We Need Open Providers (An Alternative View on Open EHR)
By Brian Weiss

Open EHRs, Soft Drinks, and Leprechauns
Just under a year ago, having surfaced the disturbing and shocking possibility that EHR vendor marketing claims may not all be objectively measured and verified, Mr. H issued a challenge to have someone (other than EHR vendors) define what an “open” EHR really is. That call was answered by two PhDs named Sittig and Wright and a summary of their work was recently published on HIStalk.
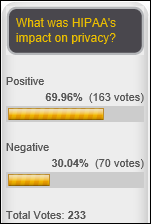
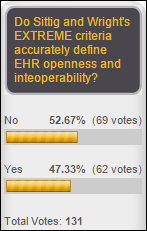
You know Mr. H must be pretty excited about something when – despite his admirable track record of correctly calling out flawed survey/study methodologies by others – he set up this week a Yes/No survey with the guidance that if you provide the answer he wants (in support of the self-declared “consensus” about what a great job Sittig and Wright did) you can just vote “yes”, but “if you vote no, it’s only fair that you click the poll’s Comments link to describe what they missed.” Since not everyone is prepared to challenge (in writing) the work of well-credentialed experts, I’m thinking that might introduce a little unintended skew into the survey results.
I think it’s always good for HIStalk when Mr. H is passionate about a subject. However, if we’re going to go after questionable marketing claims, I think it would be great if Mr. H challenged readers to draft measurable standards for claims in other industries as well. For example, what criteria must a cola beverage meet to legitimately claim to be “The Real Thing” or to “Change the Game?”
Does the DoD purchase soft drinks for its personnel? If so, maybe we can get Congress involved here as well. Granted, we probably should stick to the IT realm in general and open IT systems in particular, where the government has demonstrated a strong track record. I’m sure you have also been impressed with the government work being done on Open Personnel Management Systems, which enable a much more efficient global process on security clearances without all that redundant background checking work by multiple countries.
So, no reason to limit ourselves to health IT. I noticed that Sittig and Wright established as a must-have criteria for EHRs that, “An organization can move all its patient records to a new EHR.” Can we do that in other IT areas as well so that purchasers of all IT systems always know they can change their mind at any time? How about with cellular phone plans?
But I digress. Mr. H has earned the right to establish what it is we should be debating and defining, and if he wants us to figure out whether Goofy is or isn’t a dog, what a Leprechaun is, or what an open EHR really is, I’m there.
Send Me the Encyclopedia
I actually don’t have any issues with the specific criteria proposed by Sittig and Wright for defining the mythological creature I’ll call Nessie and they refer to as an open EHR. Even if I did, how can I argue with a summary when I can’t even begin to fathom the precise definition of most of the terms it uses? We can spend years debating what it means for an EHR to provide “role-based access,” “where data are stored and what they mean,” “controlled clinical vocabulary,” “record-locator service functionality,” “existing metadata,” “appropriate support and maintenance,” or “authorized users.” This is how Meaningful Use regulations get to be thousands of pages long.
I’m also not really sure which EHR vendors can actually submit their products for evaluation since the authors of the summary indicated that any vendor that chooses to “maintain a degree of control over access to their software for financial, security, intellectual property, and reliability reasons” can’t be considered “truly open.” And I fear some EHR vendors might fall into that category.
Again, I digress. All in all, I think the Sittig and Wright piece is a pretty good summary of conventional thinking on what constitutes an open EHR.
Welcome to our Dysfunctional Family
My issue is not with the proposed definition of what an open EHR is or isn’t. My issue is that I think we’re focused on the wrong approach to achieving our goals. Like the “National Health Network” or “Beacon HIEs” or “Interoperability Alliances” before it, debating the definition of an open EHR is like looking for a lost wallet where the lighting is best rather than where it might actually be found.
What is it we are looking for? I think Sittig and Wright say it pretty well: “… to address the needs of patients, so they can access their personal health information no matter where they receive their healthcare; clinicians, so they can provide safe and effective healthcare; researchers, so they can advance our understanding of disease and healthcare processes… and software developers, so they can… create new applications to improve the practice of medicine …”
Why is open EHR where the light (of Congress, HIStalk, and so many vendors and providers in the HIT world) is shining, but not where we can find the answer? I think Sittig and Wright started to also say that pretty well: “…in addition to having all EHRs meet these technical requirements, we must also begin addressing the myriad socio-legal barriers (e.g., lack of a unique patient identifier, information blocking, high margin fee-for-service clinical testing) to widespread health information exchange required to transform the modern EHR-enabled healthcare delivery system.”
