Top News

Cerner delivers strong Q1 numbers: revenues up 15 percent, adjusted EPS of $0.37 versus $0.33 a year ago, both in line with analyst estimates. The company also reported its $910.2 million in bookings was an all-time number for a first quarter.
Reader Comments
From Haberdash: "Re: Matt Hawkins. Greenway sent an email to customers saying that President Matt Hawkins is on the way out.” The note, which was sent Tuesday, indicates that Hawkins is leaving the company to pursue “an exciting new leadership position outside of the company.” The departure of Hawkins, who was CEO of Vitera Healthcare prior to the Greenway/Vitera merger, could be unsettling for any Intergy customers already concerned about Greenway’s long term product strategy. I emailed the company Wednesday for a comment but have not yet received a reply.
HIStalk Announcements and Requests

 Mr. H is out and about today so I am flying solo. I am not sure what he’s up to but since I’d like to be sitting on a beach with an umbrella drink, I’m just going to pretend he’s doing something fun like that.
Mr. H is out and about today so I am flying solo. I am not sure what he’s up to but since I’d like to be sitting on a beach with an umbrella drink, I’m just going to pretend he’s doing something fun like that.
Some highlights from HIStalk Practice this week include: EHR vendors could learn from Surescripts’ “alliance of foes” model. The AMA reminds providers to order their ICD-9 codebooks for 2015 now that ICD-10 has been temporarily shelved. CVS MInuteClinic surpasses 20 million patient visits since opening its first in-pharmacy site in 2010. Rushed physicians create frustration and tension for both patients and providers. Orthopedists were the most highly compensated physicians last year. Wikipedia trumps Google Flu Trends and the CDC in tracking flu outbreaks. Dr. Gregg promotes “multiview” as a necessary EMR feature. Thanks for reading.
This week on HIStalk Connect: Nike shuts down its Fuelband activity tracker line, cancels plans to introduce a new tracker this fall, and eliminates 55 of the 70 staff members in the activity tracker business unit. Twitter announces the winners of its #BigData grant program, half of which were healthcare-focused research projects. In an otherwise neglected market, eCaring raises a $3.5 million Series A for a simplified health journal designed to help seniors age in place by trending for changes in physical or behavioral health and alerting appropriate caregivers.
Upcoming Webinars
May 1 (Thursday) 1:00 p.m. ET. Think Beyond EDW: Using Your Data to Transform, Part 2 – Build-Measure-Learn to Get Value from Healthcare Data. Sponsored by Premier. Presenters: Alejandro Reti, MD, senior director of population health, Premier; and Alex Easton, senior director of enterprise solutions, Premier. Once you deploy an enterprise data warehouse, you need to arrive at value as quickly as possible. Learn ways to be operationally and technically agile with integrated data, including strategies for improving population health.
Acquisitions, Funding, Business, and Stock

VMware reports Q1 results: revenues up 14.2 percent and adjusted EPS of $0.80 vs. $0.74, beating estimates.

Kaufman Hall, a provider of financial consulting services and software for healthcare, acquires Axiom EPM, a provider of financial performance management software for healthcare and other industries.

Huron Consulting Group enters into an agreement to acquire the assets of Vonlay.

Quest Diagnostics posts Q1 numbers: revenues down 2.3 percent and adjusted EPS of $0.84 vs. $0.89 a year ago, missing estimates. Quest blames an unusually harsh winter that deterred people from going to its centers for tests.

NexJ Systems acquires Liberate Ideas, developer of a point-of-care patient education solution.

Owlet, developers of a smart baby bootie monitor that measures a child’s heart rate, raises $1.85 million from multiple firms, including ff Venture Capital and Eniac Ventures.
Heart Corporation expands its Hearst Health group and Zynx Health division with the acquisition of CareInSync, the developer of a mobile platform for provider-patient communications.

CTG attributes its 22 percent drop in Q1 profits on lower revenue from its healthcare technology services business. CEO James R. Boldt says the lower revenues are the result of hospitals delaying EMR and other IT implementation projects as they manage Medicare cuts from a year ago.
HealthStream reports Q1 results: revenues up 29 percent and flat earnings of $0.07 per share, beating revenue estimates but missing on earnings.
Sales

Crozer-Keystone Health System (PA), Tahoe Forest Health System (CA), Capital Health (NJ) and Hocking Valley Community Hospital (OH) will implement the InteHealth Patient Portal.
Michigan Health & Hospital Association Keystone Center will use RegistryMetrix from ArborMetrix at 60 hospitals to capture OB data and measure clinical performance.

Johns Hopkins Health System selects Carestream Health’s Vue PACS system.
Southern Illinois University HealthCare selects Allscripts TouchWorks EHR for its physician clinics.

SCL Health System will implement Stanson Health’s clinical decision support system.
People

Population health management and patient engagement provider Rise Health names Connie Moser (McKesson) president and COO. Moser replaces Mark Crockett, MD, who will remain as CEO, and Fred Croft, who will shift to CFO.
QPID Health forms an advisory that includes David W. Bates, MD (Brigham and Women’s Hospital); John D. Halamka, MD (Harvard Medical School); Julia Adler-Milstein (University of Michigan); and Robert M. Wachter, MD (University of California, San Francisco).

