HIStalk Interviews Lou Silverman, CEO, Advanced ICU Care
Lou Silverman is chairman and CEO of Advanced ICU Care of St. Louis, MO.

Tell me about yourself and the company.
The company has been doing tele-ICU work for the past seven or eight years with clinical founders. We’ve been growing steadily ever since.
I’ve been at the company for just a little bit under a year. My experience spans healthcare IT, revenue cycle management services, and clinical services. I’ve also had some exposure via being a board member to pharmaceutical companies as well as home care companies and data and analytics companies.
What are the key issues hospitals have with delivering ICU services?
The ICU units happen to be a place where a disproportionate percentage of dollars is focused and spent. ICUs typically have the very sickest of patients for the hospitals.
The staffing in ICUs can be challenging for a number of hospitals. The ICU obviously should be staffed 24x7x365. The gold standard for staffing includes 24×7 intensivist involvement. The supply — and therefore the ability to recruit intensivists — is variable across many hospitals, many markets, and in fact many geographies.
How many hospitals meet that 24×7 intensivist monitoring standard, and of those, how many do it using a remote service?
It’s a relatively small percentage of hospitals that have the gold standard of 24x7x365 bedside intensivists. The number of hospitals that are using tele-ICU services to supplement that is growing fairly nicely, but we are still in the very early stages of adoption of tele-ICU services.
I think it’s fair to say that those hospitals that have elected to adopt tele-ICU services have developed a keen understanding of, and keen appreciation for, the benefits that accrue to a hospital across many different parameters for making that selection. Recruitment of intensivists is difficult. Retention, just by the very nature of the job, can be a little bit difficult. Some markets are far easier to recruit from than others.
In addition, just getting to uniformity of care, implementation of agreed-upon best practices … there are just many, many elements that hospitals are dealing with in their ICU.
We try to organize our thinking around focusing on outcomes, patient outcomes, implementation, and sustained use of clinical best practices. Doing all of those things in a ROI-appropriate manner.
You can group virtually all issues that hospitals face in the ICU into those one or more of those three areas. A good tele-ICU partner will help address in a compelling way each and all of those key areas.
What is the regional span or the geographical span of the services that you provide or that you could provide? Could it be a global service like radiology nighthawking with appropriate licensure?
Our company specifically is in 20 states today, but that’s just simply a nod to the fact that we’re growing and we’re adding states in a rapid way. The answer to your question from a U.S. perspective is that this is a model that would work in any state.
We focus on having U.S. board-certified, U.S. board-eligible clinicians working with and for us and with and for our partner hospitals. Historically at least, that has kept the focus of our recruitment on U.S.-based physicians.
It is fair to say that there are some small companies that are starting up in other geographies outside the U.S. and trying to get into the business. Some of those, in fact, also are using U.S. trained and board-certified clinicians to staff their operations. Historically, I’m not aware of any situations where U.S. companies are providing services to hospitals in other geographies. I am certainly aware that tele-ICU services are starting to start up in countries other than the U.S.
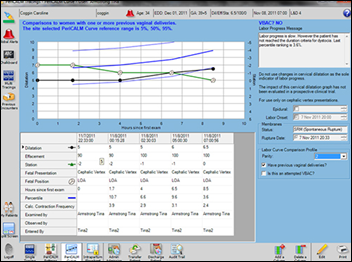
How much of the care that’s delivered to ICU patients is driven by formal protocols and accepted evidence? How does the technology take that and turn it into your service?
At a high level, the technology that we are using is driven toward having excellent access to the patients and the relevant patient health data. We have in the technology that we use algorithms that give us advanced alerts when certain patient trends are moving in a negative way. That gives us a way for us to be alerted and for us to also work in partnership with the bedside teams that we collaborate with to ensure a rapid attention to deteriorating patient conditions.
In terms of clinical best practices, that is very much a collaborative approach that we engage in with our partner hospitals. We have developed, over time and over the 60 hospitals that we have under contract, a very good understanding of what clinical best practices are and how they’re best deployed in an ICU. But it’s also fair to say that in some cases, there is perhaps more than one opinion on what the best practice is or the timing for implementing that best practice.
It is at some level not a “one size fits all” approach that we take. It is much more of a collaborative approach that we take with partner hospitals to establish an agenda of best practices that we want to collaborate and implement together. Once we have agreement on what we’re going to do and in what sequence, we work collaboratively to execute on that plan.
If a hospital has its own local intensivists but needs coverage assistance, can you do that and how is the technology used in that case?
A significant percentage of the hospitals that we partner with do in fact have some level of intensivist staffing. All of them have some level of bedside staffing. We’re not at the bedside. That’s an obvious condition of the partnership.
In terms of collaborating when there are intensivists in place, that is a regular practice for us. We are a 24x7x365 service. We provide is a robust and always-on data capture practice, where we are able to take data across all of the patients that are coming through the ICU. We are able to convert that data into actionable and informative reports that we provide to our clients and collaborate with our clients to understand exactly what’s going on with their patient flow in the ICU. How the ICU patients are faring across a variety of metrics in terms of outcomes and utilization of best practices.
That is a value-added service, even in the context of a collaboration with a hospital that has a certain number of intensivists at the bedside. ICUs historically have been not really robust in terms of the modern data that they’re able to pull on what’s going on within the ICU itself. That’s part of the service that we provide for all of our clients.
The deal that you signed recently with Adventist Health System — are they seeing results yet?
It is still relatively early days. We’ve had a very robust and on-time implementation process across all of the pilot hospitals that we have been working with at Adventist. I’m not prepared to share specific results publicly, but I can tell you that even though it is relatively early days, the returns thus far, both from a quantitative and qualitative perspective, have been extremely positive and extremely well received across all aspects of the partnership.
Do you have any final thoughts?
The whole notion of tele-ICU is a very timely idea. It’s certainly one we’re seeing increased interest as an industry. We’re seeing increased interest in us as a company.
When you look at trends that are impacting the overall healthcare ecosystem — with people having much more to do than they have time for, budgets are strained, outcomes are a clear increasing focal point — what we do as a tele-ICU provider is very consistent with all of the directional trends that are going on in healthcare, going on in hospitals, going on in the ICU. It is still an emerging market.
Our own company, without making this an advertisement, is the largest player in the space. It’s a very interesting company. The cliché is being in the right place at the right time, but it’s not a cliché for us. We are at that place at that time.













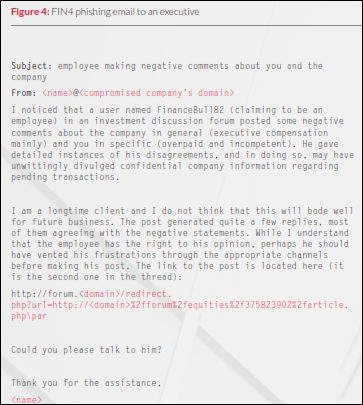




































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…