical decision support, a robust charge capture engine, and the quickest and easiest to use documentation system, EDIMS improves profitability and productivity for every ED.
EDIMS Says: EDIMS will have several of their current clients on hand to discuss lessons learned from implementing and using a best-in-breed EMR. Booth activities will include playing Xbox Kinect, adult beverages, guest speakers, multiple give-aways, including a raffle for a great vacation to view the last shuttle launch, and of course opportunities to demo the product.
Elumin Healthcare Solutions

Meetings By Request
Contact:
Mark Williams, CEO
866.597.5861 ext. 707
425.369.8211
www.eluminhs.com
mwilliams@eluminhs.com
Elumin Healthcare Solutions is a privately held premier national technology implementation and project management firm serving ambulatory, acute, and post-acute healthcare providers. Our comprehensive range of programs and services includes system implementation, integration, optimization, project management, custom reporting, education and knowledge transfer expertise. We primarily focus on the Allscripts, Cerner, Epic, and Siemens, customer bases. We strive to successfully establish and maintain long term relationships by providing experienced professionals who consistently exceed their customers’ expectations. Come out of the dark and let our expert consultants shed light on your projects. Become Illuminated!!
Elumin Healthcare Solutions Says: Contact us to arrange a personalized meeting where we can focus on you and your organizations projects. Elumin possess an excellent delivery record, coupled with straightforward implementation methods and a lean operating model offers clients big company results at a very attractive price. Our clients appreciate our business approach and the small firm commitment and personal attention we provide. We’ve been in healthcare IT for 20+ years and are invested in the success of each client.
Emdeon

Booth: 2201
Contact:
www.emdeon.com/HIMSS11
Emdeon. Powering Clinical Information Exchange. Emdeon powers the exchange of clinical information. By using Emdeon’s existing independent national health information network hospitals, physicians, labs, pharmacies and other healthcare stakeholders are able to securely and cost-effectively exchange patient-centric information. With Emdeon, customers gain access to tools that help enable accountable care, achieve Meaningful Use and maintain regulatory compliance.
Emdeon Says: Stop by Emdeon booth 2201 at HIMSS in Orlando, February 21-23 to learn more about how Emdeon powers the exchange of clinical information and hear presentations from industry known speakers. 16 iPads® will be given away during Emdeon’s in-booth speaking events!
Special Give-away Just for HIStalk Readers: We are giving away one iPad just for HIStalk readers. Come by the booth for any of our speaking events and write “HIStalk rocks!” on your entry form. You will be entered to win the iPad drawing during the speaking event and again for a HIStalk specific drawing. That’s double the chance to win for each speaking event you attend!
Enovate

Booth: 2738
Contact:
Tommy Hodge
thodge@enovateit.com
248 655 0548 ex 112
c 734 891 4620
f 847 890 6131
Headquartered in Canton, Michigan, Enovate is a national provider of mobile and wall mounted clinical workstations for the healthcare environment. Enovate provides multiple solutions for medication delivery, computerized physician order entry, clinical documentation, and electronic medical records and services. Enovate – advancing health information technology. For more information, please contact Enovate at (877)258-8030 or visit www.enovateusa.com.
Enovate Says: See our new products including the new e900 series, sign up to win an iPad.
Enterprise Software Deployment

Booth: 2777
Contact:
David Tucker, VP of National Sales
512.350.1735
www.enterprisesoftwaredeployment.com
dtucker@enterprisesoftwaredeployment.com
We assist healthcare organizations implement new EHR technology in the most efficient way possible by preparing organizations for implementation. Through the help of our configuration experts, we train your staff with experienced clinical trainers and stay with you through activation to ensure your go-live runs smoothly. Whether it’s time to implement a whole new system throughout your organization or just a component to one department, we have the experience and resources to both complement your team, and meet your goals.
Enterprise Software Deployment Says: Are your feet aching from walking around the show? Come stop by our booth for a pair of cozy flip flops! Perfect for the Orlando beach, resting your tired conference feet, or for just hanging out in our booth that features an nice grassy floor and some healthy goodies! You can also register for your chance to win a FLIP Handheld Camcorder.
Special Give-away Just for HIStalk Readers: Tired of all of the ARRA rumblings? Well turn up the Sonos, and turn down the stress with a Sonos Music System! ESD will be having a special drawing specifically for HIStalk readers. Sign up at our booth (#2777) and mention specifically that you are a HIStalk reader to qualify.
FormFast

Booth: 4963
Contact:
Laura DeVries, Director of Marketing
www.formfast.com
ldevries@formfast.com
800.218.3512
Since 1992, FormFast software has enabled healthcare organizations to achieve significant lean process improvement across the enterprise, supporting HR, contract management, rogue clinical processes, risk management and countless other workflows. A top-ranked provider of electronic workflow solutions, FormFast serves more than 850 hospitals internationally. Our easy-to-use software helps healthcare organizations accelerate their progression from time-consuming manual processes to fully automated workflows.
FormFast Says: Become a lean high performance hospital with FormFast. Stop by booth #4963 to learn how our solutions can help your hospital gain efficiency, improve coordination of tasks, reduce supply costs, and eliminate errors resulting from misdirected routing, mistakes in form completion and delayed delivery.
GetWellNetwork

Booth: 3635
Contact:
Tony Cook, Vice President Marketing
240.482.3200
www.getwellnetwork.com
info@getwellnetwork.com
GetWellNetwork offers the first digital platform — using the bedside TV in the hospital, TV or Web at home — that entertains, educates and empowers patients to throughout the care continuum, from pre-admission to home. This patient-centered approach enables hospitals to engage patients throughout their journey leading to increased patient activation, higher satisfaction, lower cost per case and better compliance with Meaningful Use Standards. The company is recognized by KLAS® as the leader in the new interactive patient systems category. The GetWellNetwork interactive patient care solution is exclusively endorsed by the American Hospital Association.
GetWellNetworks Says: Expand your hospital’s patient-centered care to the entire patient journey. From pre-admission through post-discharge, empower patients to take a more informed and active role in their care. The results are improved patient satisfaction, clinical quality and enhanced financial operations.
Greenway Medical Technologies

Booth: 2430
Contact:
Laura Mendenhall, Trade Shows Coordinator
404.309.9326
lauramendenhall@greenwaymedical.com
Greenway Medical Technologies, Inc. provides a fully interoperable EHR and practice management solution PrimeSUITE® 2011 that integrates clinical, financial and administrative tasks to streamline the entire patient encounter. The platform also allows for tight data exchange and application networking to combine the needs of ambulatory and hospital systems. Custom templating currently in use by more than 30 specialist and subspecialty practices also allows for greater flexibility and long-term results.
Greenway Medical Technologies Says: Having earned 11 KLAS awards in seven years while also staying current on 2011 ambulatory CCHIT certification and the addition of ONC-ATCB Complete Stage 1 2011/2012 Meaningful Use certification, Greenway’s PrimeSUITE® 2011 electronic health record (EHR), practice management and interoperability platform is a successful long-term business solution. See why CCHIT granted PrimeSUITE 2011 a 5-star usability rating. Visit www.meetgreenway.com to hear from our customers.
Hayes Management Consulting

