Top News

ONC announces that Chief Privacy Officer Joy Pritts, JD has resigned after four years on the job.
Reader Comments
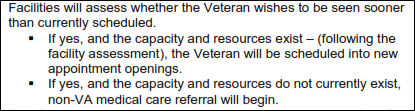
From Anonymous Tipster: “Re: Wayne Tracy on VistA. I agree it would be a tragic shame to see VistA replaced. Unless Epic were to make some dramatic changes in its approach to interoperability, this could be a disaster for the VA. Anyone who has ever suffered through a migration to Epic could tell you how difficult this can be from a workflow perspective (not to mention cost overruns). You think there’s backlog now? Remember the iEHR project that died? It’s an election year and the money is rolling in big time from lobbyists — maybe Epic will even begin to divert some of its campaign dollars to Republicans).” The DoD’s IT efforts have been financial disasters, with AHTLA and its predecessors rumored to have cost $10 billion. The VA has done very well with VistA, but its more recent efforts involving government contractors (BearingPoint’s CoreFLS at Bay Pines) were spectacular failures, so there’s no guarantee that VistA wasn’t a one-trick pony. It’s also true that DoD and VA don’t agree on anything despite their common responsibility in caring for active service members who eventually (hopefully) become veterans. Kaiser had to pull the plug on its IBM-developed system that cost hundreds of millions of dollars and replace it with $4 billion or so worth of Epic, so that’s an interesting IBM-Epic partnership (I can’t imagine Epic letting IBM tell its 25-year-olds how to implement.) Add replacing VistA to DoD’s $11 billion project and you’re probably talking about $30 billion worth of overruns, delays, and potential patient harm as the VA and DoD are forced to smoke their first-ever HIT peace pipe – that number has substance since the DoD walked away from iEHR because it was going to cost $28 billion and nothing involving the federal government ever comes in on budget, especially if the military is involved. Britain’s failed NPfIT has been called one of the most expensive government IT projects in history at around $17 billion, so we’ll beat that for sure. One final thought: Epic’s Judy Faulkner and InterSystems’ Terry Ragon are already healthcare billionaires as sole owners of their hugely successful private companies — an IBM-Epic DoD deal would certainly raise the numeric placeholder in front of their billions.

From Expandable Beltway: “Re: DoD bid. Cerner is teamed up with Accenture.” Unverified. I am getting anxious to hear what Dim-Sum has to say. Lorre would love to get him or her to present a webinar on the DHMSM topic, for which I would even arrange one of those voice-changing gadgets.

