News 1/13/12
Adventist Health expands its affiliation with Cerner, announcing plans to implement Cerner Ambulatory EHR across its 130 clinics.
Reader Comments
![]() From Booth Babe: “Re: HIMSS and HIStalkapalooza. Have mercy on the aching feet of worn out tradeshow floor ‘workers’ who have only minutes to spare getting from work to FUN. Do you know how often during aching feet moments we think of the upcoming party and how it drives us through each additional hour until we can cut loose and have some fun?! I would never have time to deck out as some of those fashionistas did last year, though they looked fabulous and were fun to see. Maybe you should add a category for best ‘survivor’ shoes for tradeshow performance. ” Gee, the term “survivor” shoes is right up there with the “straight from the exhibit hall” style company logo shirts. That being said, I have a couple pair of great shoes similar to the ones above that are comfy enough for the trade shoe floor, yet stylish enough for a quick transition to Vegas nightlife. E-mail me if you want details on the brand.
From Booth Babe: “Re: HIMSS and HIStalkapalooza. Have mercy on the aching feet of worn out tradeshow floor ‘workers’ who have only minutes to spare getting from work to FUN. Do you know how often during aching feet moments we think of the upcoming party and how it drives us through each additional hour until we can cut loose and have some fun?! I would never have time to deck out as some of those fashionistas did last year, though they looked fabulous and were fun to see. Maybe you should add a category for best ‘survivor’ shoes for tradeshow performance. ” Gee, the term “survivor” shoes is right up there with the “straight from the exhibit hall” style company logo shirts. That being said, I have a couple pair of great shoes similar to the ones above that are comfy enough for the trade shoe floor, yet stylish enough for a quick transition to Vegas nightlife. E-mail me if you want details on the brand.
From ThickAndThin: “Re: McKesson. To acquire European firm MACH4 Pharma Systems?” Unverified. The England-based company sells drug packaging and preparation automation for hospital pharmacies.
![]() From DeepThrowIT: “Re: White House CTO Aneesh Chopra. Word on the street is that he will announce in the next few weeks that he will be leaving his job. No word on where he’s going next.” He’s a young guy (39) with a lot of enthusiasm and charisma, so if the rumor is true, we’ll see whether he pursues money (running a private company) or power followed by money (running for office.)
From DeepThrowIT: “Re: White House CTO Aneesh Chopra. Word on the street is that he will announce in the next few weeks that he will be leaving his job. No word on where he’s going next.” He’s a young guy (39) with a lot of enthusiasm and charisma, so if the rumor is true, we’ll see whether he pursues money (running a private company) or power followed by money (running for office.)
![]() From LeftCoaster: “Re: EDI 5010. Oregon and Washington hospitals are experiencing significant issues with transmission and receipt after mandated January 1 use, but deferred enforcement until April 1. Clearinghouse vendor [vendor name omitted] is a huge problem – they are not responding to support calls and hospitals are considering switching. Both Cigna and Providence Health Plan claim they are unable to transmit payments and organizations are having major cash flow problems, particularly community hospitals. Anyone else having problems?” Unverified, so I removed the vendor’s name. Further reports are welcome.
From LeftCoaster: “Re: EDI 5010. Oregon and Washington hospitals are experiencing significant issues with transmission and receipt after mandated January 1 use, but deferred enforcement until April 1. Clearinghouse vendor [vendor name omitted] is a huge problem – they are not responding to support calls and hospitals are considering switching. Both Cigna and Providence Health Plan claim they are unable to transmit payments and organizations are having major cash flow problems, particularly community hospitals. Anyone else having problems?” Unverified, so I removed the vendor’s name. Further reports are welcome.
![]() From Nasty Parts: “Re: [vendor name omitted]. Is moving away from their legacy EHR product and all efforts will be put behind a SaaS product they bought last year. 400+ people will be RIF’d as a result in the near future.” I removed the vendor name while we try to get confirmation (which I don’t expect to be successful), but Nasty Parts has been accurate about this company in the past.
From Nasty Parts: “Re: [vendor name omitted]. Is moving away from their legacy EHR product and all efforts will be put behind a SaaS product they bought last year. 400+ people will be RIF’d as a result in the near future.” I removed the vendor name while we try to get confirmation (which I don’t expect to be successful), but Nasty Parts has been accurate about this company in the past.
