There was a recent report pointing to increased Medicare costs when patients returned to traditional Medicare, of course assuming that…
News 11/30/12
Top News
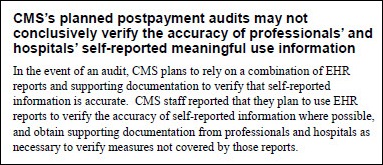
The Office of the Inspector General finds that CMS has not implemented adequate safeguards to verify the accuracy self-reported EP and hospital data for the MU program. It also says that the audits CMS plans to conduct after the fact may not work, either. OIG recommends that CMS randomly select providers to provide supporting documentation for pre-payment; issue guidance detailing the types of documentation that providers should maintain to support compliance; and require certified EHRs to produce reports verifying the achievement of MU measures. Medicare hasn’t audited any of the $3.6 billion it’s paid out so far. Acting CMS administrator Marilyn Tavenner doesn’t like the idea of pre-payment review, saying it could “significantly delay payments to providers” and “impose an increased upfront burden on providers.”
Reader Comments
![]() From Uncorked: “Re: MyWay switch. I’ve learned the upgrade that Allscripts is offering its customers from MyWay to Pro does not include a detailed conversion of financial data, meaning users have to work the old balances in MyWay. Sounds painful.” The details on the MyWay to Pro upgrade are on the client-only section of the Allscripts Web site, so I can’t verify. However, since detailed conversion of financial data between disparate systems can be quite complicated and time consuming, maybe the balance forward option is actually the lesser of two pains.
From Uncorked: “Re: MyWay switch. I’ve learned the upgrade that Allscripts is offering its customers from MyWay to Pro does not include a detailed conversion of financial data, meaning users have to work the old balances in MyWay. Sounds painful.” The details on the MyWay to Pro upgrade are on the client-only section of the Allscripts Web site, so I can’t verify. However, since detailed conversion of financial data between disparate systems can be quite complicated and time consuming, maybe the balance forward option is actually the lesser of two pains.
From NoNamesPls: “Re: MD Anderson. To release an EMR RFP in January.” Unverified.
From Lucille Carmichael: “Re: Nuance. Planning to spin off Salar, which it acquired with its Transcend acquisition, possibly as early as Friday.” Unverified.
HIStalk Announcements and Requests
![]() If your week has been anything like mine, you are still recovering from all your thankfulness last week. In case you missed any HIStalk Practice news, here are some highlights. ONC says the percentage of physicians e-prescribing on the Surescripts network through an EHR has jumped from seven percent in 2008 to 48 percent as of June 2012. Almost 10 percent of US residents now receive their healthcare through an ACO. The highest-rated EMRs in an AAFP-member survey are Praxis, Medent, Healthconnect, Amazing Charts, and SOAPware. Pediatricians lag other specialties in EHR adoption. Practice Wise’s Julie McGovern offers key points for selecting an EMR vendor. Dr. Gregg muses about corporate chaos and HIT. Thanks for reading.
If your week has been anything like mine, you are still recovering from all your thankfulness last week. In case you missed any HIStalk Practice news, here are some highlights. ONC says the percentage of physicians e-prescribing on the Surescripts network through an EHR has jumped from seven percent in 2008 to 48 percent as of June 2012. Almost 10 percent of US residents now receive their healthcare through an ACO. The highest-rated EMRs in an AAFP-member survey are Praxis, Medent, Healthconnect, Amazing Charts, and SOAPware. Pediatricians lag other specialties in EHR adoption. Practice Wise’s Julie McGovern offers key points for selecting an EMR vendor. Dr. Gregg muses about corporate chaos and HIT. Thanks for reading.
On the Jobs Board: Marketing Programs Manager, Meditech Clinical Trainer, National Sales Director, Ambulatory Implementation and Deployment Managers — athenaclinicals.
Acquisitions, Funding, Business, and Stock
The mobile interactive health advice platform HealthTap acquires the health business of Avvo, including its directory and network of providers.
Ginger.io, which analyzes sensor and patient-entered smartphone data to for the equivalent of a “check engine light” for patient populations, raises $6.5 million. The investor is Khosla Ventures, whose founding partner Vinod Khosla famously predicted several weeks ago that machines will replace 80 percent of doctors (some of his other investments include iPhone attachments for heart monitoring and diagnosing ear infections). Ginger.io is based on research conducted at the MIT Media Lab. The company acquired another startup, Pipette, earlier this year for its technology that claims to reduce hospital readmissions by reviewing patient-reported outcomes. Travis reported the acquisition on HIStalk Connect back in March, where he concluded,
Ginger is a company we are going to hear a lot more about in the coming years. They have a clear focus on learning about patient behavior and proactively trying to address potentially costly events. The main question will be how much money can Ginger make quickly from pharma research or how much money can it raise to sustain itself until the healthcare industry is ready to pay for services like this. Either way, this acquisition is good for mobile health startups and Rock Health.