Extension Healthcare hires Jill Vavala (CareFusion) as CNO.

Covisint names Michael Keddington (McDermott & Bull Executive Search) SVP of worldwide sales.

The NCQA appoints Michael S. Barr, MD (American College of Physicians) EVP in charge of leading the organization’s research, performance measurement, and analytics efforts.

David J. Bensema, MD moves from CMIO to CIO for Baptist Health (KY).

Essia Health names Rachel Leiber (Providence Health & Services) to lead the company’s EMR implementation services division.

Accretive Health CEO Stephen Schuckenbrock will step down from the troubled company when his contract expires October 2. Last month the company was delisted from the NYSE after failing to file restated financial reports from 2012.
Announcements and Implementations

The Greater Houston Healthconnect network and the Austin-area Integrated Care Collaboration establish health information sharing through the Texas Health Services Authority’s HIETexas.

American Health Network implements eClinicalWorks Care Coordination Medical Record for population health management to manage its three ACOs in Ohio and Indiana.
Via Christi Health (KS), which is owned by Ascension Health, will go live on its $85 million Cerner system June 1 across all of its Wichita hospitals and clinics.
Behavioral Health Information Network of Arizona leverages NextGen’s Mirth Connect platform to become the first statewide behavioral health information exchange in the country.

Lady of the Sea General Hospital (LA) goes live with T-System’s EDIS EV.

The W. W. Caruth Jr. Foundation awards Parkland Center for Clinical Innovation (TX) a $12 million grant to establish the Dallas Information Exchange Portal to connect Parkland Memorial Hospital with local social service agencies.
Government and Politics
HHS says two entities have collectively paid almost $2 million to resolve potential HIPAA violations following the theft of unencrypted laptop computers.
The House Appropriations Committee approves a 2015 budget plan to that would hold back 75 percent of the VA’s requested funds to upgrade its EHR until Congress is convinced the DoD and VA are making progress in their efforts to share EMRs.

CNN reports on the Phoenix VA Health Care System and how delays in scheduling appointments has led to 40 deaths. The report also reveals details of a scheme by VA managers to hide the scheduling delays in order to improve official scheduling metrics. A retired VA doctor claims that the health system maintained a “sham” waiting list that was shared with Washington officials that showed timely appointments, as well as a real but hidden list with wait times of more than a year. To create the secret list, staff entered appointment details into the computer, printed the screen, but did not save what was entered. Patients remained on the secret list until the scheduled appointment was within 14 days, then details were transferred to the sham list and the hard copy was shredded. The US House Veterans Affairs Committee is now investigating.

The FBI warns that healthcare systems and medical devices face an increased risk of cyberattacks because private health data has a higher financial payout on the black market than credit card numbers.
Other

