Dan Paoletti is CEO of Ohio Health Information Partnership of Hilliard, OH.

Tell me about yourself and about OHIP.
I’ll start with the Partnership since that’s really what it’s about. The Partnership is a non-profit created about 2 1/2 half years ago by the Ohio Hospital Association, the Ohio Medical Association, the Osteopathic Association, the State of Ohio, as well as another non-profits. It was designed to apply for the federal ARRA grant dollars that had just been issued. We were awarded the state-designated entity for health information exchange in Ohio by the governor at that time and were awarded those federal dollars as well as we were awarded about $28.5 million of Regional Extension Center monies to help providers adopt electronic medical records.
My background is very simple. I was vice president with the Ohio Hospital Association. Previous to that, I worked for Johnson & Johnson. I’m kind of a data geek. I am really here just to facilitate the grassroots effort of the Partnership.
Ohio is progressive when it comes to healthcare technology, even down to Board of Pharmacy regulations that are both admired and feared. Compared to how other states or organizations have set up their HIEs and RECs, how is your structure different or better?
It’s hard to compare if we’re actually better, but I think we are different. We decided very early on that we were going to use the resources and the expertise that existed already in the communities throughout Ohio. There was no reason to layer on another complex organization on top of all that. We are really a facilitating body to gather together the resources that exist in the state, like connecting the dots and get everybody working in the same direction.
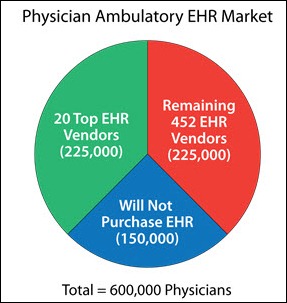
Most of the work is being done at the community level, the grassroots level. It took us a while to get started. We started off pretty slow, but right now I believe we have more doctors than anybody signed up in the country. We just passed 6,000 primary care providers that are using our Regional Extension Center services. That grassroots effort is really the key. That’s what makes the difference.
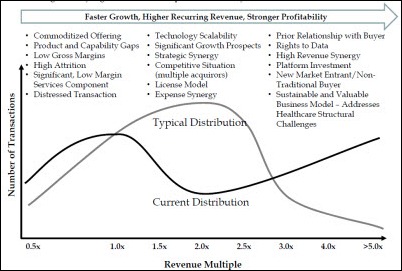
Early on, groups thought their problems were going to be technical, so they were quick to go through a rigorous process of selecting technology vendors and looking at infrastructure. What blew up in their faces was issues related to bringing competitors together at the table or privacy issues that were a lot different than they expected. When you look at your long term strategy, the question always is, “Well, what’s your business model once the grant money runs out?”
Great question. You did hit the nail on the head with that. It’s really not a technology issue, it’s a trust issue.
It goes back to our roots. Our board consists of stakeholders from throughout Ohio that have a lot vested in this and building the trust among each community. We’re targeting not Ohio necessarily as a state, but community by community, and using the community leadership to really get people to the table. That’s the key. It’s not about the partnership. It’s not about the health information exchange, it’s about assisting and solving problems in those local communities. That’s really what’s generated the success model to date.
Privacy is a huge issue. We’ve decided with CliniSync , which is what our health information exchange is called, it’s an opt-in model. We have developed a policy that users of the program will assist and educate the patients that are going into the exchange, what that means. It’s not a law, it’s not a state-level policy, but it’s users of the CliniSync program. We’ve tried to address those very carefully. It’s taken us a long time, but we’ve gotten buy-in from most of the major players and small providers in the state. We’re ready to move forward, and we are.
You must have a good message to get that number of providers on board since they typically understand that there’s patient benefit, but it requires extra work and potentially money from them, plus having to work with competitors that they’re not especially fond of. What selling points make them want to hook up to the HIE?
The core message is it’s about the patient. This is about what’s best for the patients in Ohio and the folks that are receiving care in Ohio. The providers in the state understand that. That’s really what’s most important.
We’re not competing about data. It’s not about competing on that. It’s about competing on service and quality. All of this can have a great effect on that as well as bring efficiencies to the table. Once you sit down and look at specific issues around what the electronic medical records and what the exchange can do for that community-based model and really take it down to that level, people understand. It’s keeping the focus on the patient. That really has had a tremendous affect.
Like all statewide organizations, you’ve got some high-profile, big-ego organizations involved. You also have some that are using systems like Epic, which touts its own private HIE capabilities among Epic users. Has that been a problem when you’re working with groups like Cleveland Clinic?
It’s not a problem. It’s one of those issues that you have to really get down to the patient level and figure out what’s best for the community. I’m not sure about this statement, but I think by the end of this coming year in 2012, we’ll probably have more Epic installs than state in the country.
It’s a unique challenge, but when you look at specific community models, not everybody in every community is using the same systems. You have to be able to communicate with home health agency. You have to be able to communicate with the skilled nursing facility and the competitor down the street. If that patient is moving in and out of all of those, there’s no way that one system solves all that problem.
