Keith Neilson is CEO and co-founder of Craneware of Edinburgh, Scotland.

Tell me about yourself and the company.
I was born in Edinburgh, Scotland and live there to this day. My background was in physics. I was very poor at physics, so I migrated into computers and computer science and around those areas from sales and marketing positions, but also technical and development positions.
In 1999, along with my co-founder Gordon Craig, we decided to form a software company. We met a healthcare consultant based in New Jersey called Nora McNeil, whose company did charge master management for a large proportion of the New Jersey and New York hospitals. We partnered with her to write some software to produce the first automated charge master solution in the marketplace.
It must have been tough to get those first customers to sign on with a company located outside of the United States. What was your story that led them to have that confidence?
In the early days, we were selling through the consultancy company. It was an extension to the services that the consulting company was providing.
We started to develop our own direct sales force and direct sales after probably about the first year or so and started to move through from there. In the first year, it was all through Nora McNeil’s consulting company. We were writing software that her consultants were then using out in the field.
How many employees does the company have and how many of those are in the United States?
We’re about 220 in total, of which I think about 130 or 140 are in the US.
What are the key revenue cycle issues that hospitals are struggling with?
We started in charge master. I still believe that’s an untapped asset in many hospitals. The charge master is a valuable control point within their hospital operations.
We’ve widened towards a more transactional basis. We have transactional software that deals with claims generation, claims processing, and denials management. We have some RAC audit software in there as well and third-party payer audit software. At the front end, we’re starting to move more into patient access and into the consumerization of healthcare.
There’s probably three, maybe four areas that hospitals should be looking at. One is around, are they billing correctly and getting everything that they’re entitled to? Because they should be. Future revenues will be based upon their success in doing that currently, and equally we know that revenues are going to get tighter in the future. It’s going to be proportioned in different ways with the Affordable Care Act and different areas from there.
Hospitals should also be considering their cost base and looking at their supply side and their supply chain and whether they’re getting value out of that.
The data that’s flowing through the revenue cycle, whether they’re capturing that and whether they’re utilizing that to the best value.
Lastly, it’s the consolidation trend. How do you manage? If you’re a consolidator, how do you get value out of the hospitals that you’re buying or the facilities that you’re buying to be able to achieve the economies of scale that people are looking for? Equally on the other side, if you are being acquired, how do you manage to continue to provide quality of care within your community and provide your mission and your needs from there?
To me, those are the four things that are going to be the biggest challenges going forward.
How do you see the supply chain systems market shaking out given that many hospitals bought ERP systems but don’t seem to be getting the value from them they expected?
I think hospitals are probably getting exactly what they need from some of these systems — or certainly have the ability to get exactly what they need from them — which is very, very good quality stock management systems. In the healthcare environment, though, more uniquely than many other environments, supplies and pharmacy have to be tracked in a different way. Equally, they are billed in a different way because they are typically billed independently — or at least recorded independently — and in high volumes. It’s very different from many other industries.
If we take the car manufacturing industry, the car is the sum of many different parts. It is recorded within the ERP system as being the sum of many parts. But they don’t bill that way. They don’t claim that money back. They don’t get reimbursed on the individual parts. They get reimbursed on the car in its entirety.
In healthcare, that’s not the case, and I believe certainly for the foreseeable future that will not be the case. You’ll still need to have detailed out what drugs, what supplies are actually going in, for both a health and safety perspective of knowing where supplies and drugs have been administered, implantable devices, those kind of things. But also just from an accountability perspective, were they actually supplied to the patient? Did the patient actually consume them? Were they medically necessary?
Also record details of them from a perspective of trying to drive future cost savings in healthcare by understanding the use of implantable devices, new med tech as it’s coming through, general supplies, but also both the current wave of pharmaceuticals and the new wave of smarter pharmaceuticals that are coming through as well so that people can learn from that.