Sales

Stormont-Vale Healthcare (KS) selects Hyland Software’s OnBase enterprise content management solution for integration with its Epic ambulatory EMR.
Yale-New Haven Hospital contracts with Mediware for its Transtem software for tracking the use of stem cell products in providing patient care.
OnFocus Healthcare adds 75 hospital clients of its OnFocus | epm software during the company’s fourth quarter.
Pomona Valley Hospital Medical Center (CA) selects Dell and Siemens Healthcare to provide diagnostic image archiving and sharing services.
BJC Healthcare (MO) expands its use of the Surgical Information Systems perioperative information system to Saint Louise Children’s Hospital and Barnes-Jewish West County Hospital.
Santa Clara Valley Health and Hospital (CA) awards CSI Healthcare a contract to support its Epic initiatives.
Beaufort Memorial Hospital selects the Medseek Empowered solution to expand its patient engagement initiatives.
St. Joseph Health System (TX) chooses GroupOne Health Source for EHR medical billing services.
Ophthalmic Consultants of Boston (MA) deploys MedAptus for professional charge capture in its office and ambulatory surgical center locations.
People
SPI Healthcare appoints Ken Christensen (Health PCP) SVP of operations.
CareTech Solutions names Robert M. Johnson (Palace Sports & Entertainment) CFO.
Joseph Kvedar, MD, director of the Center for Connected Health of Partners HealthCare, signs on as a principal with Wellocracy, but will continue in his role at CCH. The new company will focus on personal activity trackers and motivation tools that integrate healthy activities into busy lifestyles, initially producing books. He’ll be joined by a self-help author, a personal trainer turned physician, and a media relations expert.
Bill Bria, MD (Shriners Hospital for Children) is named chief medical officer of business intelligence software vendor Dataskill.
Peter Henderson (PatientKeeper) joins social networking-based employee wellness vendor ShapeUp as COO.
Announcements and Implementations
Washington DC Mayor Vincent Gray announces the go-live of Direct Secure Messaging in the district using Orion Health’s technology platform.
RelayHealth announces that it will provide an open, vendor- and payer-neutral platform for patient identity management, patient consent management, and other technology services to enable a longitudinal patient record. The technology will allow providers to embed a cross-entity MPI into their native systems and enable patient identification across multiple systems.
Jennie Stuart Medical Center (KY) goes live on Ingenious Med’s Impower charge capture solution.
The Kansas HIN and ICA share patient data with the CDC’s Biosense public health tracking system.
Government and Politics
An opinion piece in The Wall Street Journal written by former US Senator George LeMiuex (R-FL) says the government is doing little to stop the estimated $100 billion per year that Medicare loses to waste, fraud, and abuse. He had proposed a credit card-like fraud prevention system that would stop questionable claims before they’re paid, but that’s the $77 million system developed by Northrop Grumman and Verizon that had stopped less than $8,000 in questionable payments in its first eight months. He concludes that the problem is “bureaucrats hiding in their own ineptitude.”
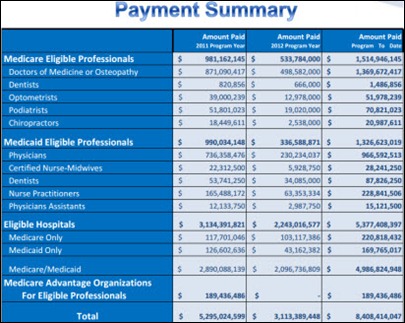
CMS has paid more than 150,000 EPs and 3,238 hospitals $8.4 billion in MU incentives through the end of October.
CMS extends the Medicare MU attestation deadline for New York and New Jersey hospitals affected by Hurricane Sandy. Eligible hospitals must submit to CMS and extension application to extend the attestation deadline from November 30, 2012 to the spring of 2013.
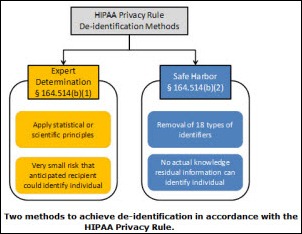
HHS issues a guide for de-identifying patient data to meet HIPAA privacy rule requirements.