Meetings By Request
Contact:
Joy Tewksbury-Pabst
Joy@hayesmanagement.com
617.559.0404 ext. 235
www.hayesmanagement.com
Hayes works with healthcare organizations across the country to improve quality, efficiency and the bottom line. Our work ultimately leads to greater clinician, staff and patient satisfaction. Many of Hayes consultants are clinicians, and many have worked in hospitals and physician practices as business and clinical leaders. They are also certified and experienced in premier technologies such as Epic, GE Healthcare, Allscripts and NextGen. On average, our consultants have more than 15 years of experience.
We have been ranked Top Overall Professional Services Firm by KLAS* for four consecutive years (2007-2010). Hayes is 100% focused on healthcare. Seventy-five percent of our annual business is from repeat clients. Hayes’ services include: IT strategic planning, ICD-10, 5010 migration, system implementations, data conversions, revenue cycle management, and interim staff.
Hayes Says: We’re available for networking/coffee/lunch at HIMSS. Please contact Joy Tewksbury-Pabst at Joy@hayesmanagement.com or call her at 617-559-0404 ext. 235 to set something up!
Healthcare Innovative Solutions

Booth: 4023
Contact:
Cody Calapa, BS BME, Vice President, Project Development
800.236.0141
www.CustomizedEHR.com
info@hisorg.com
Founded in 2001, Healthcare Innovative Solutions (HIS) delivers advanced consulting, systems implementation, optimization, and redesign services for any size hospital. Our customers range from large multi-facility health systems to small community hospitals. Several of our customers have received national recognition for EHR and CPOE adoption directly related to our work.
Healthcare Innovative Solutions Says: The HIS Difference is over 20 years of CPOE/EHR consulting expertise. Stop by booth #4023 to learn more about our clinician-focused approach, our team of clinicians and clinical process engineers, and our new CPOE workflow planner software, Pillars.
Holon Solutions

Booth: 2475
Contact:
Sandra Schafer, VP Marketing
678.324,2939
sschafer@holonsolutions.com
www.Holonsolutions.com
Holon’s brings a new way of thinking about interoperability. We convert information from disparate systems into consumable formats, automate routine processes and provide comprehensive workflows to manage all of your information sharing needs. Holon is setting a new standard for delivery of actionable information managing both delivery and viewing preferences and enhancing and extending current systems to deliver information WHEN, WHERE and HOW you need it. For more information please visit us at www.HolonSolutions.com.
Holon Solutions Says: Visit Holon Solutions to see interoperability in action and learn how Holon can deliver tailored, comprehensive services and solutions to help you put meaning into your exchange of healthcare information.
HT Systems / PatientSecure

Booth: Innovation Technology Pavilion 218-10
Contact:
Carl Bertrams, SVP, Sales & Marketing
630.464.6002
www.patientsecure.com
cbertrams@patientsecure.com
HT Systems is a healthcare technology leader, providing the latest innovation in patient identity management. PatientSecure™, the company’s flagship Biometric Patient Identification Management System, links the biometric palm vein pattern of the patient to their medical record in any HIS registration, EMPI or EMR system. HT Systems is the first to successfully implement a large scale biometric patient identification system in the nation. PatientSecure is currently installed at over 50 hospitals and hundreds of affiliated clinics and physician practices, with more than 2 million patients enrolled.
HT Systems Says: Come join us to learn from your fellow healthcare systems about their experience with PatientSecure, an award-winning biometric patient identification system. Orlando Healthcare Systems is going to share their story on their successful implementation of PatientSecure at 4:15pm on 2/22 Tuesday at Innovation Technology Pavilion. Register with us in advance and enter the raffle to win an Android-based Tablet PC! Email to marketing@patientsecure.com.
Iatric Systems

Booth: 3601
Contact:
John Danahey, Vice President, Sales and Marketing
978.805.4153
John.Danahey@iatric.com http://www.iatric.com
Iatric Systems is a leading provider of software applications, interfaces and reporting solutions for healthcare information systems. Our solutions help healthcare professionals optimize patient care while improving clinical, financial and administrative workflow.
Iatric Systems Says, “Interoperability is all about connections – connecting to patients, to providers and to communities. Iatric Systems has the solutions that make these connections and can put your healthcare organization on the forefront of Interoperability.
Special Give-away Just for HIStalk Readers: In recognition of Mr. HIStalk’s appreciation for music, Iatric Systems will be giving away three (3) $50 iTunes Gift cards. Simply stop by the Iatric Systems’ booth and mention HIStalk and we will enter you in the drawing. Three random winners will be chosen at the end of the show and the iTunes gift cards will be mailed to the winners.
ICA

Booth: 2837
Contact:
John Tempesco, Chief Marketing Officer
615.866.1465
john.tempesco@icainformatics.com
www.icainformatics.com
Informatics Corporation of America’s (ICA) health information exchange (HIE) solutions, originally envisioned by practicing physicians at Vanderbilt Medical Center, capture, integrate and provide comprehensive patient data from numerous and disparate installed systems. ICA adapts and deploys this pioneering technology to design and deliver comprehensive HIE solutions to hospitals, IDNs, communities and states generating cost efficiencies and improving patient care and outcomes. ICA’s solutions align with physician workflow empowering caregivers to make informed decisions at the point-of-care with standards-based interoperability to help health care enterprises achieve operational efficiencies across multiple providers and settings. Visit www.icainformatics.com, follow us on Twitter at www.twitter.com/icainformatics, and Facebook at www.facebook.com.
ICA Says: Come preview the most comprehensive and easiest to use portal for the most comprehensive and powerful health information exchange available today. Visit Booth #2837 to see how clinics, hospitals, IDNs, communities and states are exchanging health information easily and quickly, using existing systems, and bringing patient information to the point-of-care and the moment-of-need.
iMDsoft

Booth: 1050
Contact:
Steve Sperrazza, Vice President Sales, North America
866.4 iMDsoft
781.449.5567
iMDsoft is a leading provider of Clinical Information Systems for critical and perioperative care. The company’s flagship family of solutions, the MetaVision Suite, was first implemented in 1999. It captures, documents, analyzes, reports and stores the vast amount of patient-related data generated in a hospital. Over 125 hospitals worldwide use MetaVision to support their workflow, and arm their healthcare professionals with timely, accurate, and actionable information. iMDsoft products demonstrate 100% implementation success rate and a 100% customer retention rate.
iMDsoft Says: Come visit our booth to find out why 4 of the top 10 US hospitals have decided that MetaVision is the best choice for improving care quality and financial performance. Learn more about how MetaVision interoperates with the latest technologies, and seamlessly integrates with all standard hospital systems. Hear how Lehigh Valley Health Network reduced mortality by 31% on Wednesday, February 23, at 10:00 AM when Ethan D. Gershon, MD, Chief Medical Informatics Officer, iMDsoft, speaks about “Tele-ICU, Reduced Mortality, and Continuous Improvement.
Imprivata

Booth: 3872
Contact:
Jim Whalen, VP Sales – Healthcare
781.674.2700
www.imprivata.com
sales@imprivata.com
Imprivata is the leading authentication and access management solution for simplifying password management and securing user access to patient health information.
Imprivata Says: Stop by Imprivata’s booth # 3872 to see live presentations from CIOs and CMIOs on how Imprivata’s solutions enable faster EMR access for their clinicians at their hospitals – with no clicks, no passwords and no problems. You can also test Imprivata’s #1 KLAS-rated single sign-on and access management solutions for yourself at one of our four live demo stations.
Ingenix