Supply chain is quite a critical area for hospitals. I think the latest statistics I saw from American Hospital Association was that up to about a third of costs come from supplies and pharmaceuticals for hospitals. That drives directly to reimbursement as well because many of these things are on very thin margins and many hospitals are running very thin margins. That’s a significant amount of spend that I don’t think gets enough attention both from a financial and from a data perspective at this stage.
You mentioned getting paid for the components of a car rather than the whole car, but new payment models push more toward getting paid for the car. How do you think that will change your business?
On the surface, we’ll look at individual payments there. I would be very surprised if people don’t still want the detail and the data underneath.
If we are moving to electronic health records with a purpose of better understanding the patient interaction so that we can better anticipate cost and the need for investment in healthcare going forward, why would we go to the stage where we would then take that data and destroy that data? We’ll still need that data at a later stage.
I also think that there’s a potential that bundling ACO models were not necessarily indicating that need for data will be relatively short-lived. We already have a case just now where if we think about it, we have our DRGs, and within the DRGs, we have ambulatory payment classifications, which take over a higher level than the individual procedural codes below that. But although the individual procedural codes are not necessarily billed individually. You still have to record that you’ve carried out those individual procedures and you’ve proved the individual pharmaceuticals supplied down to the patient so that people know that they’re getting value and they’re getting the full treatment.
I think we’ll have a similar thing with bundled payments and in the ACO model. I don’t think that level of detail will disappear from underneath. It actually will become more critical as we go forward. The genie’s out of the bottle.
If we go to Volkswagen, although they sell one car, they don’t record all the data and all the component parts of that car and just say, well, that’s a Volkswagen Beetle. They look at all the individual components and have them all listed and have a full understanding of what the cost implication of supplying part A or supplying part B is to make up a brake caliper.
From there, I think that level of detail is only going to increase underneath. And of course, with ICD-10, potentially ICD-11 — whenever that rolls out to bring coding in line with the rest of the world — you’re increasing that level of detail again.
The company has talked about acquisitions for some time. You’re publicly traded. You have a big footprint, with a fourth of US hospitals as customers. What are you looking for in terms of potential acquisitions, especially with regard to analytics?
Certainly from a data perspective, we believe that we should be continuing to invest in our internal data platforms to be able to take the information that we gather and build that into better products. That’s been a longstanding commitment from us to do that. In fact, we’ve had tools in that marketplace since I want to say 2005, but what we’ve tended to do is roll them into our other products rather than have them as standalone.
Part of the reason for that is that analytics themselves, I believe, are becoming more and more of a commoditized marketplace. You can buy off the shelf a whole series of Microsoft tools that even four years ago, we couldn’t have dreamt we would have had that kind of analysis ability at our fingertips. I think the actual analysis itself will become more and more commoditized.
Where I think we need to focus more of our efforts as an organization – and where I believe our customers are focusing and starting to look — is more of the content that goes alongside that to make those analytics intelligent. A combination of both predictive analytics, truly looking at how we can model the future to try and get an understanding of today and current short-term performance as well as long-term performance. How do we do that with predictive analytics?
But also looking at content and value add of, what do those analytics actually tell you? If you’ve got this traffic light, what does it really mean? How do you improve the performance of your operations with the ultimate aim of then improving patient care? What’s the thing or the 10 things that make the difference to improve that patient care and do that in an environment where you can afford to be able to do that?
That’s the bit that we’re trying to concentrate on more of. That’s what you see as quite a common theme throughout our products. It’s about applying that intelligence and doing more than just providing the tools, but providing some of the structure and some of the workflow in that as well. If you do highlight a problem, how you can correct that and manage it through?
How do you see the future playing out in terms of acquisitions?
We’ve made it quite clear and been quite public that we continue to look for acquisition opportunities that extend the range of our product set or augment the range of our product set. Particularly in our supply chain side of things, particularly in patient access. We’ve got some very good products in there, but we don’t have what we would call a gateway product in there, a product that’s strong enough as a standalone elite product that we can take in to a brand new customer.
From there, find revenue from that, then generate more sales and provide benefit to the customer as well and incremental extra benefit to the customer. We’re looking to add into patient access, and equally, we’re looking in around revenue cycle and revenue integrity with a slant towards supplies and pharmacy. That’s where we’re looking.