From Cool Runnings: “Re: Benefis EHR RFI. They use Meditech inpatient and replaced LSS with NextGen a few years ago. NextGen is taking a hit in Montana – a small hospital sued them, Bozeman Deaconess is rumored to be switching from Meditech/NextGen to Epic, and Community Medical Center in Missoula is merging with Billings Clinic, which very likely means a move from NextGen to Cerner Ambulatory. I’ve heard that Benefis is talking to athena, but may be leaning toward looking for an integrated solution instead of just an ambulatory switch.” Unverified, but I should have checked Meditech’s online customer list, which would have told me that Benefis runs its soon-to-be-gone systems.
HIStalk Announcements and Requests
It’s time to say goodbye to Inga, who has moved on to greener pastures after seven years of contributing to HIStalk and HIStalk Practice. She finished working on the sites in April and has finally tied up her last loose ends. Rumors that she is launching a healthcare shoe division of Christian Louboutin may or may not be unfounded, but we will wish her well in any case. Jennifer Dennard took over writing HIStalk Practice several weeks ago, while Lorre is happily handling the non-writing HIStalk chores.
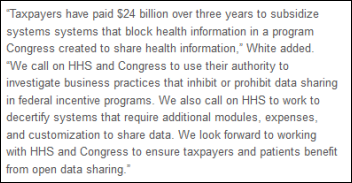
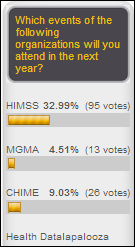
This week on HIStalk Practice: ONC’s 10-year vision statement on interoperability prompts CommonWell to up its game. Several trade associations line up with telemedicine-related requests for new HHS head Sylvia Burwell. ARcare receives the HIMSS Analytics Stage 7 Ambulatory Award. Epocrates ranks number one again. HIT Policy Committee meeting numbers show $24 billion in MU incentive payments so far. Jim Morrow, MD gives healthcare IT its due as an independent physician. Wesley Medical Center docs face employment ultimatums. Northern Virginia launches the HeaLiXVA HIE. Thanks for reading.
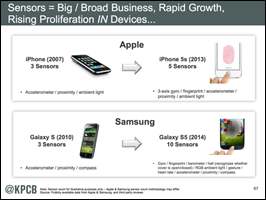
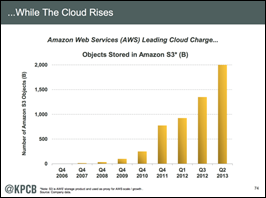
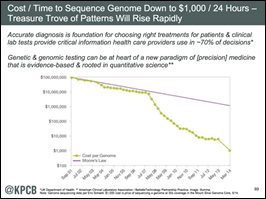
This week on HIStalk Connect: Dr. Travis discusses the concept of patient ownership of health data, its benefit to public health in general, and the role that Apple and Samsung will play in advancing the concept. ZocDoc expands its business model to include corporate wellness services. Autism Speaks signs a deal with Google to create a database that will store 10,000 fully sequenced genomes in the cloud, where researchers across the globe can access the data.
Upcoming Webinars
June 24 (Tuesday) noon ET. Innovations in Radiology Workflow Through Cloud-Based Speech Recognition. Sponsored by nVoq. Presenters: David Cohen, MD, medical director, Teleradiology Specialists; Chad Hiner, RN, MS, director of healthcare industry solutions, nVoq. Radiologists – teleradiologists in particular – must navigate multiple complex RIS and PACS applications while maintaining high throughput. Dr. Cohen will describe how his practice is using voice-enabled workflow to improve provider efficiency, productivity, and satisfaction and how the technology will impact evolving telehealth specialties such as telecardiology.
June 24 (Tuesday) 2:00 p.m. ET. Share the Road: Driving EHR Contracts to Good Compromises. Sponsored by HIStalk. Presenter: Steve Blumenthal, business and corporate law attorney, Bone McAllester Norton PLLC of Nashville, TN. We think of EHR contracts like buying a car. The metaphor has is shortcomings, but at least make sure your contract isn’t equivalent to buying four wheels, an engine, and a frame that don’t work together. Steve will describe key EHR contract provisions in plain English from the viewpoint of both the vendor and customer.
June 26 (Thursday) 1:00 p.m. ET. The Role of Identity Management in Protecting Patient Health Information. Sponsored by Caradigm. Presenter: Mac McMillan, FHIMSS, CISM, co-founder and CEO of CynergisTek. Identity and access management challenges will increase as environments become more complex, users create and manage larger amounts of sensitive information, and providers become more mobile. Learn how an identity and access management program can support regulatory compliance, aid in conducting audits and investigations, and help meet user workflow requirements.
Acquisitions, Funding, Business, and Stock

Imprivata sets terms for its $75 million IPO that values the access management company at around $400 million.

KeyBanc downgrades shares of CPSI, saying that Healthland is strong in the small-hospital market and that Epic’s Community Connect program is making it a competitor there as well.

Elsevier acquires Amirsys, which offers clinical decision support and learning tools for radiology, pathology, and anatomy that will be integrated with the Elsevier Clinical Solutions suite.

Mediware acquires Harmony Information Systems, whose systems help state and local agencies track long-term care policies.
Sales

The State of Vermont signs a six-month $5.69 million contract with OptumInsight for evaluation, remediation, and operations support for its health insurance exchange.
In England, Oxford Health NHS Foundation Trust awards a five-year, multi-million pound contract to Advanced Health & Care to develop an EHR that up to 3,500 clinicians will use on iPads. Oxford Health provides services for mental health, home care, children and family, and substance abuse.