Booth: 1163
Contact:
800.765.6713
www.ingenix.com
engage@ingenix.com
Ingenix is a leading provider of health information, technology and consulting services. In an effort to provide health care organizations with an end-to-end capabilities and expertise, we have brought together some of the health care industry’s leading companies, including Picis, Lynx, Axolotl, Executive Health Resources and A-Life Medical. By combining these services and technology, Ingenix will provide a single vendor solution that helps health care organizations solve their most significant challenges to clinical and financial performance improvement and simplify the administrative complexities of health care. Visit www.ingenix.com for more information.
Ingenix Says: Much is riding on the decisions and actions health care professionals make in 2011. The ICD-10 implementation deadline is just two years away; new health care laws will soon require greater coordination of patient care and the ability to share critical patient and clinical information quickly; and Meaningful Use rules now detail what health care providers must do to receive federal incentives and avoid future penalties. HIMSS attendees will be looking to hear real-world success stories around these topics, plus developing accountable care organizations, establishing health information exchanges and accelerating clinical and financial performance improvement.
Intellect Resources

Meetings By Request
Contact:
Tiffany Crenshaw, President/CEO
tcrenshaw@intellectresources.com
Anne Sydnor, Manager Client Services
asydnor@intellectresources.com
www.intellectresources.com
Intellect Resources is a search firm specializing in full-time and contract placements in the healthcare It industry, primarily in core HIS implementations. We’ve been working exclusively in the industry since our inception twelve years ago and serve the recruiting needs of both hospitals and consulting firms.
Intellect Resources Says: Finding resources is a current challenge for new and ongoing implementations. Feel free to reach out to our team. We are always happy to provide insight on and discuss the current and future talent pool.
Intelligent Medical Objects

Booth: 3517
Contact:
Melinda Watman, VP of Strategic Relationships
www.e-imo.com
melinda.watman@imo-online.com
Intelligent Medical Objects (IMO®) develops and licenses medical vocabularies that allow clinicians to capture clinical intent when documenting in EHR systems while at the same time attaching the guaranteed billing codes. IMO has market-leading clinical interface terminology products that cross link standardized vocabularies such as SNOMED CT®, ICD-9, CPT®, MeSH, UMLS, and now even ICD-10-CM, that are necessary for healthcare organizations to connect providers with patient records, administrative information, academic references, decision support content and consumer information. This allows healthcare professionals to focus on patient care rather than administrative details. Products include Problem (IT), a vocabulary database allowing clinicians to enter diagnoses into clinical systems using common, familiar and desired terms; Procedure (IT), a powerful master index used to enter procedure terms quickly and easily for charge capture; Medical Necessity, which provides organizations with the tools they need to integrate reimbursement checking and iHealthSearch™, an intelligent search portal for content.
Intelligent Medical Objects Says: IMO’s suite of vocabulary products can go a long way to ease the transition to ICD-10-CM, which you can learn about along with our groundbreaking new Procedure IT solution at our booth (3517). While there, take “The IMO Challenge” to see if you have what it takes to stump our system – if you enter a key vocabulary term that’s not included in our system you’ll receive a gift and your term may be added to our extensive vocabulary database.
iSirona

Booth: 6083
Contact:
Peter Witonsky, President
850.303.0575
Peter.witonsky@isirona.com
info@isirona.com
iSirona provides simplified, software-based solutions for medical device integration. By automating the flow of data from devices directly to a hospital’s clinical information system, iSirona helps improve clinician productivity as well as data accuracy and availably. Completely vendor-neutral, this proven solution integrates patient data from any medical device, regardless of manufacturer, into any CIS.
iSirona says: Are your nurses still writing patient device data on paper, only to have to key it in later? Why make them manage the data twice? Stop by our booth (#6083) to hear about how hospitals are saving 30 minutes per nurse per shift using our device integration solution.
Keane

Booth: 1548
Contact:
Larry Kaiser, Marketing Manager
lkaiser@keane.com
631.824.5318
www.keane.com/hsd
In business since 1975 and based in the United States, Keane’s Healthcare Solutions Division (HSD) offers complete IT solutions to hospitals and long-term care facilities throughout the country. Keane’s proprietary software and services help health organizations increase efficiency, reduce medical errors, meet regulatory requirements, and enhance the revenue cycle. An electronic health record (EHR) solution, the Keane OptimumTM suite of fully integrated certified clinical applications helps hospitals and healthcare facilities reduce medical errors, increase efficiency, and improve the delivery of care.
Keane Says: Your journey towards meaningful use starts when you visit the Keane booth. Find out how Keane Optimum can help you receive full reimbursement under ARRA and register to win an iPad.
maxIT Healthcare

Meetings By Request
Contact:
Mark Fangman, Executive Vice President, Sales & Operations
877.652.4099
www.maxithc.com
mark.fangman@maxithc.com
maxIT Healthcare, the largest privately held healthcare IT consulting firm, has been completely focused on Healthcare Information Technology since our founding in 2001. With over 525 consultants, maxIT is the trusted technology advisor and partner to healthcare organizations, providing seasoned professionals and expert guidance to maximize quality, safety, and financial performance. maxIT offers implementation, project management, and management consulting expertise in healthcare information systems (HIS), electronic medical record (EMR) systems, enterprise resource planning (ERP) systems, payer systems, and clinical imaging and informatics systems.
maxIT Says: The challenges and multiple priorities that healthcare information technology executives are faced with are well-documented. At maxIT, our focus is on our clients’ success and overcoming these challenges by maximizing IT outcomes. Whether you need help with Meaningful Use assessments and roadmaps, 5010 testing, ICD-10 assessments, ACO strategy, system selection, or HIS/EMR implementation, maxIT has the depth and breadth of experience you need. If you would like to discuss these critical initiatives or any other IT priorities with us at HIMSS, we would greatly appreciate the opportunity to meet with you and discuss your needs.
McKesson

Booth: 6471
Contact:
Joey Nord, Director, Communications
www.mckesson.com/mpt
Joey.Nord@mckesson.com
McKesson Corporation, currently ranked 14th on the FORTUNE 500, is a healthcare services and information technology company dedicated to helping its customers deliver high-quality healthcare by reducing costs, streamlining processes, and improving the quality and safety of patient care.
McKesson Says: McKesson is focused on helping organizations make healthcare better. Our healthcare IT experts will be available in Booth #6471 to demonstrate how our solutions empower organizations to link clinical data, streamline processes, leverage analytics and improve financial performance.
MED3OOO

Booth: 917
Contact:
Nicole Contardo, Marketing Director
919.794.5881
Nicole_Contardo@MED3000.com
www.MED3000.com
MED3OOO provides products and services that optimize clinical and financial results for healthcare providers. MED3000 solutions bring real meaning to meaningful use by delivering the tools necessary for positive outcomes. Outcomes matter and our 360 degree solution enables hospitals and physicians to operate efficiently and deliver optimal results for their patients. We provide solutions for: physician practices, community health centers, integrated physician networks, accountable care organizations, independent hospitals, health systems, labs, billing companies, employers & municipalities, and payers.
MED3OOO Says: Stop by booth #917 to experience MED3OOO’s 360 degree solution. We’re bringing a comprehensive set of solutions to Accountable Care Organizations with our Meaningful Use Certified EHR, PM, RCM, data warehouse and lab outreach products.
Special give-away just for HIStalk readers: We’ll be doing a HIStalk-readers-only drawing on Wednesday at noon for an iPad. Stop by the booth for details.
MedAptus

