HIStalk Interviews Larissa Lucas MD, Senior Deputy Editor, DynaMed
Larissa Lucas MD is senior deputy editor of DynaMed of Ipswich, MA.

Tell me about yourself and the company.
I’m a general internist. I trained at Cambridge City Hospital. I practiced there in primary care after my training.
I joined DynaMed and EBSCO Publishing about five years ago. DynaMed is a point-of-care reference tool to help clinicians answer questions in an evidence-based way while they’re with their patients. EBSCO Publishing is a larger publishing company that provides information through databases and eBooks and other technology to libraries around the world.
You called DynaMed a point-of-care reference company, which I assume is a somewhat different model than the company had when you started with them. How important is it to push the information out where it can be used?
It’s very important. Physicians are challenged today with so many changes in the healthcare system — needing to use electronic health records, communicating to patients through e-mail, and the volume of evidence that is published. It’s nearly impossible to keep up with all that information. It’s critical for physicians to have that information at their fingertips where and when they need it.
If you were to pull 1,000 patient charts and compare that to the evidence that you have on record in your product, how much compliance do you think you’d find?
What a great question. That would be an interesting study to do. For my colleagues, they’re probably pretty good. I think physicians in general do the best they can to stay current with the evidence and follow practice guidelines. Using electronic health records and clinical decision support tools certainly has made that easier. I would say a chart review in the last five years would probably reveal a lot more compliance than a chart review 10 or 20 years ago.
Physicians presumably don’t know what they don’t know rather than ignore solid medical evidence. Do you find them to be receptive to being presented with the evidence and then changing their practice?
I think they’re receptive. It’s a matter of time balance. There’s a lot to cover in that 15 minutes. Clearly we want to spend as much time of that 15-minute visit addressing what the patient needs. A lot of the documentation and investigation of the questions that come up needs to happen usually at the end of day, before the day begins, and during lunch.
The problem we’re trying to solve is to integrate that back into patient care, the face-to-face, point-of-care decision point. That’s where you should have the information.
The issue of information needs at the point of care has been studied by a few folks, such as our friends over at InfoPOEMs, Allen Shaughnessy’s group. Many physicians finish their clinical day with five to 10 unanswered questions. That could be disturbing from a consumer point of view, but it can also be disheartening for the physician who probably feels like they just can’t get to all of it in the same day. Creating tools that make that easier is really what we’re trying to do.
Academic medical centers have rounding teams, which you would assume probe the evidence more thoroughly than in the ambulatory setting, where it may be seen as undesirable to leave the patient to look something up. Where do you think the evidence is most heavily used and most lightly used in terms of practice setting?
The scenarios are quite different. Even in an academic setting, you have the team that’s rounding that is really also the education unit. It’s got students and residents in it and hopefully a teaching faculty that’s at the bedside engaging those residents, teaching them what questions to even ask.
There’s a lot more richer learning there, but there’s been a change in the way patients are treated in a hospital now. They’re not in the hospital for very long. A lot of those problems either get solved quickly by an intervention or they’re discharged from the hospital and those problems have to then be resolved outside the hospital.
Even that academic, rigorous learning experience has changed dramatically in the last 10 years so. You don’t necessarily have the opportunity to do the rich investigation at that time.
Studies have attempted to prove that physicians deviate further from the evidence the longer they’ve been out of medical school, which then roughly correlates a patient’s mortality risk to the age of their physician. I notice that DynaMed was recently voted by Harvard Medical School students as one of their top five favorite apps, so I was thinking that maybe having residents fresh out of school using apps like yours would influence the attending more than if that same doctor was out on their own in a non-academic setting.
Oh, absolutely. I agree with that. It’s very important to have the students and residents around. They’re asking those key questions and they challenge us to answer the “why.” Products like DynaMed also challenge the users.
People define evidence-based medicine in different ways. I like to see it as understanding why we make our medical decisions, not just which medical decisions we should make. Many guidelines, many decision support tools, will put a patient on a protocol that doesn’t actually require a lot of thought. Sometimes that’s more efficient, sometimes not.
From an academic standpoint, I prefer we as educators, life-long learners, and physicians think about, “Why are we doing it this way?” instead of, “What should I be doing next?” Investigating the evidence and synthesizing it around that clinical question helps answer the “why.” Certainly students and medical students and residents challenge us to do that.
Do you think having reference material available on an iPhone or an iPad has changed the willingness of physicians to use information at the point of care than when it existed only as a book they had to go find?
Definitely. Having it at the fingertips makes it a lot easier. Even as a busy clinician, you can integrate it more easily into your workflow, because now it actually seems realistic that you could achieve that steady state of having some tool that you can constantly look things up on and stay current. Before, it was such a daunting exercise that I would think it was overwhelming to physicians to think, “How could I ever look everything up that I don’t know?“ Now it’s much easier to do that.
The ideal point of inflection would be the EMR, where you have patient-specific information available on the same platform from which the treatment decision will be created. What’s the level of integration of your product within applications from vendors like Epic, Cerner, and Meditech?
DynaMed integrates very well with electronic health records. Our structure is very templated and volatized. You can see the answer to your question very quickly and you can launch different sections depending on whether you’re interested in diagnosis or treatment.
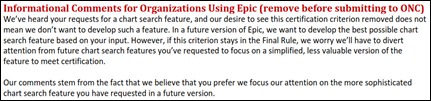
In Epic, it can integrate all the way down into the problem list. It seems to be more of a limitation on the EMR side than on our side. One of the challenges of the EMR is that each one is so different it’s hard for all of that technology to talk to each other. But we integrate very well, and with order sets, too.