The chairman of the board of supervisors for Riverside County Regional Medical Center (CA) takes Huron Consulting to task and questions its lack of progress fixing the hospital’s financial woes. Huron, which is six months into a $26 million dollar engagement, was hired to implement cost-saving initiatives to address the hospital’s $83.2 million cash shortfall, but so far the deficit has only been cut $1.2 million. The hospital’s CFO defended Huron’s work, noting that the company’s efforts have already contributed to $9 million in savings, but declining patient traffic during the same period has resulted in a $12 million decline in revenue.
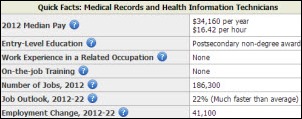
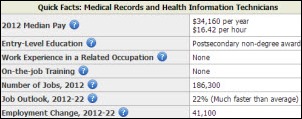
The Department of Labor predicts a 22 percent increase in the number of jobs for medical records and health information technicians between 2012 and 2022.
Health IT, care coordination, and drug shortages lead an ECRI-complied list of top 10 patient safety concerns for healthcare organizations.
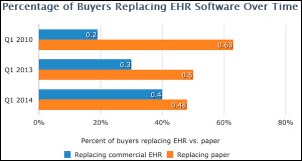
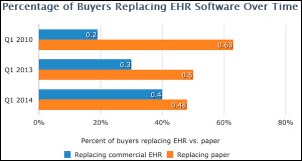
Forty percent of physician practices are looking to replace their existing EHR, according to a Software Advice report. Among buyers replacing their EHR product, the most common replacement reasons: the current solution is too cumbersome and/or integration is needed between applications.
A Rhode Island court issues a consent decree saying that the state’s EHR database CurentCare must be more transparent and offer patients more privacy protection. The ruling stems from a 2010 lawsuit filed by the ACLU that charged the state’s department of health didn’t spell out clearly or publicly enough how patients could remove or change their own records from the database.
A quaky lawsuit out of Oregon: a woman sues her mother’s neighbor after the neighbor’s pet duck attacked her. The duck ambushed the woman without provocation, causing her to fall, break her wrist, and sprain an elbow and shoulder. The victim, a retired nurse, is seeking $275,000 for pain, suffering, and other damages.
Sponsor Updates
- Elsevier will market Stanson Health’s CDS alerts and analytics solutions.
- IDC Health Insights names Wellcentive a leader in its MarketScape report on US population health management vendors.
- Merge Healthcare releases iConnect Retinal Screening for identifying and diagnosing patients with diabetic retinal disease.
- Quest Diagnostics recognizes Liaison Healthcare’s EMR-Link solution with its Quality Solutions Certification for meeting or exceeding HIT quality standards for secure clinical lab ordering and results reporting.
- BESLER Consulting will market the MedAptus charge capture management suite to its clients and MedAptus will promote BESLER’s revenue recovery and compliance services.
- McKesson Business Performance Services adds outpatient and inpatient facility coding services to its coding and compliance portfolio of services.
- CommVault enhances its PartnerAdvantage program for channel partners to accelerate revenue growth and simplify collaboration.
- Quest Diagnostics acquires the remainder of Steward Health Care System’s (MA) outreach laboratory services operations and will provide testing services to providers previously serviced by Steward.
- iHT2 posts highlights from its Atlanta Health IT Summit.
- Imprivata hosts its HealthCon 2014 conference May 4-6 in Boston.
- Aspen Advisors shares a white paper on building a technology roadmap to support an organization’s value-based model.
- Orion Health and two of its customers will discuss how state public health agencies can expand the use of integration engines to prepare for quality reporting during the Public Health Informatics Conference April 29-30 in Atlanta.
- Health Catalyst opens registration for the 2014 Healthcare Analytics Summit September 24-25 in Salt Lake City.
- Aspen Advisor principal Jim B-Reay offers tips for keeping the mind fresh in CHIME’s CIO Connection.
EPtalk – by Dr. Jayne
I caught up with one of my medical school buddies this week as she was passing through town on the way to the class reunion that I’m skipping. She’s a primary care doc turned informaticist as well, so the opportunity to talk shop with someone who has walked a mile in the same virtual shoes as me was exciting. We got to chatting about the Flip the Clinic initiative which aims to “re-imagine the medical encounter between patients and care providers.”
The website has a variety of information on “flips” in categories like communication, design, education, empowerment, etc. The idea is that by making the clinical interaction better, patients will be healthier and providers happier. Although I like the idea it’s a little hard to get on board without some objective evidence that these interventions will make a difference. Some of them are straightforward: reducing noise in the healthcare environment, or removing physical barriers between patients and the office staff. Others are more abstract such as reforming the broken payment system. I think it’s great to have a discussion but I’m not seeing how some of these concepts will translate into practice, especially for those of us who are in employed models.
My former classmate and I have both struggled with being employed physicians and our inability to get buy-in from administrators when we want to try innovative maneuvers. Administrators frequently want proof that we’ll have positive return on investment but fail to realize not all returns are monetary. It’s difficult to try to find energy to fight the status quo when all the forces surrounding us (MU, CMS, HIPAA, and the rest of the alphabet soup) seem designed to stifle any attempt to think outside the box.
It’s going to take more than concerned individuals to truly Flip the Clinic. Organizations will need to address culture issues and there will need to be institutional buy-in before change can begin. The commitment needed to actually have that level of change take place, let alone “stick” and become hard-wired is something that very few of us can muster right now.
From Demo Dave: “Re: replacement systems. I sold EHR systems to physician groups for 15 years, all before MU started to skew the market. At least 30-35 percent of the systems I sold were to practices looking for additional functionality that was already in their existing system. These practices simply never learned to utilize the capabilities of their existing systems. When an administrator told me their existing EHR was lacking functionality or reporting, I simply smiled and confirmed what they wanted in a new system. I then focused demonstrations and implementations to meet their needs.” Many EHRs have gotten to the point where they have more features than users can understand let alone incorporate on a daily basis. Anyone who thinks they can learn a system with a few days of training and never think about it again is woefully shortsighted. Having workflow validation and optimization visits at 30, 60, and 90 days post go-live can help – any bad habits can be corrected and new features can be regularly introduced to those users who are ready for them. Customers should also consider actually reading the user manual and other documentation before they throw the proverbial baby out with the bath water.
Most of our readers know I enjoy a good cocktail and also love to travel, so I was intrigued by a story on NPR that talked about powdered liquor. I should have read it right away rather than bookmarking it for later – when I returned it had been updated stating it’s not actually legal in the US. Apparently I’ll have to go to Japan, Germany, or the Netherlands to check out the options.
Speaking of the need for a stiff drink, there’s still a fair amount of chatter about the release of the Medicare payment data. The newest Coda-a-Palooza challenge calls for developers to leverage that data to “help consumers improve their health care decision-making.” I’m a professional, I understand what the Medicare data does and does not reflect, yet I still struggle to think of ways that the data can be useful in consumer decision-making. The site says the data “shed significant light on how physicians actually work.” Excuse me? How does data on Medicare payments explain how I care for patients? Maybe I’ll understand better in June when the winners are announced. In the mean time, any explanations that you can send my feeble post-call brain?
Email me.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre
More news: HIStalk Practice, HIStalk Connect.



































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…