Meetings By Request
Contact:
Jennifer Crowley, Marketing Director
617.896.4030
www.medaptus.com
jcrowley@medaptus.com
MedAptus’ offerings include powerful and easy-to-use Intelligent Charge Capture technologies and high-impact revenue cycle consulting services. Many of the nation’s most prestigious healthcare organizations rely on MedAptus for financial optimization; additional product benefits include EMR enhancement, manual process re-engineering and substantially improved productivity.
MedAptus Says: MedAptus representatives will be attending HIMSS for networking purposes. Any organizations, particularly provider groups, EMR vendors and/or medical billing companies interested in learning more about our physician charge capture technology and financial benefit should contact us to set-up time to speak.
MEDecision
Booth: 2563
Contact:
Eric Demers, Executive Vice President, Chief Strategy Officer, Health and Life Science
610.540.0202
www.MEDecision.com
MEDecision offers collaborative health management solutions that provide a way for payers and providers to harness the power of knowledge to enable the best clinical decisions, engage patients and improve health outcomes. Designed around a patient-aware health management philosophy, MEDecision’s solutions include Alineo®, a health management platform for delivering outcome-driven case, disease, utilization and behavioral health management; InFrame™, a set of tools that facilitate the health and performance management processes for physicians and accountable care organizations; and Nexalign®, MEDecision’s health decision support service that applies analytics to information gathered from multiple sources to foster better business and clinical decisions on a patient’s behalf. For more information, visit www.MEDecision.com.
MEDecision Says: Stop by the MEDecision booth for a complimentary cup of Starbucks coffee! It’s the only Starbucks coffee available on the mile-long show floor. Sip on a hot latte and ask about our comprehensive solutions to support patient-centered medical home and accountable care organizations. We’ll be demonstrating the technology we’re developing to power these important new game-changing models.
Medicity

Booth: 6749
Contact:
Lilian Myers, SVP of Marketing
801.322.4444
marketing@medicity.com
www.medicity.com
Medicity, the industry standard for health information exchange (HIE), is the leading innovator and largest provider of HIE technology – with more than 750 hospitals, 125,000 physicians and 250,000 end users in its connected ecosystem. Medicity’s solutions empower hospitals, physicians and HIEs with secure access to and exchange of health information – improving the quality and efficiency of patient care locally, regionally and nationally.
Medicity Says: Visit us at HIMSS to see how our certified meaningful use modules run on iNexx – the first open, modular, HIE-native platform for healthcare IT applications – to enable physicians to qualify for stimulus funds. We will also be presenting how our new partnership with ActiveHealth Management enables a turnkey solution for ACO technology and management.
Medicomp Systems

Booth: 2231
Contact:
James Atia, Senior Product Manager
703.803.8080
www.medicomp.com
jaita@medicomp.com
Medicomp’s dynamic, as opposed to static template-based, EMR tools provide clinicians immediate access to the total patient picture, based on the way doctors think and work. At the heart of every product is Medicomp’s powerful MEDCIN® Engine, a robust clinical data engine in use throughout the world by a growing number of physicians and hospitals.
Medicomp Says: Come experience our newest innovation, Quippe, that enables clinicians to access and document information in the cloud. We’ll also be rolling out CliniTalk, Medicomp’s voice-enabled, easy-to-use EMR tool. Look for a big HIMSS announcement on HIStalk on Monday evening, February 21.
MediServe

Booth: 5054
Contact:
Ruth Taylor, Corporate Event & Trade Show Coordinator
480.831.7800
www.mediserve.com
medimail@mediserve.com
MediServe delivers software solutions designed to manage the unique workflows associated with providing rehabilitation care. MediServe solutions are fully integrated companions to any EMR. MediServe works with clients to improve revenue and make compliance easier in the complex environment of rehabilitation care.
MediServe Says: Come see us at booth #5054.
MedPlus, a Quest Diagnostics® Company

Meetings By Request
Contact:
Steve McDonald, President, Hospital Sales
MedPlus, a Quest Diagnostics Company
800.444.6235, ext. 2792
smcdonald@MedPlus.com
MedPlus, the healthcare information technology subsidiary of Quest Diagnostics, provides clinical connectivity for hospitals/IDNs and physician practices, helping bridge the gap between inpatient and outpatient worlds. Care360™ EHR provides physicians with a step-wise approach to EHR adoption that helps transition key activities from paper to electronic with features like electronic lab order management, clinical messaging, ePrescribing, document management and multi-system interoperability. For more information, visit www.Care360.com.
MEDSEEK

Booth: 1149
Contact:
Lori Moore
Lori.moore@medseek.com
205.982.5881 office
205.834.5263 cell
Since 1996, MEDSEEK has focused exclusively on creating a 360-degree optimal eHealth experience for patients, clinicians and administrative staff by removing traditional integration and communication barriers, workflow roadblocks and redundant processes. Used by more than 785 hospitals, MEDSEEK solutions enable hospitals to execute enterprise-wide strategic objectives by improving quality of care, uncovering new sources of revenue and generating meaningful loyalty among physicians and patients with a low-risk, high-return investment that leverages existing IT investments and infrastructure. For more information, visit www.medseek.com or call 1.888.MEDSEEK.
MEDSEEK Says: We began this journey in 1996. Now,785 hospitals later, MEDSEEK is happy to mark 15 years in eHealth. Join us for our 15th anniversary celebration Tuesday, February 22 at 5pm at booth #1149 at HIMSS in Orlando, and hear Apprentice’s Bill Rancic present “Entrepreneurship in Health Care”. Space is limited, so get details and RSVP online today.
MedVentive

Meetings By Request
Contact:
Info@medventive.com
781.290.2511
MedVentive – in the right place and now the right time. While healthcare was evolving the concept of an accountable care organization, MedVentive was busy operating as one. MedVentive was founded as the PSN in 1997 by the CareGroup Healthcare System, an integrated, at-risk network of 4,500 physicians and eight hospitals that cared for more than 450,000 at risk patients. Our origins as an ACO give MedVentive a deep understanding of provider organizations and the healthcare environment. Having been an at-risk provider network, MedVentive is uniquely qualified to support an organization’s transition from a fee-for-service payment environment to risk-based contracting, and provide the clinical integration/ population management infrastructure necessary to be successful under this new model.
MedVentive Says: Take the opportunity to schedule a one-on-one meeting – breakfast, lunch, dinner or more detailed meeting at our onsite guest suite – with our Executive team to discuss how our history can impact your future in transitioning from managing patients to patient populations (clinical integration and registries) to successfully taking on risk-based contracts.
Merge

Booth number: 3348
Contact:
Jennifer Jawor, Marketing Manager
312.565.6825
www.merge.com
jjawor@merge.com
Merge Healthcare develops software solutions that automate healthcare data and diagnostic workflow to create a more comprehensive electronic record. Our products, ranging from standards-based development toolkits to fully integrated clinical applications, have been used by providers, vendors and researchers worldwide for over 20 years. In addition, we provide Interoperability solutions that link systems together and image-enable broader health information exchange.
Merge Says: Hurdle ‘Meaningful Use’ with ease with Merge Healthcare – your partner for diagnostic content and instrument connectivity! Visit booth #3348 to discover Merge iConnect™, our new comprehensive and modular solution suite built to enable interoperable image exchange and management. We’re the guys in orange with a Tesla in our booth. Stop by, check out the car and get a photo!
Microsoft Health Solutions Group