In my view, “myriad of socio-legal barriers” is a huge understatement. EHR vendor product features (open or otherwise) are a tiny fraction of the issue. And what about all the new forms of healthcare data sources like telehealth, urgent care centers, mail-in clinical or genetic lab tests, personal monitoring devices, and everything else that isn’t an EHR (open or otherwise)?
Don’t Forget To Update Me on Progress Next Decade
What I think we are capturing in a potential Mr. H-driven consensus on the definition of an open EHR is another meaningless piece of a puzzle that, when complete, will give us a vision of what a theoretical fantasy healthcare world might look like in “one decade from now” (meaning, one decade from whenever you choose to take a look, for eternity).
I have no illusion that the people who are still reading this article are going to be convinced by what I’ve written. And even if all three of them are convinced, I don’t think that will alter the course of the ongoing Congressional hearings, ONC roadmaps, standards body committees, industry consortiums, EHR vendor leader visions, and everything else driving all the never-ending work on “legacy approaches to healthcare data interoperability.”
Plus, other than my youngest son (who is already rapidly changing his mind), does anybody else think that I know more than everyone else? Given the more qualified, more experienced, and smarter people working on this stuff, not only won’t I stop them, I really don’t want to. What if they are right and the emperor is in a stunning getup?
My plea is only this. Let’s also consider an alternative, parallel approach. One from the world I termed (in my not-academic, 20-minute study titled A Tale of Two Healthcare Worlds) “CCHIT” – consumer-centric healthcare IT.
In the few words I (really don’t) have left in this article (even my beloved three readers are now fading fast), I will now publish my definition of open EHR, and more importantly, open provider (note, Mr. H, that unlike Sittig and Wright, I don’t work for a provider, so it’s legit for me to do this one).
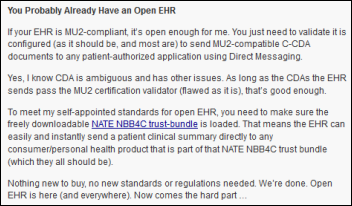
You Probably Already Have an Open EHR
If your EHR is MU2-compliant, it’s open enough for me. You just need to validate it is configured (as it should be, and most are) to send MU2-compatible C-CDA documents to any patient-authorized application using Direct Messaging.
Yes, I know CDA is ambiguous and has other issues. As long as the CDAs the EHR sends pass the MU2 certification validator (flawed as it is), that’s good enough.
To meet my self-appointed standards for open EHR, you need to make sure the freely downloadable NATE NBB4C trust-bundle is loaded. That means the EHR can easily and instantly send a patient clinical summary directly to any consumer/personal health product that is part of that NATE NBB4C trust bundle (which they all should be).
Nothing new to buy, no new standards or regulations needed. We’re done. Open EHR is here (and everywhere). Now comes the hard part …
Open Provider
To save HIStalk PhD readers the work of defining it, let’s jump straight to the certification/testing process for open provider. I now officially declare every patient in America an “Open Provider Authorized Testing Body” (OPATB). Here’s what you do:
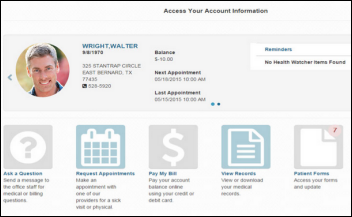
- Sign up for a free Carebox at https://carebox.it.
- Go to the “DIRECT Inbox” feature under “Import” and note your personal Direct Messaging address.
- Go to any doctor or hospital that received at least one penny in Meaningful Use money and ask them to send you your clinical summary to that address using their EHR.
OK, you don’t really have to use my product for Steps 1 and 2. There are plenty of other applications that will give you a Direct Messaging address. But since I am making up the rules here, I get to self-promote a little. Plus, mine is free right now and there’s nothing to install, so you can just ignore it after you are done with your role as an OPATB.
Here’s how you score the provider. If in less than five minutes your clinical summary shows up in Carebox, you give them an open provider certificate, a sash they can wear at next year’s HIStalkapalooza, and a big hug from me.