What we’ve tried to do is position this product as very community-focused, a neutral third party that is a gateway. We’re not storing data. We’re not a data repository. It just allows people to communicate with each other. The focus on the patient has been the key to getting people to work together.
In your experience connecting these different clinical systems that are out there both in the practices and the hospitals, have you found that you had to blaze new ground with vendors who weren’t comfortable with either the technology or the concept of sharing information?
That’s an interesting question. I don’t think technology is quite at the point where we thought it was to allow for the free flow of information. But we’ve worked very closely with most of the vendors, especially the ones that have the bulk of the market, and for the most part they have really been great to work with. They are looking for some standardized process to make all this happen. They really do want this to happen now that this is real, because it is happening and this transformation of healthcare is real.
It has been a challenge. We’re finding a few that are ahead of the others, but we’re using them to blaze that new ground in sharing that information with the others. Even among the vendor community, what we’ve found is they really do work well together as long as you’re not taking sides. That neutrality is key. But it is blazing new ground, without a doubt.
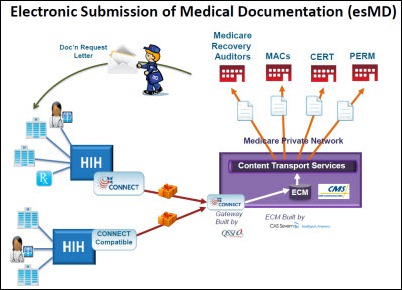
You had an announcement within the last couple of weeks about using the Direct system to communicate with another state, which sounded good on paper, but somebody might say, “Well, it’s not really that relevant. Most care is local.” Why was that event important?
It really did not affect any patient care. This was really a test of whether we could accomplish it.
If you look at what ONC has tried to do – and I would like to just say that this is all happening, this transformation in healthcare around electronic medical records and exchange, is really a result of this stimulus act, and it’s a result of a lot of the great work that ONC has done — Direct is something that they thought was a way to quickly allow people to exchange information. We want to help them be successful. It was really a communication between two clinics. We really didn’t have a whole lot to do with it except to help them facilitate that process. They wanted to see if it could happen, so it was really instigated by the providers themselves.
The important piece was that you had providers that were trying to exchange information across state boundaries. It wasn’t the fact that we could do it, it was their interest, and we were help in enabling that. But what is important about that is there is information that without sophisticated health information exchange in using this Direct Project, these Direct protocols, it can really help the patients.
Let me give you an example. You have a mental health patient that shows up in the ER. That sensitive type of information is very difficult to exchange in a health information exchange, especially with the laws in Ohio. We see the Direct protocols as a way to exchange some information, with the patient’s permission, explicitly to another provider that they might be going to for a follow-up care. We think there are some definite use cases that that can help. It’s an easy way for doctors to do that. Was it going to change the world? No. But it’s a start. The exciting part is that it was between the providers. That’s what we want to emphasize.
According to the announcement, that was the first time Direct had exchanged data across state lines. I would have thought it was further along than that. Is there a technical reason that it hasn’t been done or was it just that nobody felt the need to do it?
I think it has a lot to do with everybody ramping up. The Direct protocols are fairly new. People are ramping up trying to create those protocols and create the secure e-mail systems. There’s nothing new about secure e-mail, but getting the providers provisioned with an address and making sure that everything adheres to HIPAA compliance and all of that — it’s complicated for a lot of folks to get that up on a large scale; especially with a lot of folks that received these state-designated entities. We’re getting close. We just happen to be a little bit out in front, but I think you will see a huge charge of other states and other entities doing this now. We just happen to be a little in front.
What does the big picture look like when there are HIEs springing up from two places that are a mile apart to crossing multiple states, you’ve got the Direct protocol out there for folks to use, and maybe private HIEs that vendors have set up. How will the average medical practice be interoperating?
I’d like to speak for Ohio if I could. The picture here is really community based. The reason that’s important is that the majority of care occurs inside a community. That community could be a single town, it could be a county, it could be multiple counties. But there is some geography where the bulk of care occurs. Ensuring that that information can be exchanged, whether there’s two regional health information exchanges that exist within that community or whether it’s a community without any ability to exchange. The vision that the partnership board and the grassroots stakeholders in the state that are part of OHIP see is that the partnership can be that gateway to facilitate that.
Again, it’s not about us. It’s not about our ability to store and retrieve data. It’s about our ability to allow others to communicate with each other. And for a while – I don’t know whether it will be five years, 10 years, 20 years — there’s still going to be some middleware required to allow that type of exchange to occur. I think that was the vision of ONC — to facilitate this.
In Ohio, our model is just a little bit different, but we’re pleased because we have a lot of folks that have already expressed interest and commitment to make that happen regardless of where they stand technology-wise. That’s our vision, it will be interesting to see what happens though in the next five or 10 years.
The jury seems to somewhat be out on whether Regional Extension Centers are really increasing EHR adoption and whether they’re helping technology improve outcomes and reduce costs. Do you get the sense that they’re accomplishing what they were supposed to?