Booth: 3101
Contact:
Nancy Narraway, Senior Industry Marketing Manager
nancyna@microsoft.com
Over the past 13 years, Microsoft has steadily increased its investments in health with a focus on addressing the challenges of health providers, health and social services organizations, payers, consumers and life sciences companies worldwide. Microsoft closely collaborates with a broad ecosystem of partners and delivers its own powerful health solutions, such as Amalga, HealthVault, and a portfolio of identity and access management technologies acquired from Sentillion Inc. in 2010. Together, Microsoft and its industry partners are working to deliver health solutions for the way people aspire to work and live.
Microsoft Says: Come learn more about Microsoft’s health solutions: Amalga™, HealthVault™, HealthVault Community Connect, Vergence™, ProVision™, ExpreSSO™ and Way2Care™ — and check out some cool tablets made by Microsoft partners. While you’re in the booth, test drive Kinect™ for Xbox 360® and try your luck at the Way2Win kiosk for a chance to win a Microsoft Arc™ Mouse.
MyHealthDIRECT

Booth: 218, Kiosk 11
Contact:
Carol Heideman, Director of Marketing
262.787.3439
www.myhealthdirect.com
cheideman@myhealthdirect.com
MyHealthDIRECT “connects people to providers” through its web-based service solution. We offer the missing gateway, which enables hospitals/health systems, managed care organizations, HIE and state Medicaid agencies to link patients to the right health professionals offering the right health care services at the right time and location.
MyHealthDIRECT Says: Come see and learn first-hand through a live demo of MyHealthDIRECT on how our SaaS-enabled application links supply-to-demand in the referral and scheduling process by connecting patients to provider appointments in real-time; taking only 1-3 minutes. MyHealthDIRECT analytics and reporting can clearly quantify the outcomes—as well as the real-dollar-results of more efficient care delivery, and access to timely care. Come hear Jay Mason, CEO and president of MyHealthDIRECT speak during HIMSS at the New & Emerging Technology Pavilion (Booth #218), Monday, February 21st (1:30 pm – 2:15 pm). Marilee Benson, VP Community Alliances will also be speaking on Monday (3:30 pm – 4:15 pm).
NCR
![NCR-logo_Pantone[2] NCR-logo_Pantone[2]](http://histalk2.com/wp-content/uploads/2011/02/NCRlogo_Pantone2_thumb.jpg)
Booth: 2805
Contact:
Jim Dowling, VP of Sales
Jim.dowling@ncr.com
As the #1 provider of patient self-service, NCR can help you manage the anticipated 32+ million new patients entering the healthcare system as a result of Healthcare Reform. Our proven online, mobile and kiosk-based solutions automate routine transactions, allowing patients to pre-register, schedule appointments and pay bills how and when it is most convenient. We have the consulting, industry and consumer expertise to help you improve the patient experience, optimize revenue cycle and streamline workflow.
NCR Healthcare Says: Visit us at Booth 2805 to see the latest, most innovative and widely deployed patient self-service solutions. Free copy of "Paper Kills 2.0: How Health IT Can Help Save Your Life and Your Money", signed by Newt Gingrich, founder of the Center for Health Transformation, to the first 25 people who schedule a booth appointment.
NextGen Healthcare

Booth: 2163
Contact:
NextGen Healthcare
www.nextgen.com
215.657.7010
Sales@NextGen.com
NextGen Healthcare drives patient-centered, accountable care across the continuum. Ambulatory and inpatient providers of all sizes are leveraging our integrated clinical, financial and connectivity solutions, along with our quality management and consulting services, to improve care coordination within their communities and drive business growth. NextGen Healthcare is proud to share that its product suite was one of the first to be Meaningful Use certified for both eligible professionals and hospitals.
NextGen Healthcare Says: In our booth this year, HIMSS11 attendees will see the vision of collaborative, higher quality care come alive before their eyes, as incredible splash artists embody the characteristics that make world-class products, services, and partnerships on canvas. Don’t miss the chance to see them in action, and then win one of their amazing creations, a new smart phone or an iPad! Also stop by to check out the NextGen Patient Portal, test NextGen Mobile on an iPad, and catch the unveiling of our revolutionary new data capture device.
Nuance

Booth: 2744
Contact:
Mark Erwich, Senior Director Marketing
781.565.5070
www.nuance.com/healthcare
mark.erwich@nuance.com
Nuance will be exhibiting our full suite of speech-driven clinical documentation and communications solutions including eScription, which will be receiving its 7th consecutive Best-in-KLAS Award at HIMSS this year (an accomplishment of very few HIT software products!) At the booth, also visit our Physician Station, to see hands-on best practices demos of Dragon Medical in the EHR; a Clinical Language Understanding (CLU) Station where we will highlight new technologies for extracting structured data from free-form text, and our VERY COOL Mobility Station where we are previewing a bunch of clinical documentation apps for the iPhone and other devices!
Nuance Says: Stop by our booth too see how Nuance Healthcare is building on its leadership in speech-driven clinical documentation, communication and decision-support systems to capture and transform clinical data into actionable patient information.
Orion Health

Booth: 5146
Contact:
Michael Burke, VP of Sales
310.526.4030
www.orionhealth.com
Orion Health is the leading Health Information Exchange solution provider with over 15 years of experience in clinical workflow and integration technology for the healthcare sector. Orion Health’s easy to use solutions and applications improve patient care and clinical decision making by enabling the exchange of healthcare information among disparate systems and providing integrated health data in a single, unified view. Our HIE solution also meet the ‘meaningful use’ requirements and the goals of Accountable Care Organizations to improve care coordination, cut cost and provide better quality of care.
Orion Health Says: Come visit the Orion Health booth at HIMSS and hear what other CIOs and IT professionals have to say about using the Orion Health HIE solution including outcomes of a successful statewide implementation, achieving better collaboration between regional physicians in a competitive market, and ROI from an effective regional disease management program. Register for free today.
PatientKeeper

Booths: IO showcase Hall E, booth #7343, Exhibitor booth #5543
Contact:
Kathy Ruggiero, director of corporate marketing
www.patientkeeper.com
kruggiero@patientkeeper.com
781.373.6433
PatientKeeper® Inc., the leading provider of physician healthcare information systems, enables physicians and hospitals to focus on their patients, not technology, by providing highly intuitive software that streamlines physician workflow to improve productivity and patient care.
PatientKeeper Says: Stop by our booth or visit us at the Interoperability Showcase to learn how PatientKeeper offers customers an alternative path to Meaningful Use to meet the stimulus requirements outlined in the HITECH Act. See how we’ve designed our CPOE and Physician Documentation software to increase the probability of physician adoption; our new handheld platform to support all the latest mobile devices for many of our applications (Charge Capture, Mobile Clinical Results, etc.); and our HIE solutions to create a longitudinal view of patient health status across a community.
Perceptive Software

Booth: 5163
Contact:
Adam Meloan, Marketing Program Manager – Healthcare
800.941.7460
adam.meloan@perceptivesoftware.com
www.perceptivesoftware.com/healthcare
Perceptive Software creates enterprise content management (ECM) technology that integrates easily with your EMR, EHR and HIS applications to complete the patient record and connect staff with the information they need. With ImageNow document management, imaging and workflow, you can capture, process and collaborate on important documents, protect data integrity throughout its lifecycle and access precise content in the context of your everyday processes.
Perceptive Software Says: Accessing the content you need isn’t brain surgery. Visit us at Booth #5163 and see how ImageNow easily puts patient information and content into the context of your facility’s daily processes. While you’re there, register to win one of three Apple iPad mobile digital devices. Plus, on Tuesday, Feb. 22, we’ll be serving fresh-baked cookies and gourmet coffee starting at 9:30 a.m.
Picis