Irving, TX-based USMD chooses the population health management platform of Lightbeam Health Solutions for its ACO and other risk-based programs. I interviewed Lightbeam CEO Pat Cline three weeks ago.
People

IMDsoft names Lars-Oluf G. Nielsen (Epic) CEO.
Announcements and Implementations

Estes Park Medical Center (CO) goes live on Medhost EDIS.
UPMC (PA) will deploy 2,000 Microsoft Surface Pro 3 devices to deploy its Convergence app, which UPMC says it first tried to roll out on the iPad without success. Convergence, developed by UPMC and Caradigm, gives clinicians a single view of UPMC’s Cerner and homegrown applications and suggests and monitors compliance with clinical pathways.

Nevada, MO, Cerner’s testbed for healthy communities, gets a new playground courtesy of the company and the Nevada Parks and Recreation Department.
Government and Politics
CMS reassures taxpayers that the workers who were sleeping on the job at the call center of Serco (which has a $1.25 billion Healthcare.gov contract) are busier now that the site is actually working.
Jon Stewart makes fun of the June 9 testimony of Assistant Deputy VA Under Secretary Philip Matkovsky, in which Matkovsky says in in the deadest of deadpans, “Our scheduling system scheduled its first appointment in April of 1985. It has not changed in any appreciable manner since that date.”
It isn’t just the VA that has an appointment problems. England’s NHS backlog hits three million patients who are waiting for appointments, not even counting six trusts that couldn’t report data because of computer problems. Still, NHS squeaked by in meeting the requirement that it treat 90 percent of patients within 18 weeks. As with the VA, increasing demand could cause NHS to start missing its goals routinely.
OpenFDA was possible only because the agency used a startup’s technology to turn its document backlog into discrete data. Captricity uses a combination of optical character recognition and crowdsourcing the unreadable parts by giving human reviewers “shredded” sections so they don’t see entire Social Security numbers or full names, preserving confidentiality. Pricing runs around 15 cents per page.
Innovation and Research

Device maker Medtronic says every person will eventually want sensors implanted in their bodies that will generate data for self assessment, remote monitoring, and disease management. The company is testing a pill-sized cardiac pacemaker and has already released the Linq insertable cardiac monitor that’s the size of a AAA battery and uses cell technology for remote cardiac monitoring.
Other

Via Christi (KS) asks for patience as it tries to recover from slowdowns caused by its Cerner Millennium go-live, with one patient reporting a 12.5-hour wait to get from the ED to a bed.
A McKesson-sponsored report predicts that value-based payments will double within five years, to two-thirds of the total.

AMA approves guidelines recommending that limitations on physician payments for providing telemedicine services be removed as long as a valid patient-physician relationship has been previously established, the physician is licensed in the patient’s state and follows that state’s laws, and standards are followed the same as for in-person encounters.
CHIME and AMDIS announce an alliance in which CHIME will provide health IT support to AMDIS and AMDIS will provide physician informatics advice to CHIME. The organizations recently jointly offered the CHIME/AMDIS CMIO Boot Camp, modeled after CHIME’s longstanding CIO Boot Camp.

Georgia Regents University will host the week-long NLM Georgia Biomedical Informatics Course September 14-20 at the Brasstown Valley resort in Young Harris, GA. Applications are due July 7. The nationally known faculty will teach change agents (biomedical educators, medical administrators, faculty, and others who don’t have knowledge of the field but who can spread the word) how to apply informatics solutions such as clinical informatics, big data, and telemedicine to their delivery, research, and education challenges. Enrollment is limited and competitive since the National Library of Medicine will pay for the registration, travel, housing, and meals of those accepted.

For $2,500, you can buy a report containing a SWAG at the size of the EHR market over the next four years in which the authors clearly don’t have a clue about data precision and presentation. Either that or they are very good at estimating the market to within 0.004 percent. I don’t see them trumpeting proof of previous accuracy.
A hospital in France blames a drug delivery robot’s computer bug for sending $15 million worth of drugs to the incinerator in the past five years.
An English hospital apologizes for the death of an 11-month-old baby whose acute appendicitis was not diagnosed because the samples for ordered tests were not delivered to the lab. A Trust spokesperson said that the pathology computer system has been upgraded to flag specimens ordered but not received.