HIStalk Announcements and Requests
![]() Highlights from HIStalk Practice this week include: Dr. Gregg explains why he is skipping the HIMSS soup line this year. Hospitals now employ 20% of physicians. CareCloud grows rapidly. A breakdown of EP attestations by EMR product. Age affects physicians’ perceptions of HIT. A little bit of ambulatory HIT news is like a ray of sunshine of a cloudy day. In other words, by signing up for e-mail updates on HIStalk Practice, you can keep the winter doldrums at bay. Thanks for reading.
Highlights from HIStalk Practice this week include: Dr. Gregg explains why he is skipping the HIMSS soup line this year. Hospitals now employ 20% of physicians. CareCloud grows rapidly. A breakdown of EP attestations by EMR product. Age affects physicians’ perceptions of HIT. A little bit of ambulatory HIT news is like a ray of sunshine of a cloudy day. In other words, by signing up for e-mail updates on HIStalk Practice, you can keep the winter doldrums at bay. Thanks for reading.
![]() Welcome to Humedica, sponsoring both HIStalk and HIStalk Practice at the Platinum level. The Boston informatics company offers SaaS-based clinical business intelligence solutions that create a real-time longitudinal patient care view, giving providers insight into their patient populations, the outcomes of the treatments and procedures, and how those factors impact quality, outcomes, and cost. For physician practices, the company’s MinedShare Ambulatory product supports clinical, operational, and financial benchmarking. Humedica partners with Anceta, the informatics subsidiary of AMGA, to allow its members to collaborate on quality improvement and to share best practices. I interviewed President and CEO Michael Weintraub last month, where he talked about the company’s top-rated performance in KLAS, its partnership with Allscripts, the $50 million in capital investment the company has received, and what’s next for the industry after EMRs. Thanks to Humedica for their support of HIStalk and HIStalk Practice.
Welcome to Humedica, sponsoring both HIStalk and HIStalk Practice at the Platinum level. The Boston informatics company offers SaaS-based clinical business intelligence solutions that create a real-time longitudinal patient care view, giving providers insight into their patient populations, the outcomes of the treatments and procedures, and how those factors impact quality, outcomes, and cost. For physician practices, the company’s MinedShare Ambulatory product supports clinical, operational, and financial benchmarking. Humedica partners with Anceta, the informatics subsidiary of AMGA, to allow its members to collaborate on quality improvement and to share best practices. I interviewed President and CEO Michael Weintraub last month, where he talked about the company’s top-rated performance in KLAS, its partnership with Allscripts, the $50 million in capital investment the company has received, and what’s next for the industry after EMRs. Thanks to Humedica for their support of HIStalk and HIStalk Practice.
![]() Speaking of Humedica, the company announces a predictive analytics tool that analyzes EMR data (not claims information) to identify high-risk CHF patients and intervene before they require hospitalization. Preventable heart failure admissions cost up to $35 billion per year, with 40% of Medicare CHF patients readmitted within 90 days. MinedShare client Community Physician Network (IN) says the tool will help it perform in an Accountable Care Organization model by avoiding unnecessary admissions and providing better patient outcomes.
Speaking of Humedica, the company announces a predictive analytics tool that analyzes EMR data (not claims information) to identify high-risk CHF patients and intervene before they require hospitalization. Preventable heart failure admissions cost up to $35 billion per year, with 40% of Medicare CHF patients readmitted within 90 days. MinedShare client Community Physician Network (IN) says the tool will help it perform in an Accountable Care Organization model by avoiding unnecessary admissions and providing better patient outcomes.
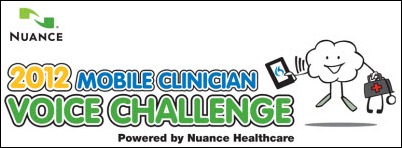
![]() Reminder: you app and Web developers still have plenty of time to enter Nuance’s 2012 Mobile Clinician Voice Challenge, considering that it takes only a couple of lines of application code to speech-enable your mobile or Web app for clinicians and the deadline isn’t until February 3. Prizes and fame could be yours. Even non-programmers can get a shot at the prize kitty by tweeting about the contest.
Reminder: you app and Web developers still have plenty of time to enter Nuance’s 2012 Mobile Clinician Voice Challenge, considering that it takes only a couple of lines of application code to speech-enable your mobile or Web app for clinicians and the deadline isn’t until February 3. Prizes and fame could be yours. Even non-programmers can get a shot at the prize kitty by tweeting about the contest.
Acquisitions, Funding, Business, and Stock
T-System acquires Practice Management Associates, a provider of coding and billing services for EDs.
