Neither of those sound like good news for Oracle Health. After the lofty proclamations of the last couple years. still…
News 5/31/13
A letter to the editor in The New York Times by National Coordinator Farzad Mostashari says public policy is making the healthcare system smarter, citing the recently announced figures that half of practicing physicians and 80 percent of hospitals are using EHRs.
HIStalk Announcements and Requests
![]() Some HIStalk Practice highlights from the last week or so: WNA makes a rare HIStalk Practice appearance to comment on a physician who has quit taking insurance. Physician satisfaction with their EHR vendors has declined over the last year. Almost one-third of physicians buying EHRs today are replacing legacy EHRs. Physicians fear that declining reimbursements, rising costs, and ACA-related requirements will threaten practice profitability. Athenahealth recognizes Midland Orthopaedics with its athenaVision award. Most nurse practitioners believe a practice led by an NP should be certified as a PCMH, but most physicians disagree. Dr. Gregg posts a letter to Allscripts. Thanks for reading.
Some HIStalk Practice highlights from the last week or so: WNA makes a rare HIStalk Practice appearance to comment on a physician who has quit taking insurance. Physician satisfaction with their EHR vendors has declined over the last year. Almost one-third of physicians buying EHRs today are replacing legacy EHRs. Physicians fear that declining reimbursements, rising costs, and ACA-related requirements will threaten practice profitability. Athenahealth recognizes Midland Orthopaedics with its athenaVision award. Most nurse practitioners believe a practice led by an NP should be certified as a PCMH, but most physicians disagree. Dr. Gregg posts a letter to Allscripts. Thanks for reading.
We’ve had some interesting posts on HIStalk Connect lately, so you might want to sign up for e-mail updates if you follow mHealth, innovative technology, and startups. Lt. Dan also does a Friday weekly news recap there that provides a great summary. Some recent articles:
Tim Cook Discusses Wearables, Acquisitions, and Executive Changes at D11 Conference
The Third Screen Revolution in Healthcare Is Before Us
How Consumers Enter the System
EHRs Propagate “Best” Practices
Healthcare Q&A
VentureHealth Launches Equity Backed Crowd Funding Site
Texting for Health Revisited
Acquisitions, Funding, Business, and Stock
Shareable Ink raises an additional $3 million, bringing its total funding in the last three years to over $14 million.
Sales
Bon Secours Health System Center for Clinical Excellence and Innovation selects Quantros to advise on performance improvements to advance ED quality and safety.
Southpoint Surgery Center (FL) selects Wolters Kluwer Health’s ProVation MD and ProVation MultiCaregiver.
The Pennsylvania eHealth Partnership Authority signs a five-year agreement with Truven Health Analytics for its HIE solution.
Clyo Internal Medicine (OH) selects simplifyMD as its EHR provider.
The University of Miami and the University of Miami Health System will deploy Hyland Software’s OnBase enterprise content management solution across 60 academic departments, 30 outpatient facilities, and three hospitals.
John C. Lincoln Health Network (AZ) selects Besler Consulting to assist in the identification of Medicare Transfer DRG underpayments.
People
AirStrip names OptumInsight CEO Bill Miller to its board.
Verisk Health EVP Brian Smith joins the advisory board for telemedicine provider SnapMD.
Explorys appoints Cleveland Clinic CFO Steve Glass to its board.
Announcements and Implementations
Advocate Physician Partners (IL), a care management collaboration with Advocate Health Care, implements its 500th independent physician on SynAPPs, Advocate’s cloud-based version of eClinicalWorks EHR.
Practice Fusion announces preferred billing partnerships with ADP AdvancedMD, CollaborateMD, and NueMD.
The Idaho Health Data Exchange and St. Luke’s Health System launch Image Exchange viewing capabilities by eHealth Technologies.
Malcom Randall VA Medical Center (FL) installs Welch Allyn’s Connex Electronics Vitals Documentation System.