British troops in Afghanistan are using a portable 3D camera to assess battlefield injuries and send images around the world for second opinions.
Surgical Theater LLC sells its first 3D imaging surgical rehearsal platform. It generates statistical models from an individual patient’s scanned images, providing life-like feedback using flight simulator technology that allows the surgeon to practice the procedure hands on. The first customer is University Hospitals Case Medical Center (OH), which isn’t surprising since its co-originator is the chair of the hospital’s neurosurgery department and the product bears his name. FDA approval is pending. The co-founders are former members of the Israeli Air Force, with my reason for calling out that fact becoming more clear as you read further down the page.
Other
The California Department of Public Health fines Prime Healthcare Services $95,000 after determining that Shasta Medical Center violated patient confidentiality when it shared a woman’s medical information with journalists and sent an e-mail about her treatment to several hundred hospital employees. The disclosures were made when the hospital was seeking to respond to a news story featuring the woman and the hospital’s alleged overbilling of Medicare.
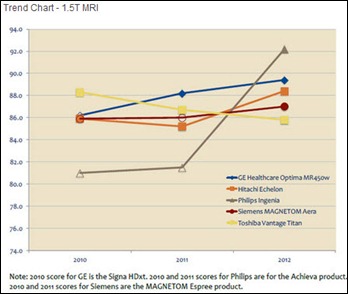
Philips moves from last place to first place in KLAS’s review of the MRI market.
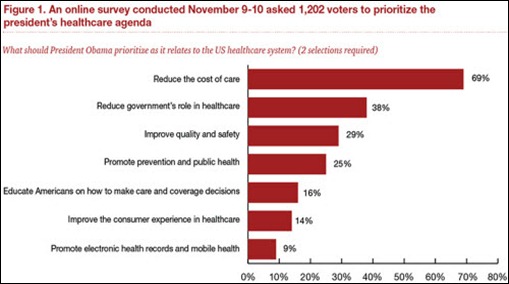
A survey finds that promoting EHRs and mobile health are a low priority for voters compared to other healthcare issues. When asked where federal healthcare spending should be cut, 50 percent of voters said payments to providers should be reduced, while 42 percent said the government should spend less on healthcare IT.
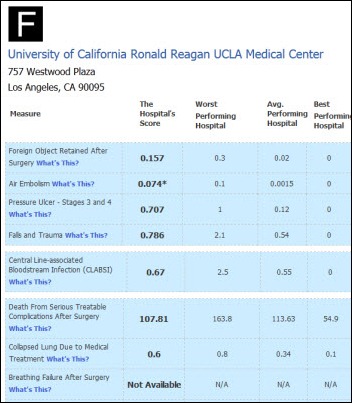
Leapfrog Group’s second round of hospital safety ratings show significant swings in the months since the original report after it changes its methodology and uses newer data, with 103 hospitals moving from a C to and A, two changing from A to D, and an overall 8 percent moving at least two grades. Ronald Reagan UCLA Medical Center earned an F grade along with 24 other hospitals, while Cleveland Clinic took home a D. Predictably, the high-profile hospitals with the bad grades denounced the methodology when stung by local press coverage of their embarrassing results, claiming they’ve improved vastly in the 1-3 years since the information was collected.
The Bureau of Labor Statistics predicts that IT positions in healthcare and social assistance will account for about 28 percent of all new jobs by 2020.
A New Zealand sleep expert blames mobile devices for a 50 percent jump in sleeping pill consumption by young people, saying, “People go to bed with their iPhones and iPads and expect to be able to then go straight to sleep, but realistically, you can’t do that. You really need to put these devices down about an hour before you go to bed.”
I was interested in the answer Kobi Margolin gave to my interview question about why Israel produces so many healthcare IT companies that sell products to the US. He suggested reading Start-Up Nation, which describes the business climate there. I plan to do so, but from the Amazon reader comments, some of the reasons that the country is so successful despite being constantly at war, surrounded by enemies, and devoid of natural resources are: (a) mandatory military service that encourages innovation and forges early social networks; (b) Jewish tradition; (c) open immigration that encourages brilliant innovators to come there; (d) a tradition of young people traveling all over the world due to the small size of the country; (e) government policies and culture that supports entrepreneurism and the questioning of authority; (f) a flat hierarchical society; (g) acceptance of failure in the quest for success; (h) early maturity and lack of belief that people shouldn’t start businesses without a lot of experience, emphasizing instead agile, problem-solving generalists; (i) mashing up technology with other disciplines in fresh ways; and (j) great universities. In other words, pretty much exactly opposite what we have in the US except for the great universities part. If you’ve read the book, feel free to chime in.