We are a publicly traded company, as you said, on the London Stock Exchange. We have been successful, but we believe we can be far more successful. We believe we can do far more to help our customers and provide value to them, and therefore through that, grow our business. We’ve only just scratched the surface of that.
In the future, I certainly would see us getting that scale and building that scale through a combination of both organic growth and through acquisition. Then to be able to look at potentially becoming a public company in the US as well.
I wouldn’t say you fell by accident into becoming an entrepreneur, but it sounds like it took some turns that wouldn’t have been expected. What are the most surprising things that you’ve learned in becoming an entrepreneur and now running a publically traded company?
I think it’s fair to say I fell by accident into healthcare, definitely. [laughs] That’s something that I’ve really enjoyed and certainly haven’t regretted at all. I feel that we’re making a difference there.
From the entrepreneurial side of things, from a very early age, I’ve been writing software and selling software and doing things from there. I think what that can bring to healthcare is a very fresh approach. I think that both the combination of what we did both in 1999 and hopefully we have consistently done through today is try to tip some of those sacred cows over. Trying to look at healthcare as an organization and trying to understand where the differences are between healthcare and other industries and how we can bridge those gaps, predominantly how we can bridge those gaps with technology.
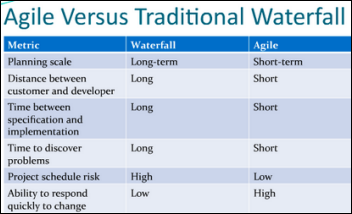
We’ve been very much about trying to produce solutions which are easy to implement and easy to roll out for our clients and give them maximum benefit as quickly as possible.
I’m not sure if I answered your question. The lessons are being able to be dynamic in terms of your approach, being able to be flexible to the circumstances and the changing legislative landscape. But also being able to put those changes into context and look at them over the long term rather than just over short term. By short term, even cycles of two or three years, and trying to look at cycles of five and 10 years and see how we can have long-term sustainability.
Those are some of the things learned through the course of this journey and my previous work, but particularly are relative for healthcare just now.
Do you have any final thoughts?
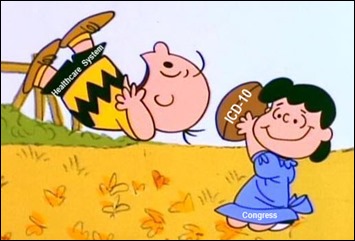
I know that many of your readers will be potentially very frustrated with some of the changes that are coming through with the Affordable Care Act and some of the uncertainties that come with whether ICD-10 is coming in this year or next year and all the various different vagaries of that.
But underlying, healthcare in the US has the potential to be absolutely phenomenal. There is wastage there. There are areas that can be improved. But there are areas that can be measurably improved within the resource bands that are there just now. That sometimes gets lost in the noise.
We talk about ACOs and we think, OK, everyone’s going to be an ACO. Actually, that’s probably not going to be the case. We talk about, everyone’s going to be driven by these quality measures and it’s going to be quality or everyone’s going to be affected by just having bundled payments. Actually, that’s probably not going to be the case.
What’s most likely going to happen is most facilities are going to claim and be reimbursed through a variety of different models. What they need to do is very calmly and rationally think through what the data implications of that are going to be. What data can they influence? What data do they need? What tools to be able to help understand and analyze and correct?
There are tools being generated just now. We’ve seen a huge change in even just the last two or three years with the software that’s available and the adoption of software within facilities. I think the next two or three years and beyond that will have equally aggressive change coming forward. A lot of that will be for the better.
There tends to be a big despondency and malaise out there, but actually things are turning out not quite as bad as people were expecting. I think a little bit of optimism should be there.
Comments Off on HIStalk Interviews Keith Neilson, CEO, Craneware





















































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…