TriZetto Group, which last week acquired Medical Data Express, acquires Kocsis Consulting Group.
Practice Fusion raises an additional $2 million in funding, raising its total to $38 million from Band of Angels, Felicis Ventures, and other investors.
Columbia University signs an exclusive agreement with Health Fidelity to commercialize its MedLEE text-based natural language processing technology. Fidelity offers its own NLP solution called Fidelity Platform, which uses MedLEE to extract medical data from unstructured text and generate SNOMED codes from it.
In Europe, CompuGroup Medical acquires Netherlands-based ambulatory and pharmacy systems vendor Microbais Werkmaatschappij BV. The transaction also gives CompuGroup a 51% stake in healthcare connectivity startup MediPharma Online.
Sales
Barnabas Health (NJ) adds MedeAnalytics’ Revenue Cycle Intelligence solution to compliment its existing Patient Access Intelligence solution.
El Paso Children’s Hospital (TX), which opens next month, selects RCM provider Cymetrix for business office technology and services.
The DoD awards GE Healthcare a three-year, $43 million extension of its contract for patient monitoring systems.
Illinois Neurological Institute selects JEMS Technology to provide tele-stroke evaluation.
Massachusetts Eye and Ear selects PatientKeeper Charge Capture and PatientKeeper P4P for its 250 clinicians.
Catholic Health East signs a five-year, $40 million contract to implement AUXILIO’s managed print services in its 19 hospitals.
People
Former Google Health exec Missy Krasner joins Morgenthaler Ventures as executive in residence. She was also previously senior communications director at ONC under David Brailer.
Medical appointment booking site ZocDoc adds former Senators Tom Daschle and Bill Frist to its advisory board.
Encore Health Resources promotes Thomas J. Niehaus from EVP of client services to president and COO. Dana Sellers remains as CEO. In case you missed it, Mr. H recently interviewed Joe Boyd, Encore’s chairman of the board.
Lisa Conley, formerly with McKesson, joins Sunquest Information Systems as VP of North American sales and global marketing.
Industry long-timer Kerry de Vallette joins OPTIMA Credentialing as EVP of sales and marketing.
Interactive patient care systems vendor Skylight Healthcare Systems names Scott Johnson as VP of sales. He was previously with A-Life Medical and Philips.
Announcements and Implementations
North Hawaii Community Hospital begins implementation of its HIE, which uses Wellogic’s technical platform
Intelligent Medical Objects announces the successful integration of 2012 ICD-10-CM within its newly released IMO Problem IT 2012 Regulatory 1.3 software.
Nuance Communications expands the availability of Dragon Medical to French-speaking Canadian providers with the delivery of Dragon Medical 11 French.
![]() Yale New Haven Hospital SVP/CIO Daniel Barchi provides an update on its Epic project. Six practices of 27 physicians are live, with e-prescribing at 91% and 80% of encounters closed the same day. Physician productivity for those docs is nearly back to pre-Epic levels. Greenwich Hospital will be the first hospital to go live in April. Daniel is one of few CIOs who has implemented Epic in two large health systems (he came from Carilion) so I asked him how it was the second time. He says Epic’s greatest strength is that they fully believe and trust their own process — developing their own software, rarely partnering with other companies, and creating finely detailed training plans. The benefit for customers, he says, is that if you just follow their plan, you will have a successful go-live.
Yale New Haven Hospital SVP/CIO Daniel Barchi provides an update on its Epic project. Six practices of 27 physicians are live, with e-prescribing at 91% and 80% of encounters closed the same day. Physician productivity for those docs is nearly back to pre-Epic levels. Greenwich Hospital will be the first hospital to go live in April. Daniel is one of few CIOs who has implemented Epic in two large health systems (he came from Carilion) so I asked him how it was the second time. He says Epic’s greatest strength is that they fully believe and trust their own process — developing their own software, rarely partnering with other companies, and creating finely detailed training plans. The benefit for customers, he says, is that if you just follow their plan, you will have a successful go-live.
Innovation and Research
Researchers at the University of Washington develop medical robots that support the open source Robot Operating System, saying it’s time to get away from proprietary, one-off medical robots and allow universities to collaborate in sharing their applications.
Technology
![]() Ford partners with Microsoft, Healthrageous, and BlueMetal Architects to develop “the car that cares,” which would monitor the health and wellness of drivers. Data would be collected biometrically and through voice capture, then uploaded into HealthVault. And I thought texting while driving was distracting.