Our process is a little bit different. It all starts with electronic medical record adoption. It’s hard to accomplish all that without widespread adoption, so that’s where we spent the last two years, really working with our community leaders to adopt the electronic medical records. The next stage is working with the community stakeholders to begin to exchange that information and get a solid base of exchange going so we can start to work as a community on the outcomes and improving quality.
It’s connecting the dots. It’s been a phased approach. I think it will be difficult to accomplish the vision that many people have set without that kind of phased approach. We think we can, because we are accelerating things here in this state. Adoption is the key.
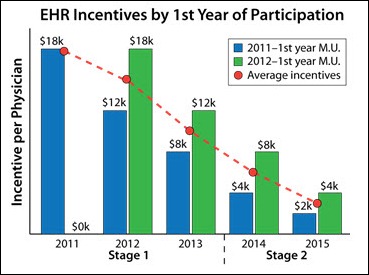
There was huge interest in HITECH money early on, but it’s starting to look like some folks gave up or decided it wasn’t worth doing. Are you seeing people who thought they might be going with electronic health records who saw the wall in front of them and decided to stick to where they are?
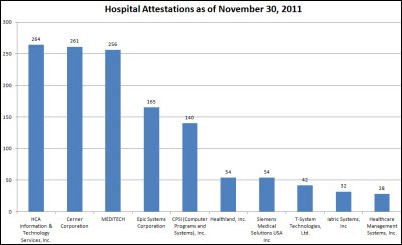
In the beginning, there was a lot of doubt and a lot of concern. I do think we did have some people drop off. But what we did here in the state is develop that grassroots support mechanism, so the physician and the practices and the small hospitals weren’t out there by themselves. They had a support structure in place. Because of that support structure, I think you will see an incredible acceleration of Meaningful Use attestation in 2012.
Ohio, I believe, ranks third as far as Medicaid payments for Meaningful Use and we also are at the top as far as Medicare attestation. Our goal for next year is to help 10,000 providers attest to Meaningful Use, not just primary care providers, but all providers. It’s pretty lofty, but because of that support structure, we’re trying to accelerate and keep things moving forward, because without that, we’re not going to see the benefit. That’s our number one priority. The key is that support structure — they have to have somebody to fall back on.
Is there resistance to the check-off for Meaningful Use that it isn’t really directly related to patient care?
That’s a very difficult thing to answer, especially where we are right now. Is the Meaningful Use criteria going to directly affect patient care? I think it will, in the sense that as providers have to work towards meeting that, it’s going to naturally bring along more and more of the practices as far as how it’s going to affect that patient outcomes. It was a great starting point, but what people have to realize is there’s only so much at the federal level that they can make happen. It really comes down back to that community level in putting the support structure in place to help people meet Meaningful Use.
Then make the next step to help them exchange that information, then get these projects together that will help providers learn from each other and really make the impact on patient care in the outcomes and the efficiencies — because we have to have the efficiencies as well. It will happen. It’s just coordinating all that together, which is a monumental task.
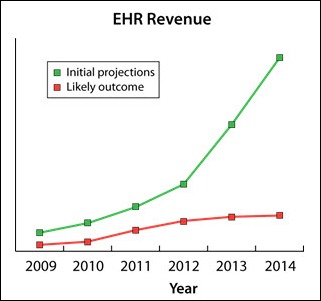
Every transformation is hard. It’s about having that support structure in place at the grassroots level to help facilitate that. It will happen. We spent a lot of time looking at the return on investment of electronic medical records, return on the outcomes of care of electronic medical records. I think there’s enough documentation out there now to prove that yes, it does have an affect. We want to be able to prove it has a significant effect. We think in a couple of years that we’ll be able to do that.
If you look down the road, let’s say five years, how will you know that you’ve done the job you hoped to do?
I can tell you the goals we have in place. Our board and our stakeholders make sure that we’re very goal-oriented.
To document success is the number of providers that have adopted; the number of providers that have attested to Meaningful Use; the number of providers and institutions that are sharing information; and then ultimately getting the entire community — the payer community, the employer community, the patient-consumer community, as well as the provider community — to get enough data to document that we have had an impact on the outcomes and the cost of care. And getting everybody involved in that process.
Can I give the exact metrics that we’ll need to prove that? No. But we have enough momentum now that I believe in five years, at least in Ohio, we’ll be able to prove what kind of success that this whole thing has caused. We’re pretty excited about that.
Any concluding thoughts?
This is really an exciting time for Ohio. ONC has enabled us to jump on board with this and provided the funds we’ve needed to help create transformation here in the state. It’s not about our organization. It’s really about the folks out in the community doing the work. We’re here to help them, and we hope to be one of those models of success that people can point to and say, “Look, if you can do it like this, you’ll be successful.”


























































































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…