Edward Hospital & Health Services (IL) deploys Levi, Ray & Shoup’s VPSX print management and document delivery system its Epic system.
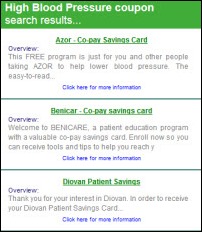
PDR Network will distribute drug company patient support coupons from OPTIMIZERx via EHRs.
SCI Solutions releases Order Facilitator v10, which includes mobile ordering, expanded messaging, and enhanced capabilities for lab order requisitioning, collection, and labeling.
Nuance publicly confirms for the first time that its speech recognition technology powers Apple’s Siri, with CEO Paul Ricci stating at a conference, “We are the fundamental provider of voice recognition for Apple.”
In England,NHS chooses BJSS and Valtech as finalists to develop an electronic referrals service to replace Cerner’s system.
The MUSE conference is underway this week in National Harbor, MD, wrapping up Friday. The photo above of Farzad Mostashari delivering the keynote was posted to Twitter by Dan McQueen.
CureMD will demonstrate a new chemotherapy administration module of its oncology EHR that it says took five years to develop next week at the American Society of Clinical Oncologists conference in Chicago.
Government and Politics
CMS advises practices on the role of clearinghouses in the ICD-10 transition, noting that, “While clearinghouses can help, they cannot provide the same level of support for the ICD-10 transition as they did for the Version 5010 upgrade.”
The HHS Office of Inspector General finds that healthcare provider information maintained in the National Plan and Provider Enumeration System (NPPES) and Provider Enrollment, Chain and Ownership System (PECOS) was often inaccurate, occasionally incomplete, and generally inconsistent between the two databases. In NPPES, 48 percent of records contained inaccurate data; 58 percent of PECOS records contained inaccuracies.
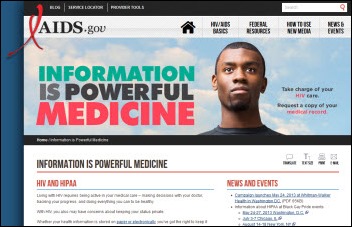
HHS launches the “Information is Powerful Medicine” campaign that targets HIV/AIDS sufferers.
A group of Senate Republicans calls for an independent investigation of HHS Secretary Kathleen Sebelius, claiming that her fundraising efforts for Enroll America, a non-profit that promotes the Affordable Care Act, is inappropriate and possibly illegal in appearing to solicit donations from industries she is responsible for regulating.
Other
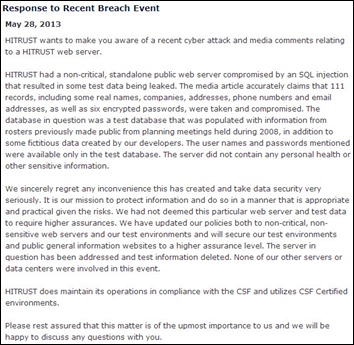
The Health Information Trust Alliance, which promotes data security among healthcare providers, experiences a cyber attack of a non-critical, standalone public Web server. HITRUST a test database with fictitious data was compromised.
Bon Secours Hampton Roads Health System notifies 5,000 patients of a potential EHR security breach after discovering that two clinicians had accessed patients’ medical records “in a manner that was inconsistent with their job functions and hospital procedures.” The hospital has terminated the pair and is offering affected patients free credit monitoring services.
In England, Royal Berkshire Hospital says its problem-plagued Cerner Millennium EPR forced it to write down $23 million. According to the hospital’s CEO, “Unfortunately, implementing the EPR system has at times been a difficult process and we acknowledge that we did not fully appreciate the challenges and resources required in a number of areas.”
Australian researchers review the use of CSC and Cerner CPOE systems in a small-scale study that suggests systems with more drop-down menus may increase error risk.