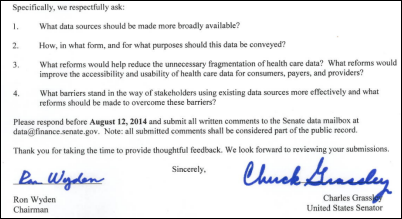
Castlight Health co-founder Giovanni Colella, MD (formerly of RelayHealth), says big data rather than government intervention is needed to fix healthcare. He recommends: (a) companies should analyze the claims data from their health plan to see what they’re paying for; (b) gag clauses prohibiting the release of price contracts between insurance companies and providers should be abolished; (c) the government should allow the private sector to use Medicare claims data and physician quality data; and (d) price, utilization, and quality data should be made publicly available in the absence of a compelling reason not to.
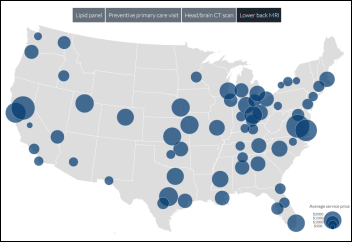
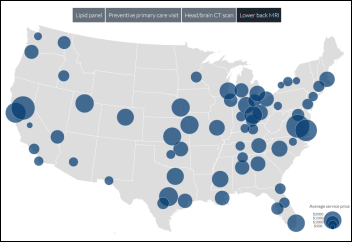
More from Castlight Health: the company releases interactive maps showing national in-network pricing for lipid panel, PCP visit, head CT, lower back MRI (above, which ranged from $676 in Fresno, CA to $2,635 in Sacramento, CA, just 171 miles away by car.)
Sponsor Updates
- Healthland will offer its hospital customers Meaningful Use Manager of Iatric Systems to help with their Meaningful Use attestation.
- Grinnel Regional Medical Center (IA) reports a seven percent increase in cash collections, 79 percent of payments made via self-service, and 124 saved hours per month in a two-year review after its go-live with Patientco’s payment automation solution.
- Impact Advisors and the Scottsdale Institute publish a report from the CIO Summit on IT Cost Management and Value Realization.
- Sixteen medical innovations were showcased at Premier, Inc.’s Innovation Celebration in San Antonio, TX this week.
- Quest Diagnostics certifies MedicsDocAssistant EHR v. 7.0 from Advanced Data Systems as a Silver Quality Solution under its Health IT Quality Solutions Program.
- Janssen Diagnostics collaborates with Halfpenny Technologies to provide specialized reporting for HIV/AIDS healthcare.
- GetWellNetwork recognizes several providers for using its solutions to improve care at GetConnected 2014 in Chicago, IL.
- Hills Health Solutions signs a distribution agreement to make Lincor’s interactive patient engagement technology available in Australia and New Zealand.
- Craneware and Centura Health (CO/KS) will co-present best practices of charge capture during HFMA ANI 2014 in Las Vegas June 24.
- InstaMed shares how its Premium Payments solution has changed the consumer payment process.
- Medfusion publishes a white paper on creating patient value through portals.
- Gartner names Covisint a Leader in Identity and Access Management as a Service.
- PeriGen CNO Rebecca Cypher will discuss fetal heart rate interpretation at AWHONN 2014 in Orlando June 14.
EPtalk by Dr. Jayne