Booth: 1163
Contact:
Mark Blazejewski, Sales Operations Manager
781.557.2271
Mark_Blazejewski@picis.com
www.picis.com
Picis, an Ingenix company, is a global provider of innovative solutions that enable rapid and sustained delivery of clinical documentation, financial and operational results in the emergency departments, surgical suites and intensive care units of more than 2,200 hospitals in 19 countries.
Picis Says: Learn how Picis takes the guesswork out of meaningful use. Stop by our booth to hear how hospital executives are using our solutions to support HIEs, meet CPOE requirements, ease quality reporting and optimize continuity of care.
Quality IT Partners

Meetings By Request
Bruce A. Werner, Director of Business Development
828.635.6525
828.234.0075
bwerner@qitp.com
www.qitp.com
Quality IT Partners (Quality) is a premier national healthcare consulting firm with an unparalleled reputation of taking good care of their clients and employees. We provide implementation and support services for healthcare applications such as Epic, Cerner, QuadraMed, Siemens, Eclipsys and McKesson. Quality also specializes in Meaningful Use, ICD-10, Revenue Cycle Management, Business Continuity & Disaster Recovery Planning, and New Construction IT Infrastructure Planning & Management.
Quality IT Partners Says: Quality is interested in meeting with clients and prospects as well as professionals who may be interested in joining our firm while at HIMSS. Please contact (Bruce Werner, Director of Business Development, Office: (828) 635-6525, Mobile: (828) 234-0075, or e-mail: bwerner@qitp.com) to schedule a time.
:RATIO, a division of Software Testing Solutions

Booth: 2975
Contact:
Brent Christensen, VP
877.765.0100 ext. 408
bchristensen@ratio.us.com,
www.ratio.us.com
Software Testing Solutions has been the leading provider of true technology-based quality assurance solutions to Primary Acute Care organizations for over a decade. Our dedicated staff of Healthcare and IT professionals leverage over 70 years of experience to deliver state-of-the-art automated testing solutions to hospitals of all sizes throughout North America. Our focus on setting the highest possible standards of testing in the lab, the blood bank, and across a wide spectrum of CPOE offerings brings the flexibility of a customized solution with the ease of use of a turnkey implementation, bridging the gap of patient safety by eliminating the risk of untested applications.
Ratio Says: Learn new ways to make your CPOE application more robust, insure higher levels of quality care, and meet critical standards of “meaningful use” more efficiently and with greater speed. Stop by to discuss options with the experts in the automated testing at booth 2975.
RelayHealth

Booth: 1663
Contact:
Lynette Cortez, Solutions Advisor, RelayHealth
888.743.8735
rhinfo@relayhealth.com
www.RelayHealth.com
RelayHealth enables information exchange for all those involved in healthcare – including providers, patients, payers, pharmacies, financial institutions and pharmaceutical manufacturers – to simplify clinical and financial interactions. RelayHealth’s SaaS solutions accelerate quality of care, financial health and workflow efficiencies. The RelayHealth network provides connectivity services to approximately 1,800 payers, 2,000 hospitals, 200,000 physicians, 1.35 million patients and thousands of retail pharmacies across the nation.
RelayHealth Says: RelayHealth’s clinical integration capabilities offer a low-cost, scalable and highly networked SaaS solution that doesn’t require a costly infrastructure and is sustainable. RelayHealth creates a way for hospitals and physicians to facilitate care coordination and take advantage of federal ARRA incentives. Visit RelayHealth at Booth #1663/Hall B and experience Health Connections Brought to Life.
Renaissance Resource Associates
Meeting By Request
Contact:
Maria McBride, Managing Director
206.949.6011
maria@rraconsulting.com
Laura Noble, CEO
425.241.9210
laura@rraconsulting.com
Renaissance offers over 20 years experience in meeting the challenges of HIT in an ever changing and evolving industry. We get it right the first time, saving IDNs time and money, and delivering optimized use of technology in a clinical care environment. Meaningful Use, ICD-10, Clinical Informatics, Strategic Planning, Process Redesign, Implementation, Upgrade, Maintenance.
Renaissance Resource Associates Says: We make sure you implement your vendor’s software in a way that will achieve the meaningful use criteria. Buying a certified product will not get you there – we will take you from product to your first payment. We can get you to ICD10 – mapping, transition, even certified coders until you get up and running!
Sage Healthcare

Booth: 1713
Contact:
Tony Ryzinski, senior vice president of marketing, Sage Healthcare Division
813.202.5511
www.sagehealth.com
tony.ryzinski@sage.com.
At Sage, our philosophy is simple: We are physician-focused and patient-centric, providing clinical and financial technology solutions for the ambulatory market, serving more than 400,000 healthcare professionals including approximately 80,000 physicians in small, medium and large practices and Community Health Centers. Our products are designed by clinical and technical specialists who focus their skills on developing solutions for key medical specialty areas including primary care, OB/GYN, Pediatrics, Cardiology and Orthopedics. Sage’s certified connected solutions meet the end-to-end technology needs of physician practices from portal to integrated Practice Management and EHR to Revenue Cycle Management and Practice Analytics.
Sage Says: Experience the Sage difference: We are physician-focused, patient-centric. Sage has teamed with the Larry King Cardiac Foundation to highlight the importance of prevention and early detection of heart disease, the leading cause of death in the US. At Sage, we’re putting the “care” back in healthcare technology by providing practices with the technology they need to enable them to take better care of their patients and achieve better outcomes. As such, feel free to come by and sign our Red by Sage Wall of Inspiration to commemorate those you know and love whose lives have been touched by heart disease. Or, just stop by and get some heart health information, and enjoy a complimentary stress reducing chair message.
Salar

Booth: 1141
Contact:
Greg D. Wilson, RVP Sales
860.294.9877
gwilson@salarinc.com
www.salarinc.com
Salar delivers the healthcare industry’s most flexible and physician-centric inpatient documentation and billing solutions. With Salar, physicians and hospitals alike achieve notable productivity, financial and patient safety improvements. Physicians are free to document the way they want, using customized electronic forms that save time and improve collections by automatically transforming physician notes into billing and clinical data. By integrating with existing health information systems, Salar helps hospitals capture and share this data in real time to achieve a higher-quality, more complete EMR.
Salar Says: If you’re struggling to migrate physicians to an electronic clinical documentation platform, or seeking a better solution than traditional dictation systems and paper processes, let Salar show you a better way. Actually, let our customers show you. Visit us a booth 1141 and talk directly with several CIOs, CMIOs, and physician champions who have increased physician satisfaction and adoption of the EMR using Salar’s intuitive documentation and charge capture solutions.
Sentry Data Systems