Ford partners with Microsoft, Healthrageous, and BlueMetal Architects to develop “the car that cares,” which would monitor the health and wellness of drivers. Data would be collected biometrically and through voice capture, then uploaded into HealthVault. And I thought texting while driving was distracting.
A doctor in Canada gets her smart phone PHR app certified by Canada Health Infoway, only the second app to earn that distinction. She named it Mihealth, with the “Mi” referring to her feeling that adopting digital data in Canada was Mission: Impossible.
The Qualcomm Tricorder X Prize offers $10 million to anyone who can create a Star Trek-like tricorder that can diagnose medical conditions non-invasively. The X Prize Foundation chairman helpfully adds, “We don’t have a requirement that it makes the same noise.”
Other
An AHRQ study finds that 5% of Americans account for 50% of the country’s $1.26 trillion in healthcare costs. The top 1% of spenders account for 22% of the costs.
![]() Could there be a connection? Life expectancy is up two years since 2000 and Hostess, maker of Twinkies, DingDongs (my personal fav), and HoHos, files for bankruptcy protection. Experts blame a shift toward healthy foods.
Could there be a connection? Life expectancy is up two years since 2000 and Hostess, maker of Twinkies, DingDongs (my personal fav), and HoHos, files for bankruptcy protection. Experts blame a shift toward healthy foods.
![]() Here’s a point/counterpoint issue to mull over. Inga and I disagree on the value of CMS’s attestation statistics. Inga thinks the percentage of each vendor’s customers that have attested is a good benchmark, so she did lots of spreadsheet work to compare vendors and to assume that varying percentages among them must be reflective of product capabilities and ease of use in meeting Meaningful Use requirements. I said the information is useless for that purpose since it’s more reflective of unmeasured customer demographics and buying criteria than anything else and that it would be wrong (not to mention statistically indefensible) to use the CMS figures to infer that vendors with a higher percentage of successfully attested users have a better product for earning Meaningful Use money. Feel free to take sides. One thing’s for sure: vendors who massage the data into slick marketing collateral won’t be footnoting their handouts with statistical disclaimers.
Here’s a point/counterpoint issue to mull over. Inga and I disagree on the value of CMS’s attestation statistics. Inga thinks the percentage of each vendor’s customers that have attested is a good benchmark, so she did lots of spreadsheet work to compare vendors and to assume that varying percentages among them must be reflective of product capabilities and ease of use in meeting Meaningful Use requirements. I said the information is useless for that purpose since it’s more reflective of unmeasured customer demographics and buying criteria than anything else and that it would be wrong (not to mention statistically indefensible) to use the CMS figures to infer that vendors with a higher percentage of successfully attested users have a better product for earning Meaningful Use money. Feel free to take sides. One thing’s for sure: vendors who massage the data into slick marketing collateral won’t be footnoting their handouts with statistical disclaimers.
Weird News Andy says “the eyes have it” in referring to this story, in which researchers are working on a smart contact lens that can continuously and non-invasively monitor glucose levels, electrolytes, and cholesterol, sending the results electronically.
Former Steve Jobs mentor turned nemesis John Sculley, who served as Apple CEO for 10 years, is interviewed at the Consumer Electronics Show, where he was promoting a company he advises and invests in, Audax Health. He describes his interest:
The area I am particularly excited about now is healthcare. Healthcare has been the last major industry that hasn’t been touched by technology in terms of productivity and consumer adoption in the way so many other industries have. While I’m not bringing any technology experience to the healthcare industry, I do see some similarities between what I was asked to do when I came to Apple, which was to bring big brand consumer marketing to Apple and carry it over to the whole Silicon Valley industry – because everybody does that today – well that same opportunity exists today in healthcare. Health innnovation enabled by digital technologies to build big consumer service brands, is an incredibly interesting complex problem to work on. Audax is really the first social health company and it’s focused on consumer engagement in the healthcare space bringing in a lot of the social media technologies and experiences that have been learned from companies like Facebook and Zynga and others.
The federal government adds insurance fraud to the list of charges faced by a Louisiana doctor that also includes possession of child pornography. The doctor was medical director for a company that monitored neurophysiologic surgeries over the Internet, billing insurance companies for their time. He and the company are accused of billing for surgeries in which no Internet connection was established, padding their billed hours, and instructing non-physician employees to log on to the monitoring system and pose as physicians for billing purposes.
An Indiana health insurance plan alerts 2,700 members that their records may have been exposed on the Internet in February 2011, when a server was inadvertently opened up to the Web during an upgrade.