We collaborate with Zynx order sets to support some of their evidence. Users can link right to DynaMed or the Zynx evidence. That’s really where we need to be, because that’s now where physicians are interacting with their patient, and they’re interacting with their own question and intellectual curiosity.
Obviously DynaMed will continue to research the literature, but is it a different mission to work with these vendors to turn your information into more useful forms? You have more incentive than they do to accomplish that.
Yes. I think that’s on the technology side, not so much for us editorially. Editorially, our prime objective and vision stays the same. We certainly have enhanced our interface quite a bit in the last year, but more in response to our user feedback and also a need in the market for a tool that both sends out alerts and is a searching tool. We added that alerting feature as well. That doesn’t interact with the EMRs, but we are modifying the way that we’re producing the content a little bit to answer some of those demands from the market.
Do you have examples of how customers are using the information at the point of care?
We have people using it on iPads and iPhones, obviously, and we have quite a few customers using it integrated within Epic and within Meditech. I’ve seen it in Epic, either in just the InfoButton, the information drop-down menu at the top where an institution may have links to multiple resources that they subscribe to, all the way to an InfoButton right next to the problem list so that you could click on the diabetes in the patient’s problem list and launch the topic in DynaMed that would about diabetes.
Is the InfoButton the least common denominator, or is the look-up function even more standard?
All EMRs have the look-up function, usually in their top menu where institutions can put links to external web sites that have information. That’s the most basic integration that anybody can do.
The InfoButton is still somewhat unusual for a vendor to enable?
Yes. It just takes a little bit more technology.
Do you have significant usage by nurses or other clinical users who aren’t physicians?
Absolutely. DynaMed is part of a suite of point-of-care medical products that use the same evidence-based methodology and literature. We have one for nursing — that’s Nursing Reference Center. We have Rehabilitation Reference Center for physical therapists, Patient Education Reference Center for patients.
If a hospital subscribes to all those products, they’re fully integrated within one search engine. We also provide full-text data bases to Cochrane reviews and other journals in Medline. Subscribing to the whole suite of medical products gives you information across different disciplines. We have quite a few users that go between products, so nurses will look something up in Nursing Reference Center, but then they also jump over to DynaMed and use that as well.
How is DynaMed differentiated from its competitors?
We’re all very different. DynaMed is based on the critical appraisal of the literature. Then the rest of the content is built around that, but it’s synthesized around the evidence in presenting the limitations and the strengths of the research that support our decision-making.
The other products in the market – UpToDate, ACP PIER, BMJ Point-of-Care — many are published still in a traditional textbook publishing model. The whole chapter is written by the author and then updated and kept current with the literature. It’s just a very different model. They’re all very good. I think we’re all very good at what we do.
How we’re set aside from the competition is that we are very focused on the critical appraisal piece of the evidence and providing the information to support the medical decisions so that physicians are more informed about why they’re deciding to go down a certain pathway.
You have folks on the front line that are contributing their expertise as well, right?
Yes, all over the world.
Is that hard to coordinate?
It’s very challenging. We have sought experts from around the world. Sometimes time differences are challenging to deal with, but we try to be global.
We have a team of very experienced medical writers from varied scientific backgrounds. They’re very good at what they do, objectively evaluating the evidence. The collaboration with clinicians happens very smoothly and very naturally to make sure that relevance piece is part of what we do. With validity, anybody can follow a protocol in how to critically appraise and assess the validity of a trial, but the relevance needs to happen from the physician level. We’re always engaging with other physicians to get that input.
Do you know how your products are being used and being received by frontline physicians?
Every page has a “send comment to editor” button. That e-mail goes to myself, the editor-in-chief, and our support team. We get a lot of feedback from customers who are using it right at the point of care. That’s very helpful. It helps us drive our editorial priorities as well when we hear directly from customers.
We also work closely with many residency programs and get their ongoing feedback for how it’s used in their practices, in their education, and in their workflows. Our peer reviewers are also always giving us feedback. We definitely solicit feedback and we get it passively from our users. We love it. We’re dynamic. That’s why we have that name.
I once suggested to one of your competitors that it would be interesting to analyze the lookups of a reference product to infer information about prevalence of disease or outbreaks, like people who are always trying to use Twitter or Google searches to spot epidemics early.
That would be interesting. I’ve seen some of that research. Certainly our influenza topics had huge usage when we had the outbreak of H1N1, but typically our usage logs are consistent with what is seen in most general practices. Our top-hit topics are asthma, diabetes, pneumonia, sepsis, heart attacks, and urinary tract infections.
It’s interesting to me, because you’d think some of the more common diseases that we see in practice, we wouldn’t have to look up answers to questions because you see it so often. You should be comfortable with it. But I like seeing that data, because it tells me my colleagues are constantly striving to see if there’s anything new. I’ve treated 50 UTIs this month, but is there anything new I can learn? In that sense, it’s very rewarding to see those usage logs are hitting some of the major topics.
Any final thoughts?
The challenges facing physicians are so complex. I really enjoy being part of this tool that’s hopefully going to make practicing medicine easier for physicians and make physicians feel more comfortable as they have to make quick decisions in their patient care. It’s definitely going to improve quality. It’s definitely going to improve patient outcomes. Those studies are yet to be determined, but I’m hopeful that all of this technology is going to to make it easier to practice medicine.














































































The author here keeps introducing irrelevant ideas. It's true that there are nimble organizations and bureaucratic ones. What is the…