EMR reminders driven by a connection to New York City’s vaccine registry increased children’s flu vaccine rates by 9 percent, and when physicians chose not to order the vaccine, they documented the reason 98 percent of the time. The results were presented at a pediatrics conference earlier this month.
Despite performance challenges with Meditech 6.0, 95 percent of the company’s customers surveyed by KLAS say Meditech is part of their long-term plans, citing affordability and usability.
A New York Times article says Beth Israel Medical Center (NY) allowed an elderly heiress worth $300 million to occupy one of its rooms for the last 20 years of her life, but launched “an all-out fundraising campaign” in having executives hang around her room to hit her up for donations and drop hints about making a will. The CEO’s mother even watched a Smurfs video with her hoping to get on her good side.
Weird News Andy titles this story Step 1: Insert Pencil. A German man complaining of headaches and a runny nose is found to have a four-inch pencil embedded in his head, lodged there 15 years previously in a childhood accident.
Sponsor Updates
- SIIM and Brad Levin of Visage Imaging have developed a three-minute survey for IT imaging leaders to bring visibility to imaging challenges before next week’s SIIM13 conference in Dallas.
- Dorland Health names Vocera subsidiary ExperiaHealth the winner of its Case in Point Platinum Award for Discharge Planning Program for its use at Cullman Regional Medical Center (AL).
- RazorInsights exhibits its ONE Enterprise EHR at next week’s Alabama-Georgia Rural Health Clinic Conference in Opelika, AL.
- SuccessEHS client ARCare (KY/AR) achieves Stage 6 on the HIMSS Analytics EMR Adoption Model.
- Imprivata announces that it has the highest market share of any SSO solution among US Meditech EHR hospitals (36 percent) and that the number of hospitals using Imprivata OneSign has increased about 57 percent in the last year.
- e-MDs posts a Webinar that includes advice for physician practices on health information exchange and Stage 2 MU.
- Impact Advisors principal Laura Kreofsky and senior advisor Jason Fortin discuss why achieving Stage 2 MU could be challenging.
- Awarepoint is named a Red Herring Top 100 North America Tech Startup.
EPtalk – by Dr. Jayne
ICA achieves EHNAC Accreditation as a Direct Trusted Agent. Other vendors recognized include Cerner, Max.MD, and Surescripts. All four were accredited for Registration Authority, Certificate Authority, and Health Information Service Provider criteria.
The HIMSS14 Call for Proposals ends next week. It’s hard to submit timely topics nearly a year in advance, but if you’re like those of us in the nonprofit trenches, it may be the only way to have a trip to HIMSS approved. You wouldn’t want to miss an opportunity to attend HIStalkapalooza, would you?
Speaking of educational opportunities, CMS offers a National Provider Call on June 5 to help providers get started with PQRS and the Value-Based Payment Modifier programs. CMS experts will also be available after the presentation to answer questions.
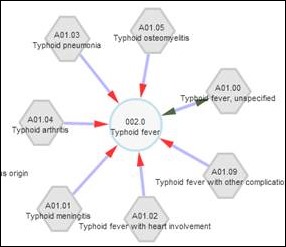
The University of Illinois at Chicago creates an ICD-9 to ICD-10 website. Maybe I have a warped sense of fun, but I enjoyed fiddling with it, and the results make for some frightening diagrams to spice up ICD-10 presentations.
A friend of mine e-mailed this blog by Reid Blackwelder MD, president-elect of the American Academy of Family Physicians. He tells the tale of a neighbor who fell and was taken to the ER where he was possibly misdiagnosed and discharged, then had to return for more extensive testing and a final diagnosis. Along the way, key clinical signs (like his inability to walk) were missed. Treating the numbers (test/lab/film) rather than the patient has become epidemic in the US. Is it defensive medicine, time pressure, the influence of Big Data, or simple lack of caring? I don’t know the answer, but we have to figure out a way to do better.