Booth: 1737
Contact:
John Peebles, CIO
john@sentryds.com
Samantha Stevens, Administration Manager
sstevens@sentryds.com
800.411.4566 xt. 2403
www.sentryds.com
Sentry Data Systems offers healthcare business intelligence technology solutions that address a variety of operational, workflow, compliance, and financial challenges found within hospitals and pharmacies. Built upon Datanex™, a healthcare cloud computing platform, they include the pharmacy management product Sentinel RCM™ (Revenue Cycle Manager), pharmacy transaction processing platform Sentrex™, and the healthcare business intelligence platform HealthBIT® (Business Intelligence Technology).
Sentry Data Systems Says: Stop by to learn how healthcare cloud computing can save you time and money while giving you access to incredible processing power. Watch us securely deploy a server for you in less than a minute. Access your data with a powerful query engine. Use application programming interfaces (APIs) to build applications or run advanced analytics on your existing data. See how you can put hundreds of servers to work running queries on massive data sets without the headache of a large scale data center build-out.
Shareable Ink

Booth: 623
Contact:
Suzanne Cogan, Vice President, Sales & Marketing
877.572.7423 x802
www.shareableink.com
scogan@shareableink.com
Shareable Ink is the natural approach to electronic health records that complements an organization’s existing IT systems and strategies. Enabling electronic capture of information with no change in workflow, Shareable Ink allows data to be routed to specific modules within an EHR, as if typed with a keyboard. Built-in analytics give hospitals and practices insight into their operations – from a clinical, quality, and efficiency standpoint –previously inaccessible from paper records.
Shareable Ink Says: Visit Shareable Ink at Booth #623 to learn how to achieve 100% physician adoption of electronic documentation without changing workflow or hampering productivity.
SRSsoft

Booth: 349
Contact:
Evan Steele, CEO
www.srssoft.com
esteele@srssoft.com
SRS is the leading provider of productivity-enhancing EHR technology and services for high-performance specialty practices—with a successful adoption rate unparalleled in the industry. Offered via the Unified DesktopTM, the robust EHR, SRS CareTracker PM, and SRS PACS increase speed, free physicians’ time, boost revenue, and heighten patient care and satisfaction.
SRS Says: SRS is all about productivity for high-performance physicians—specialists, in particular. Stop by the SRS booth to see how SRS has cracked the code to productivity-focused meaningful use.
Stimulus Search

Meetings By Request
Contact:
Dan Moriarty, Chief Sales Officer
504.875.5172
www.stimulussearchllc.com
dan@stimulussearchllc.com
Stimulus Search LLC is a national search firm that helps Healthcare Software & Services companies achieve optimum results by attracting, qualifying and delivering high-performing sales and support talent.
Stimulus Search Says: Please contact Dan prior to the show to set a time to meet on Wednesday.
Stockell Healthcare

Meetings By Request
Contact:
Rich Lewis, Vice President of Sales
800.786.2535, ext. 186 (Office)
314.616.2459 (Cell)
richl@stockell.com
Stockell Healthcare Systems features InsightCS®; our proven Electronic Financial Record (EFR) solution that effectively coexists and interoperates directly with the leading Clinical/EMR systems, and provides end-to-end Patient Access, Patient Accounting, and Revenue Cycle Management solutions to Hospitals, Behavioral Healthcare Providers, Rehabilitation Facilities, and Integrated Health Networks. With InsightCS®, you get the tools you need to more effectively manage costs via a patient-centric, workflow-driven approach which delegates the right work to the right person at the right time and place.
Stockell Healthcare Says: InsightCS® is the ONLY proven EFR solution that dynamically captures, edits, and manages encounter-based patient care delivery data by converting it into actionable enterprise information. We invite you to speak with us to learn more about the many benefits of InsightCS® and how it has been successfully deployed with a wide variety of EMR/CPOE systems at hospitals, mental health facilities, and rehabilitation centers across the United States.
Sunquest Information Systems

Booth: 6171
Contact:
Chris Fraker, Manager, Marketing Communications
520.570.2302
chris.fraker@sunquestinfo.com
www.sunquestinfo.com
Sunquest Information Systems, Inc. delivers market-leading diagnostic information technology and outreach solutions designed and implemented to fulfill the business objectives of today’s healthcare leaders. Sunquest’s vision is encompassed by a commitment to patient safety, workflow excellence, predictive medicine, and physician & patient affinity. Sunquest serves the global marketplace with reliable laboratory technology required for mission critical applications. Transforming the delivery of healthcare, Sunquest continues to strive for strategic growth through expansion, operational excellence, technological innovation, and industry-leading thought leadership.
Sunquest Says: Solutions from Sunquest are transforming the lab like never before. At our booth, you will find outreach solutions, like Sunquest Outreach Advantage® and Sunquest Physician Portal™, that expand diagnostic services into the community. You will also see how Sunquest Diagnostic Intelligence™ provides laboratories with critical information in real time so they can make data-driven decisions based on meaningful metrics.
Surgical Information Systems
Booth: 5963
Contact:
Kermit Randa, SVP, Sales and Marketing
678.507.1650
www.SISFirst.com
Randa@SISFirst.com
Surgical Information Systems (SIS) offers perioperative information management solutions designed to increase the safety, efficiency and profitability of healthcare providers. As the only healthcare IT company focused exclusively on the complex surgical environment, SIS provides adaptable single-database solutions that integrate easily with other hospital systems.
SIS Says: Stop by booth # 5963 to learn how the SIS solution, a certified modular EHR, fits into your EMR strategy.
Thomson Reuters

Booth: 5263
Contact:
clinicalxpert@thomsonreuters.com
www.healthcare.thomsonreuters.com/HIMSS2011
The Healthcare & Science business of Thomson Reuters provides intelligent information for healthcare payers and providers to better manage the cost and quality of healthcare. Our clinical decision support solutions use real-time clinical surveillance and integrated Micromedex® content to help clinicians improve outcomes and reduce costs by making more informed treatment decisions at the point of care. Our payer solutions help employers and health plans manage healthcare costs, maintain regulatory compliance and identify fraud, waste, and abuse. With our management decision support capabilities hospital administrators have the benchmarking tools they need to improve clinical, operational and financial performance.
Thomson Reuters Says: Hospital CIOs and IT managers. Clinicians. Administrators. Payers – Thomson Reuters has the intelligent information you need to improve the cost and quality of healthcare. Stop by booth 5263 to learn more about our clinical intelligence dashboards, our integrated content solutions or our HIE offering. You can also register to win a Logitech Revue.
T-System

Booth: 3323
Contact:
Corinne Tso, Director of Marketing
214.673.4696
www.tsystem.com
ctso@tsystem.com
T-System, Inc. sets the industry standard for clinical, business and IT solutions for emergency departments, with approximately 40% of the nation’s emergency departments using T-System’s products. To meet the individual needs of hospitals, T-System offers both a paper template and an emergency department information system (EDIS). These tools help clinicians quickly see information so they can provide better patient care, while improving efficiency and the bottom line.
T-System Says: Welcome to HIMSS11! We are excited to be demonstrating the capabilities of our EDIS at the Interoperability Showcase. Our T SystemEV® was one of the first ED solutions to be certified for Stage 1 Meaningful Use. To learn more about our presentation and industry-leading ED solutions, please visit us at booth #3323.
Virtelligence