Sponsor Updates
- SRS helps its customer Midwest Ortho (IL) celebrate its successful MU attestation with a tasty-looking cake.
- Pete Rivera of Hayes Management Consulting discusses building leaders and improving team effectiveness.
- Picis will participate in this month’s 2012 Military Health System Conference in Maryland.
- OnX and MEDSEEK enter into a strategic partnership that allows OnX to distribute all of MEDSEEK’s enterprise patient engagement solutions.
- MED3OOO shares details of InteGreat EHR’s improved KLAS scores.
- Minnesota’s REC recognizes e-MDs customer Christopher Wenner, MD for being one of the state’s first providers to achieve Meaningful Use.
- Gateway EDI and AAPC align to offer ICD-10 training for practices, starting with a January 24 Webinar.
- Orion Health opens its 14th international office in Paris.
EPtalk by Dr. Jayne
It may only be Thursday as I write this, but I’m really wishing it was Friday. This has been a hectic week full of clinical snafus and customer services annoyances.
The first guilty party is HIMSS, whose registration system apparently malfunctioned last month. HIMSS12 registrants were charged a zero dollar amount for their HIMSS renewals. I received an e-mail notice about the registration problem and was told that someone would call me to discuss whether or not I really wanted to renew. They did, while I was seeing patients. I didn’t want to ignore it and risk a snafu in Las Vegas.
I called the customer service number left on my voice mail and the answering staffer had no idea what I was talking about. After more than 15 minutes on the phone and two call transfers, they finally got their act together. I hope the conference itself runs much more smoothly. And to HIMSS, let me introduce you to the concept of service recovery. If you accidentally undercharge people, let it go and use it as a lesson learned. Did that many people really register on those two days that you are going to suffer without the extra $160 per person? Goodwill is invaluable.
The second guilty party was the staff at Well-Known University Medical Center whose performance at the check-in desk gave new meaning to the phrase “epic fail.” Not only did they insist that my insurance information wasn’t in the system (doubtful since it just paid a claim last week on another appointment) but they were also rude about it. As I sat in the waiting room, I was also annoyed by their ham-handed questioning of patients on race and ethnicity. I wanted to jump up and intervene with some better scripting.
If organizations can’t even handle those customer service basics, I have no idea how they’re going to achieve Meaningful Use, let alone be a meaningful participant in an ACO. Not to mention that they didn’t ask everyone about race and ethnicity. I’m not sure if they just “assumed” for the rest of us or if they decided to judge by appearance.
The final straw was a resident physician who actually was using his BlackBerry to e-mail or text during my visit. Really. Talk about smartphone distractions. He set it on the table between us and typed as he was doing the exam. I know for sure he wasn’t documenting in the EHR because the scribe was tapping away at the PC in the corner.
The resident didn’t think it was funny when I asked him if I was keeping him from something important. He did sheepishly put it in his pocket. Maybe he should have noticed the “faculty” label on my encounter bill. Oops!
Lest you think I’ve just become Angry Jayne, some good things did happen this week. Inga and I strategized on the coveted HIStalkapalooza beauty queen sashes and I have narrowed down the list of candidates who are vying for the chance to escort me to the event.
HIMSS released their list of its 2011 Best Hospital IT Departments. Texas Health Resources, whose IT shop is led by contributor Ed Marx, is listed for large hospitals.
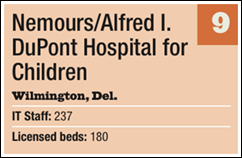
I’m curious about Nemours/Alfred I. DuPont Hospital for Children, which is described on the “medium hospitals” list as having 237 IT staff for its 180 licensed beds. I could certainly do a lot more with 1.3 staffers per patient. I wonder what their nursing ratio is?
Life Technologies Corp. announces that its new Ion Torrent genome sequencer will be able to map an individual human genome in a single day for less than $1,000. Although technically this is HOT, sequencing of a person’s genome brings up lots of controversial ethical and legal issues, not to mention the cost of the human expertise needed to transform the genetic data into something meaningful and to then counsel patients.
The absolute highlight of my week, though, is this delightful video about computers in medicine circa 1964. Thanks to Rockstar HIStalkapalooza correspondent Evan “Velvet Jacket” Frankel for making my day. See you at HIMSS.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.












































































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…