The article came at the same time that I was having a heated e-mail exchange with an IT colleague about whether we should push our vendor to incorporate genomics content in the EHR. I find it difficult to think that the average physician is going to be able to understand and act on genomic data when our healthcare delivery system so stressed that stories like Dr. Blackwelder’s exist. Of course that’s assuming we figure out a way to pay for gene sequencing and the subsequent treatments suggested by the data, which was the source of the original heated exchange.
Contacts
Mr. H, Inga, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis.
More news: HIStalk Practice, HIStalk Connect.

















At the same time @farzad_onc is in his glory seeing his letter at the top of NYTimes Op bestowing his notion of the virtues of HIT, FDASIA is meeting on the risks of MDDS, CPOE, and CDS that require that these devices be regulated:
https://www.federalregister.gov/articles/2013/05/30/2013-12817/food-and-drug-administration-safety-and-innovation-act-fdasia-request-for-comments-on-the
There is a public comment period also. Did I miss this in earlier HIStalk News?
RE: NY Times letter to editor by FM – it’s interesting that we just take it as gospel that EHR use is a good thing on the scale of national impact to healthcare. I’m pretty sure I agree or at least wouldn’t make this point without anonymity for fear of being laughed out of healthcare, but I’ve seen no data that supports the nearly universally held belief that this represents any kind of significant upgrade to the overall healthcare system in the United States.
If it is SO true, the benefits would be obvious and measureable. I see small measurements that are very positive regarding patient safety and there is always the PROMISE or POTENTIAL of data consolidation making everything more efficient, but the reflexive belief in EHR adoption increases being obviously positive would objectively suggest that there are significantly positive measureable improvements – in other words, if it’s so good, what are the results? And so far the reason for EHR adoption being a positive thing is that EHR adoption is increasing – in other words, it must be good because everyone is doing it. OK, I guess, but maybe we could just a good dose of skepticism here too. Maybe it’s just software that makes the widgets easier to produce – and if that’s the case, it’s going to take a hell of a lot more than that to make a dent in healthcare in the United States.
I guess I just want to know we (as an industry) are focusing on the right things – maybe EHR adoption will make a hospital or shared services healthcare system more efficient, but will that definitely positively influence healthcare in the United States? By itself? I doubt it…
I’m with Flunky on this one. To make the grand leap from EHR adoption, which is actually a relatively new phenomenon to it improving healthcare delivery is a stretch to say the least. And there are plenty of studies to support and detract from the true value EHRs provide in the context of care delivery and outcomes.
I am a strong proponent of the effective deployment and use of HIT as I firmly believe that ultimately it will make a very valuable contribution to improving care delivery but we are quite a ways out before that will be fully realized nationwide.
Does Nuance’s CEO really not know the difference between voice recognition and speech recognition, or is he misquoted above?
People continue to say “EMRs are a new phenomenon” or claim to be “pioneers” believing the industry started with them. Those of us who happily used one in the 1970s and since say “not so” but to no avail.
If people said “TV is new technology” and claimed to be pioneers when they got their first TV set, everyone would laugh. Yet that’s exactly what’s happened with EMRs. Yes, after an incredible start with REAL pioneers, adoption was been limited. Newcomers would be wise to ask why, not deny history.
The Battelle study in mid 1970s clearly laid out benefits of even a non-interoperable well designed EMR IMPLEMENTED WITH EXECUTIVE AND CLINICAL LEADERSHIP and PROCESS REDESIGN. The additional benefits of interoperable systems can clearly be significant and should be obvious, but the payment and delivery systems need to be fully reformed to realize them. And people need to realize it’s THEM that has as much to do with benefits as a system.
Let’s deal with the industry record of poorly designed SW and lack of executive leadership. To continue to doubt benefits can be realized or presume we shouldn’t automate one of the most complex and data intensive industries defies belief. No, you can’t slam in bad software and see benefits come out the back end.
Sorry, but it’s Groundhog Day all the time in HIT.