An article in The Wall Street Journal raises the question of the ownership of data created by implanted medical devices like defibrillators. It’s your body, but only the device manufacturer (and possibly your doctor, if you see one regularly) can see what it’s emitting. A Medtronic spokesperson says, “Our customers are physicians and hospitals” and says demand is low and patients couldn’t make sense of their data anyway, but then admits that the company is thinking about selling its patient data to health systems and insurance companies. Another senior Medtronic executive calls the information it collects “the currency of the future.” The company has created a data unit specifically charged with creating a business around selling patient data, working the loophole that only providers are covered by the 17-year-old HIPAA regulations, not device manufacturers. One patient paid $2,000 to take a technician’s class for reading the reports, but still has to pay his cardiologist for a visit to get the data.
Remedy Health Media launches a service that will send electronic newsletters to patients with specific conditions under the name of their doctor, who pays the company for use of its patient data management system. The company says health reform gave them the opportunity, while advertising drug companies give them their profit. It’s a double-opt in service due to comply with spam laws, meaning patients need to sign up and then click a link on a welcome e-mail indicating their interest to receive further e-mails. Some of the company’s brands include HealthCentral, The Body, RemedyMD, and My Refill.
Attendees of an auction at a bankrupt and closed Pennsylvania hospital claim to have seen unattended medical and employee records and computers up for bid that were displaying patient information. The bankruptcy trustee claims the medical records were in roped-off areas and the computers had been wiped clean, but a bidder says that’s not the case.
An excellent article in the Toronto newspaper questions whether e-health will ever deliver a return on investment in Canada. It calls out the massive spending on eHealth infrastructure, implying that it’s a desperate shot at addressing the question, “Could the elderly bankrupt Canada?” but points out that for all the investment, Canada is still well behind most of the industrial world, with 80 percent of its physicians still using “a fax machine running full blast against a ceiling-high backdrop of manila files.” It says that Canada’s efforts are looking a lot like those of the UK, where ambitious and expensive programs tanked with little to show for it other than billions of taxpayer pounds transferred to consultants and contractors. A former deputy health minister had an interesting thought: instead of buying EHRs for everybody, which he says will cost more than the healthcare services they consume, he suggests providing them only for seniors and people with chronic disease since 1 percent of Ontario patients have been found to consume 50 percent of hospital and nursing home costs.
Weird News Andy wonders if this is where we’re headed. In England, sick babies are being put on “death pathways,” with the rather lurid newspaper article quoting one doctor who admitted that he took part in “starving and dehydrating ten babies to death in the neonatal unit of one hospital alone.” A hospital nurse calls it “euthanasia by the back door.” An investigation will determine whether hospitals earned bonuses for hitting death pathway targets.
Sponsor Updates
- Nuance gives the $73 (at Walmart) Philips Digital Voice Tracer dictation recorder its highest rating for recording and voice recognition accuracy with Dragon Naturally Speaking.
- 3M announces details of its 2013 Client Experience Summit, set for April 2-4 in Tysons Corner, VA.
- Liaison Healthcare announces that four out of five global pharmaceutical companies use its integration and data management services.
- The Orlando paper spotlights Kony Solutions and its “cutting edge” app development.
- Levi, Ray & Shoup publishes a case study highlighting the benefits that Memorial Hermann Healthcare (TX) realized simplifying output management.
- SuccessEHS integrates the Midmark IQvitals device with its EHR.
- BridgeHead Software releases a white paper highlighting the crucial concerns of image availability.
- Besler Consulting offers a free comprehensive summary of the Hospital Outpatient Prospective Payment System final rule.
- API Healthcare offers five tips for payroll success in hospital mergers and acquisitions.
- Informatica introduces a global messaging routing capability for the Informatica Ultra Messaging environment.
- The Tampa Bay Technology Forum honors MedHOK with the 2012 Emerging Technology Company of the Year Award.
- Ingenious Med releases software upgrades for its Web and mobile solutions that include a Virtual Superbill to improve charge capture.
- Health Language Inc. releases new terminology mapping to support providers and EHR vendors meeting Stage 2 MU requirements for SNOMED-encoded problem lists.
- iSirona releases Software Makes Sense, a five-part video series detailing the specific configurations and their advantages used by iSirona’s hospital customers to sync medical devices and EHRs
EPtalk by Dr. Jayne
Friday is the last day for HIMSS 2013 Interoperability Showcase submissions. Demonstrations must include health information exchange between at least three healthcare organizations.