This has been a rough week in the healthcare IT trenches. Our medical group has been in acquisition mode again, resulting in the addition of several new specialties. Unfortunately, this time around our EHR vendor doesn’t have content for any of them.
Luckily we’ve been through this enough to have a process in place. Our implementation team sends out a staffer or two to observe the practice’s current state workflow and documentation style. This is essentially a reconnaissance mission. We try to blend in and to avoid having the practice ask us a lot of questions while we gather data.
The team then comes back and makes a presentation to the implementation manager, the application team manager, and me to talk about what their current process looks like and how much we’ll be able to handle with the EHR as-is, without any additional development. Depending on the specialty, it’s hit and miss.
For example, when we added vascular surgery, we were able to handle 95 percent of their needs because we have both general surgery and cardiovascular content. On the other hand, when we’ve added certain pediatric subspecialties, we’ve had to get creative with what we choose to offer them. Vendors haven’t quite figured out that children are not just little adults and it’s not as easy as just having them use adult content with the same specialty name.
For example, pediatric cardiology deals with care for children who have had a variety of surgical procedures that are largely unspoken of in the adult cardiology world. On the flip side, there isn’t very much coronary artery disease or many triple vessel bypass surgeries among the pre-adolescent set.
Often we’re working with physicians who are used to dictating their notes and having them transcribed. We’ve had good success at putting them in our EHR “core” templates for documenting histories, assessments, and plans, but we augment the “story” part of the visit with voice recognition. It’s a hybrid approach, but it prevents us from doing costly development that will only be used by a handful of physicians. It also provides for physician satisfaction in that they’re used to being able to include a detailed narrative in their visit documentation.
We encountered a rare bird this week, however: a subspecialist who seriously believes she’s going to be happy with point-and-click documentation. She wants us to build a whole herd of custom screens for her. She dictates on the hospital system at present and has no previous experience with discrete data.
In our experience with other physicians of the same subspecialty, it’s generally not worth building custom screens. They tend to change their minds before the content is even built. If they don’t change their minds, once they see it, they decide it’s too “clicky,” and 90 percent of the time they end up dictating anyway.
We had our follow-up meeting with her today. We ran through the options and asked her to try some typical click-by-click workflows in the general medicine templates just to get a feel for what it would be like. She wasn’t terribly proficient, so we had her try voice recognition within the system. She did fairly well with that. It was clear to the team that she’ll likely do better with that kind of hybrid approach. The subspecialist was unconvinced, however.
We moved to our next tactic, which is to ask the physician to use our recommended workflow for a couple of months and then decide if we still need custom content. It was obvious that she was not buying what we were selling. She told us we were just being difficult and didn’t want to do what she asked. She then accused us of trying to skimp on her content for budgetary reasons.
We explained the history with other physicians in her specialty, even trying to show her the content we had previously built that her peers had abandoned. She didn’t want to see that either, but made it completely clear that she expected us to build custom content for her alone. I knew we weren’t going to win this discussion, so we agreed to go back to the office, brainstorm other solutions, then meet up in a few weeks.
In debriefing with the team in the car, we’re not sure what to do for her. We have more than a decade of experience doing this. We know what works and what doesn’t work. However, we have a physician with no EHR experience (and no track record as an end user – she won’t even use the hospital system) who is demanding a certain course of action. My team asked what we should do.
My thoughts went into doctor mode. It feels like the scenario where a patient is demanding an antibiotic where none is indicated, or insisting on a procedure that could potentially be more risky than it is worth. The patient in this case is arguing with the IT-equivalent of our professional medical opinion as to the course of care. In the medical world, we wouldn’t be bullied into doing something that is not of benefit. Not to mention that building clicky screens for a provider who has never been exposed to that documentation style is a recipe for unhappiness.
Our plan is to bring some of her soon-to-be colleagues in the same subspecialty with us to our next meeting and hope that their shared experiences will steer her in the right direction. We’d like her to make the choice herself without us having to flat out reject her request, but I’m not sure how we’ll handle it if she doesn’t start to get on board with our advice. Being new to the group, we know her level of trust of our team is low and her experience with EHR is minimal, so that seems like a logical approach.
I never like disappointing people. It’s always difficult to have those conversations with patients when you deny their requests. It’s doubly challenging when you’re dealing with a peer who might be more senior than yourself, and particularly difficult when they’re in a seemingly more prestigious subspecialty than your own.
In other parts of the physician universe, we’re also dealing with some significant Meaningful Use issues where physicians are requiring retraining and a lot of hand-holding. This was just one more thing to add to the mounting heap of stress.
I polled a couple of my CMIO peers on how they handle these situations. They didn’t have too many better answers. For all our readers on the implementation and content side, what’s your take? Is there a silver bullet solution? Email me.
Contacts
Mr. H, Jennifer, Dr. Jayne, Dr. Gregg, Lt. Dan, Dr. Travis, Lorre.
More news: HIStalk Practice, HIStalk Connect.
Get HIStalk updates.
Contact us online.
































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…