HIStalk Interviews Bill Anderson, CEO, Medhost
Bill Anderson is chairman and CEO of Medhost of Franklin, TN.

Tell me about yourself and the company.
I’ve been involved with Medhost since 2007. I was originally an investor and a board member. We’re about a $200 million revenue company with both enterprise products and population health and consumerism products.
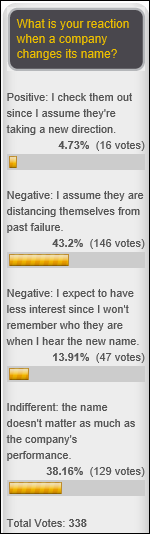
What has been the market reception following the company’s name change a little over a year ago?
We’ve acquired two different companies to go with what was originally Healthcare Management Systems. One being the original Medhost EDIS company and the second one being the Acuitec perioperative system, which was the old Vanderbilt system. Simplifying our inpatient system has been well received by the marketplace. The consolidated branding makes the company much more understandable to our customers and other constituencies.
What are the steps involved in kicking off talks about an acquisition?
We believe that we’re as much a distribution company as a technology company. The number one criterion for either buying a company or spending money internally is to try to understand what our customers’ needs are. Ideally we can anticipate those needs before they actually understand they need them.
In those two cases, for instance, these were very critical profitability centers for facilities. We believed that offering not just good enterprise departmental solutions, but best-of-breed leading solutions, was something that was going to be important to our customers. The ED and the operating room are two places they have to make money to make money. It’s really very customer driven.
You told me when we spoke last time that your main acute care enterprise competitors were McKesson Paragon and Meditech. What has changed since?
They’re both still substantial competitors. We are seeing some more competition from Cerner’s Works product, but it is in many cases more difficult to come down-market than it is to go up-market because of the complexity of the product. But largely the competition is very similar to what it was the last time we talked.
The inpatient market differentiators are usually facility size and the complexity of the app as well as the cost of buying and running these applications. How has the dynamic changed as Cerner and Epic push into smaller hospitals and large hospitals are buying their smaller competitors?
I may give you more of an answer here than you’d like. One of the things we are very concerned about is the profitability of hospitals in the middle market. Let’s say that is 50 beds to 150 beds. What has happened today is that regulations have increased the fixed costs to those facilities by mandating a lot of different systems — mostly in the IT area — and other activities. At the same time, the average revenue per customer is dropping. You see a continuous stream of news articles about the crisis in rural hospitals, particularly.
As a result, I’ve seen analysts say things like, we’re going to take 40 percent of the total facilities out of the system or 30 percent of the beds out of the system in order to get facilities to a reasonable profitability. We look at this and we say, the total cost of ownership is something that today is not only a good business practice to be conscious of, but it’s absolutely essential to the survival of these hospitals.
We’ve tried to have — and I think hospitals in general are looking for this — what I would call segment-appropriate features. Physicians, for instance, would like to have all the features you can possibly get, but the more complex the system, the more cost is added to it. We believe that total cost of ownership is a very key thing. We’ve tried to manage our systems to be able to help our customers do that.
One of the things that I always point to is that back in the mid-1980s — I used to be in the banking software business — there were about 18,000 banks in the United States. Today there are about one-third that many. If you look at the reasons that happened — increased regulations, access to capital, all those types of things — the same types of things are happening in the inpatient facility business. We’re very conscious of trying to help our facilities control costs because it’s in our self-interest to have them survive.
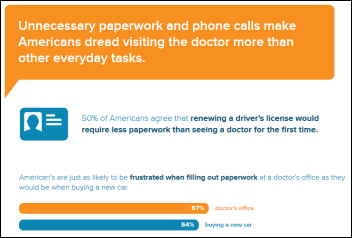
Banks invested heavily in technology to keep customers from tying up an expensive live person, such that most people now hardly ever go into the physical bank. Does healthcare have the incentives to deploy that kind of automation?
I’m not sure that you can have the same level of automation in healthcare that you have in banking with self-service. But one of the reasons we’ve heavily invested in our YourCareUniverse product suite is to help facilities manage two different digital communities, which we think are important to them — a digital community of consumers and then a digital community of providers and patients who are actually in the healthcare arena.
We think that is the analogy to the banking industry. Our facilities are going to have to learn how to manage these digital communities. It’s not going to be so much of a community-based facility as an area-based facility in the past. For instance, we have a little hospital out in Texas that covers eight counties in Texas. There’s a lot of real estate in eight counties in Texas. They need the ability to not only interact with the community, but with their patients.
The second thing we’re starting to see and having our customers tell us — particularly our big customers – is that consumerism is really starting to bite. Similar to the banking industry, you will see that things that were previously done inpatient may be moved to outpatient, whether an ambulatory surgery center or a physician’s office or some other venue outside the four walls of the hospital. Things that may have been done in a physician’s office are going to be moved out to things like MinuteClinics and urgent care offices and maybe even to self-service with the consumer, with the patient. I see very clear parallels to the banking industry.
Healthcare providers in general are saying, we’re going to be ready for this shift, because while you see it starting to happen, it’s going to take some time. The people who are preparing for that shift today, we think, are going to be the long-term winners as the market consolidates.
Are your clients confused about who their competitors and potential partners are?