If they ask you to pay anything, make you fill out forms, tell you it’s a “HIPAA issue” for them (it is, but in the sense that HIPAA says they have to do this, not the other way around), send you across town to their “records department,” ask you to provide them a self-addressed stamped envelope and expect some paper records within 30 days, or anything else, you can let Dr. Halamka know that he can stop working so hard to find an “Information Blocker,” at least by my definition.
Which Brings Me Back to Cerner
Mr. H started his initial open EHR challenge last year because he was upset with something that a reader reported was stated on a Cerner conference call about how they were open and others were not. So, Mr. H probably will not be happy to learn that I’m compiling a list of open EHR vendors who support open providers, and guess who is at the top of the list?
Why? Because I got an unsolicited call from two gentlemen at Cerner (I’d be thrilled to name them, but I don’t know if they want me to) who work on Direct Messaging. They wanted to be sure that bi-directional CCD exchange between Cerner and my no-name little startup product actually works. They showed me how easy it was for any PowerChart user — as well as users of many other Cerner apps, which all come pre-enabled to “Send Direct” and pre-configured to support the NBB4C trust bundle noted above – to send any patient’s record right into their Carebox. It worked flawlessly on the first try.
Hopefully other EHR vendors will call soon or someone can tell me who I should call so I can certify them as a great open EHR for open providers to use. Because my taxpayer-funded budget for this program is a bit limited (I’m not even tax-deductible), I’ll settle for self-certification to start. Just send me an e-mail and let me know that you sent a CCD from your EHR to Carebox and it worked. No reason it shouldn’t, if you claim MU2-compatibility. If you have any issues — since I’m told EHR vendors all want to work together to advance healthcare for everyone – I’m sure if you give Cerner a call, they’ll be happy to help you out.
Now all I need to do is convince Neal Patterson of Cerner to get his wife Jeanne to trade in the “bags and bags of records” that he speaks and wrote about her needing to carry around in exchange for a Carebox. Then, in parallel to him figuring out how to get every current or future source of our healthcare data to join CommonWell (good luck!), we can unleash thousands of startups who can help all of us transform US healthcare the CCHIT way.
Are We There Yet?
Freeing up patient data so that patients can authorize the use of that data in any clinical, research, analytics, or application context they want is — in my book — “The Real Thing” and “Changes the Game.” It doesn’t help you quench your thirst (with caffeine, a possible diuretic) or get Type II diabetes, but my CCHIT startup friends and I can try to get ONC or the White House to help us spin up some committees to work on those parts.
I think all of the constituents noted in the earlier quote above from Sittig and Wright will benefit — patients, clinicians, researchers, and software developers. I think we will get “there” a whole lot faster than by following Mr. H’s prescription for “putting the screws” to EHR vendors about what they have to prove to claim they are “open.” Of course, that is going to be lots of fun, too, so we can do that as well.
One Less Study for Mankind
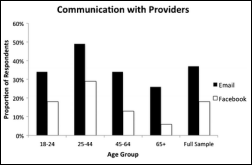
What really compelled me to write this too-long article is that just a few weeks ago, Mr. H. wrote this about patient access to their own healthcare records: “Someone should perform a study to determine the level of demand and the reasons people aren’t requesting their information.”
I started writing a snarky article (do I write any other kind?) suggesting that we go back in time and commission a study in the 1970s about why nobody wants downloadable apps from Apple on their phone (both the rotary and the newer touch-tone kind).
But then along came Sittig and Wright and the associated consensus. It occurred to me that some really smart people might already be hard at work on Mr. H’s newer study request above and I probably missed the boat on my alternative recommendation.
So before it’s too late, I want to suggest that instead of spinning up another study – not to mention all the challenges associated with the time machine and the questionable value of going back to the 1970s, if we did mine – we might all be better served if we just get open providers (who are not information blockers) to free up electronic copies of our own health data that we are all entitled to get under HIPAA Right to Access. To do that, most can use their “already open” (at the “not ideal but good enough for now” MU2-level) EHRs. Then, instead of reading more studies and articles, we can all watch in amazement what happens in months and years from now, not decades.
Brian Weiss is founder of Carebox.

























































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…