Friday is also the last day for Eligible Hospitals and Critical Access Hospitals to register and attest for incentive payments in fiscal year 2012. CMS has a tutorial on YouTube which, strangely, enough seems to have been filmed in front of a green screen that wasn’t replaced by graphics, rendering it nauseatingly distracting.
Finally, a data breach that doesn’t involve a lost laptop or stolen hard drive. A resident physician terminated from the University of Arkansas for Medical Sciences kept patient lists and notes after being terminated in 2010. The resident began to produce the records during a lawsuit against the residency program, leading to a court order to prevent further release.
Discussions at RSNA reveal mixed opinions about releasing radiology results directly to patients. I think many providers would prefer to release only annotated results to patients – those results to which the ordering physician has added comments that explain the clinical significance of the radiologist’s interpretation. There are a lot of vague terms used by some radiologists (clinical correlation recommended, questionable presence of something, etc.) and that leads to fear of patients misunderstanding, which leads to fear of being transparent with results. If health systems are going to release without annotation, maybe they should require radiologists to document results at the 5th grade reading level: “Your chest x-ray looks like the chest x-ray of every other person who lives in your part of the country. I don’t see anything that doesn’t belong there.”
For those whose providers have embraced transparency and are offering patient portals and other engagement platforms, the Family Caregivers Video Challenge offers a chance to tell how health information technology or eHealth tools have helped manage a loved one’s care. Video submissions are due by December 10 and prizes worth $8,350 are at stake.
My hospital has been lucky that this hasn’t happened to us (yet). A NYU staffer inadvertently sends an e-mail that allows a student to accidentally “Reply All” to nearly 40,000 of his classmates. Thousands of students jump on the bandwagon, creating what some termed the “replyallcalpyse.” It’s only a matter of time before it happens here.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg.
More news: HIStalk Practice, HIStalk Mobile.
















The statistic claiming 10% of patients are in an ACO seemed bogus to me, so I followed the link. The report claims a total count of 25M – 31M Americans currently receive healthcare through Accountable Care Organizations.
BUT, 15M patients included in that total are “non-Medicare patients in Medicare-oriented ACOs.” What?
The rationale for including these patients in the total seems to be “In practice, virtually any provider that moves to a value-based contract with its most significant payer—Medicare—will eventually need to move all of its patients to value.”
I am not buying it.
I’m with you Will. I saw that 10% number and instantly thought, lies, damn lies and then there are statistics.
Re: Start Up nation:
“(h) early maturity and lack of belief that people shouldn’t start businesses without a lot of experience, emphasizing instead agile, problem-solving generalists”
So they’re saying Epic’s hiring model is spot-on?
RE: Looking Deeper – Epic hiring model
Have you ever met a provider who felt that the kids just out of school with minimal training were even reasonably able to speak the language of a clinician? Probably not, why do you think so many kids are needed and so many consultants with clinical credentials and experience are needed to implement the “Model” system?
“auction at a bankrupt and closed Pennsylvania” I knew California was having fiscal problems, but Pennsylvania? First Hostess, now Pennsylvania. Sigh. Everything I liked growing up is going down.
[From Mr H] Ha! Fixed. I was in my fifth hour of HIStalk work after a full day at the hospital, an HIStalk interview, a four-mile run, and making dinner for Mrs. H who was home late from work and my fatigue was showing as I added that item as the last part of the post.
“Ginger is a company we are going to hear a lot more about in the coming years. They have a clear focus on learning about patient behavior and proactively trying to address potentially costly events”
Sounds interesting but for the most part don’t patients know they are particpating in unhealthy activities (i.e. fast food, consuming too many calories, lack of excercise, etc…) yet don’t do anythinga bout it?
Reminds me of when I downloaded an app to track calories, interesting for awhile and it did change my habits short term but after awhile I grew tired of inputting the info and no never even pull it up anymore.
We need an app that zaps people into compliance:)
OIG post payment audits…Yikes!
An almost terryfying prospect when you consider: audits of poorly defined processes that where hacked together over several months by people that had little understanding of provider operations, with numerators and denominator definitions that were revised regularly, based on data collection sysytems that were slapped together overnight by revenue hungry vendors.
And last but not least, a government that is bankrupt that is hell-bent on finding ways to reduce provider reimbursement …not to mention the political theatre back drop.
If I was a provider I would not have spent that MU $$ so quick.