It’s very challenging environment. Because of things like access to capital and the systems that are required, you see — not only in the large integrated systems, but in geographic areas — hospitals partnering up with larger facilities. You mentioned Epic moving into the smaller facilities. This is an example of how large geographic areas are handled by a large facility integrating in smaller facilities. That’s what’s happening a lot.
I think it is going to continue to be a challenge for healthcare providers to understand what the best partnership strategy will be for them. Some of these customers of ours are going to end up being purchased by other customers. Some of them are going to affiliate with ACOs or large facilities. Some of them may be in an area where they can go it alone. I don’t think there will be a single strategy because there are so many different factors involved about what the market is, the financial strength of the entity, and what the competition looks like.
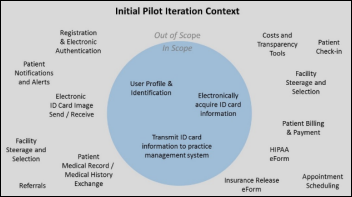
We have significant EHR adoption in the inpatient and ambulatory markets. Are post-acute care, home care, and behavioral the next frontiers in trying to move patient information from paper to electronic so that it can be shared?
Yes. We’ve got a number of really large customers and they have many different types of facilities as well as clinicians and ambulatory systems. One of our frustrations — even though we’ve built tools to help tie all those together – has been getting cooperation from other vendors. No one wants to be disintermediated away from their customer.
What is clearly the right answer for the facility and the right answer for the patient — which is to provide a totally integrated system that exchanges data and allows you to make orders and do all sorts of other things — is really very difficult to execute because there’s not alignment of economic interest there.
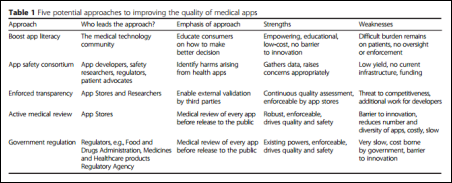
Companies ranging from tiny app developers to big enterprise companies like Salesforce are trying to figure out patient engagement. What technologies are needed and what will determine whether a vendor is successful?
We think that there will be a market evolution similar to what happened in the inpatient business. Many facilities, particularly big facilities, used a best-of-breed strategy and effectively brought components of a total system based upon individual features of that system. I think in the long run, customers are going to say — just as they are starting to say in the inpatient market, in the enterprise market — that it’s really difficult to manage a system that is cobbled together from a number of different vendors. The clear trend is a single provider for your inpatient systems.
Our approach — and what we think will be most likely to win in the long term — is that we have focused on not just having good individual components like analytics or a CRM system, but that we have a totally integrated system. That’s what the customer is going to ultimately demand.
For instance, when we did our patient portal, instead of having a tethered portal to an EHR, we built a private HIE. We’ve got both an ambulatory and an inpatient-certified Meaningful Use portal on top of that. On top of that, we have both an analytics system and a CRM system that allows you to not only track patients and all their data, but to aggregate data within a community.
Where I believe this is going to become particularly important is if in fact the Meaningful Use guidelines for view, download, transmit actually go to 25 percent. Our understanding of the regulations is that in a community, if you had information as a clinician in the hospital system and you had a single portal for both the ambulatory and inpatient providers in that community, you could effectively pool traffic. There are going to be instances where not only the market, but regulation is going to require that you have this totally integrated system, because otherwise you’re never going to get to a 25 percent view, download, and transmit standard, for instance.
What possibly unusual assumptions are you using for the company’s next five years?
Our assumptions are threefold. In the inpatient market, we believe that there are probably at least 1,000 facilities in our relevant market space — the short-term, acute-care market — that have not made durable enterprise product selections. While it is a mature market, at some point in time, as customers and the market get over the Meaningful Use trauma, they’re going to start replacing systems that are not going to meet their long-term needs or they will have a question about whether that vendor is going to be there for them five to 10 years from now. One of our assumptions is that consolidation in the vendor market — just like consolidation in the provider market — will happen sooner rather than later.
The second assumption we’ve made is that while people talk about population health, and while we have a complete population health solution, we think the most important thing is going to be addressing the consumerism needs. Specifically as more and more healthcare moves out of the inpatient setting, in order to survive as an inpatient provider, market share is going to become increasingly important. Therefore, the number one skill set that our customers don’t have today that they need to build is marketing.
We’ve started to provide tools to help them to market to the community. That includes our YourCareEverywhere content site, which is a co-branded content site. If you’ve looked at most hospital Web sites, it’s about the hospital, not about the consumer. We’re big believers in that if you’re going to engage with a consumer, you have to provide them continuous value — not just value when they’re a patient — as well as an analytical solution and a CRM solution that allows you to market to the community based on needs.
We think our focus on the consumerism side of the equation is much different than most of our competitors in the middle market.
Do you have any final thoughts?
Today I believe there is a determination being made between the facilities that are going to be survivors in consolidation and those who are not going to survive as standalone entities or even as entities at all. In many cases, unfortunately, the management of the facility does not really understand that that’s happening today. If you’re too late to address these specific issues, such as consumerism and partnering and things of that nature, it may be too late by the time you are willing to address the issues.































































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…