Booth: 2131
Contact:
Akhtar Chaudhri, President and CEO
952.548.6601
www.virtelligence.com
akhtar@virtelligence.com
Virtelligence is a privately held premier healthcare IT consulting firm that offers solution advisory and healthcare IT consulting services to payor and provider organizations throughout the U.S. Our comprehensive range of services includes system implementation, optimization, reporting, technology integration, and training in the Cerner, Epic, Eclipsys, McKesson, MEDITECH and Siemens. Virtelligence earned recognition as a Top 500 Small Business in America by Diversity Business.com, “Great Places to Work” by Minneapolis-St. Paul Business Journal, Top 100 Healthcare IT Companies (HCI-100) by Healthcare Informatics Magazine and as one the fastest-growing private companies in America for Inc5000 by Inc. Magazine.
Virtelligence Says: Choose the most cost-effective alternative in Healthcare IT. Since 1998, Virtelligence has partnered with clients in a proven record of success. Our efficient operating model allows us to deliver top-quality results at a very competitive price. Our customer loyalty far exceeds industry standards. Virtelligence pairs a solid knowledge of HIT products with true client commitment. Enjoy the benefits that come from access to the best resources available. We keep a national focus but a local commitment.
Special give-away just for HIStalk readers: Virtelligence will give away an iPad during the HIMSS Orlando conference. Stop by booth #2131, mention you are a HIStalk reader, and drop off your business card.
Vitalize Consulting Solutions

Booth: 3070
Contact:
Cyndi Cahill, Senior Vice President
610.444.1233 Ext. 4103
www.getvitalized.com
ccahill@getvitalized.com
Vitalize Consulting Solutions, Inc. (VCS) draws on the keen insight and proven methodology from its considerable HIT experience to help you fulfill organizational objectives. Our team of healthcare professionals joins your team and provides documented, high quality solutions for each engagement primarily based in Allscriptsä, Cerner, Epic, McKesson, MEDITECH, and Siemens solutions, as well as in the Ambulatory and Project Management practices. We offer the full breadth of consulting services from strategic services, operational improvement, and revenue cycle optimization projects to implementation, staff augmentation, project management, and training and go-live support. Together, through this blend of professional services and packaged solutions, we seek to forge positive outcomes that satisfy clinical, financial, and informational goals, all for a predictable cost.
VCS Says: Stop by booth #3070 at HIMSS ‘11 and help us giveback to the people of central Florida. In an effort to eliminate the need for individuals to choose between paying for healthcare and feeding their family, VCS will donate $5 to Orlando’s Second Harvest Food Bank for every “link” supplied to our Chain of Hope. You can pick up a link at the booth and attach it. Please help us help Second Harvest “fight hunger and feed hope.”
Special give-away just for HIStalk readers: For each HIStalk reader who stops by our booth and connects a link, we will double the $5 Second Harvest Food Bank donation to $10.
Voalte

Booths:
Philips: 3845
Rauland-Borg: 3031
Meru: 2979
Contact:
Trey Lauderdale, VP of Innovation
941.312.2830
trey@voalte.com
Voalté provides compelling software solutions for healthcare institutions that solve communication problems at the point-of-care. We believe that better, more efficient communication improves clinical performance, which in turn improves patient care, safety and satisfaction. Our products are designed to be intuitive, high value, mission critical applications running on the latest generation of touch-based smartphones. We provide an exceptional end-to-end user experience. We do it better than anyone else, and we spend our time thinking about ways to improve this experience.
Vocera Communications, Inc.

Booth: 4450
Contact:
salesweb@vocera.com
408.882.5600
www.vocera.com
Vocera Communications, Inc. is the leading provider of communication systems designed to restore the human connection to healthcare. By providing integrated communication solutions for voice, alarm and alert, and text systems, Vocera allows care teams, patients, and loved ones to exchange critical information at the point of care.
Vocera Says: Visit the Vocera booth to learn how hospitals across the country are elevating patient care with a variety of Vocera products. Stop by to hear about new solutions that deliver pages, text messages, and alerts directly to smartphones including iPhone, BlackBerry, and Android devices.
Wellsoft Corporation

Booth: 2230
Contact:
Denise Helfand, VP, Sales & Marketing
800.597.9909
www.wellsoft.com
dhelfand@wellsoft.com
Wellsoft, developer of the industry-leading Wellsoft EDIS (since 1988), is an ONC-ATCB 2011/2012 Certified EHR Module*; is CCHIT® Certified and is consistently ranked the #1 EDIS by KLAS and MD Buyline. Wellsoft EDIS is recognized for providing the most complete functionality, and the most scalable and configurable product in the marketplace. Features offered include patient tracking, clinical documentation, CPOE, Charge Capture, Clinical Decision Support, workflow consulting and more. Wellsoft works with you to analyze patient flow and determine how to support best practices. Wellsoft is EDIS at its Best.
Wellsoft Says: We welcome the opportunity to discuss how Wellsoft can partner with your hospital to achieve Meaningful Use. We invite you to see our newest features and to see why Wellsoft is ED clinicians’ favorite EDIS. Easy to learn and easy to use, Wellsoft is EDIS at its Best.
Wolters Kluwer Health

Booth: 6162
Contact:
Laura Gilbert, Sr. Director, Marketing Communications
612.313.1506
Laura.Gilbert@provationmedical.com
www.pointofcareapplications.com
Wolters Kluwer Health Clinical Solutions delivers intuitive clinical decision support tools designed by and for clinicians to advance the practice of evidence-based medicine and maximize outcomes from EMR/EHR, CPOE and other clinical information systems. These include ProVation® Order Sets, powered by UpToDate® Decision Support, an easily customizable order set authoring and management solution that streamlines the delivery of standardized care and integrates easily into any facility or vendor EMR/CPOE system; Medi-Span® Clinical, a robust CDS platform that delivers CCHIT-compliant medication-related clinical decision support; and UpToDate®, the resource of choice for more than 400,000 clinicians worldwide covering more than 8,300 topics in 17 medical specialties. Other offerings include its flagship drug reference, Facts & Comparisons®; pharmacy’s #1 Software-as-a-Service (SaaS) provider, Pharmacy OneSource; and procedure documentation and coding solutions from ProVation® Medical.
Wolters Kluwer Says: An opportunity to test drive some of the industry’s leading clinical decision support tools, including ProVation Order Sets, Medi-Span Clinical and UpToDate, isn’t the only reason to swing by the Wolters Kluwer Health booth (#6162). You’ll also have the opportunity to register to win a trip for four to the U.S. Masters in Augusta!
Comments Off on Mr. HIStalk’s Must See Vendors for HIMSS11



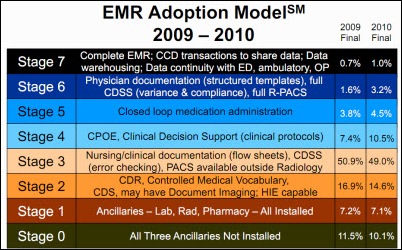

























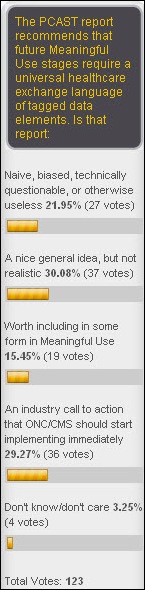






















































![NCR-logo_Pantone[2] NCR-logo_Pantone[2]](http://histalk2.com/wp-content/uploads/2011/02/NCRlogo_Pantone2_thumb.jpg)
























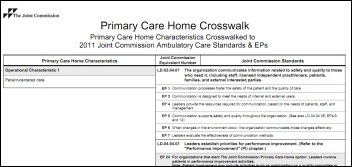






























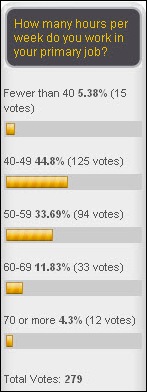







Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…