HIStalk Interviews Michael Pirron, CEO, Impact Makers
Michael Pirron, MBA, PMP is founder and CEO of Impact Makers of Richmond, VA.

Tell me about yourself and the company.
I am a former Andersen Consulting professional who has done both an undergraduate degree and MBA at Kellogg School of Management at Northwestern.
Impact Makers is an IT consulting firm, fully owned by two public charities. If we’re sold, all proceeds from that sale will go to make in-perpetuity community impact as well as to impact investments in social enterprises.
Our work is project and program management, process improvement work, management consulting for the CIO, governance risk and compliance, and security work. Also digital strategy and mobile and web implementation. The majority of our work is in the healthcare space, both payer and provider, as well as healthcare governmental agencies.
Why would a for-profit company donate all of its profit to charity?
I guess it started with me. I’ll take full blame. I was fascinated in my undergraduate degree with reading a business case on Newman’s Own. We are essentially the Newman’s Own of IT consulting. Newman’s Own is Paul Newman on the side of salad dressing, but they’re a for-profit company that gives all profits to charity and is fully owned by a foundation. I was fascinated by that business case.
I went to work with Andersen Consulting, overseas mostly, and found that I was good at what I did. But I wasn’t necessarily values-aligned with some of our clients that I worked at. As well, the company culture tended to be very money-focused and individual-focused. I found it compelling to think of an idea of creating an Andersen Consulting on the Newman’s Own model. I wrote a paper about it when I went to do my MBA with that in mind.
Non-profits and government do a lot in the world to solve social and environmental problems. I am a capitalist. I have business degrees. But figuring out how to use the power of the free market to solve social and environmental problems instead of government handouts or non-profits is something that spoke to me. It has actually gotten bipartisan support, which doesn’t happen much these days in the world.
I guess that’s the purpose. How do you transform individuals’ skills, experience, and training through their professional work every day to not just deliver client value and do all the things of job creation that any other for-profit would do, but also not be just a good steward in the world, but actually make a real impact in the world at the same time. Then what does that do for our employees in terms of personal growth and satisfaction? Not just job satisfaction, but speaking to everyone’s desire to leave the world a better place than the way they found it.
It’s interesting that your company is a for-profit that acts like a non-profit, while your non-profit health system customers make dozens of millions of dollars just like a for-profit company. Does it seem strange to explain to a non-profit health system what it’s like being a mission-driven organization?
That’s why healthcare has worked so well for us. So many people in the healthcare industry really care about patients, really care about patient outcomes, and have a deep culture of caring for their members and patients. That culture of caring and wanting to make a difference is pervasive in healthcare. It’s the reason we like working in the healthcare space and why it’s been such a good market for us.
It’s obviously an easy sell to the non-profit healthcare organizations we’ve worked with, although I would say it’s probably about 50-50 in terms of nonprofit and for-profit. We work with large national payers, providers, and healthcare government agencies. Probably a little bit more than half are on the non-profit or governmental side. Newman’s Own, which is a wonderful organization, sells using not just that it has a good product, but it uses cause-based marketing. There’s this class of conscientious consumers that buys socially impactful products.
We’re B to B — we’re not B to C — and we’re services. Our clients buy on capabilities and price. While our model is interesting to C-level folks who care about the company’s community impact footprint, really we’re competing on capabilities and price. As a for-profit company, I think that’s a good thing.
Sixty percent of our work comes from existing clients. It might get us in the door to talk to a C-level person or it might be a tie-breaker on a competitive bid, but that hasn’t been the reason we’ve won work. Although there’s been this immediate mission alignment with some of our non-profit healthcare partners, as you mentioned, which I think helps with the relationship long-term.
An article announcing that you’ve been named to the Inner City 100 list of fastest-growing inner city businesses had a picture of your cool offices. What attracts an employee to a fun, urban location instead of a faceless glass building in a suburban office park?
We’re in Richmond, Virginia, in a warehouse district that’s being renovated. All the warehouses are being turned into breweries and various interesting businesses. It is also a big hipster community. It’s a trendy area in Richmond, which is a wonderful place, You don’t always associate Richmond, Virginia — the home of the Confederacy — with hipsters.
It’s a really neat space. It’s accessible to public transportation. We have solar panels on our roof, which provide 25 percent of our electricity. It was aligned with being in the city. It was aligned with our values and with environmental impact standards. We’re founding B Corp, so we try to not just focus on social impact, but environmental impact and all of those things as well.
It was a good space. It was aligned with our values and aligned with a lot of our staff’s values. It’s an open office environment. People like to work in the space. Although our clients don’t hire us for our model as an IT consulting firm, we’ve had amazing retention. We’ve been Inc. 500 three years in a row and Inc. 5000 four years in a row.
The reason we’ve been successful isn’t our model, but because employees want to come work for us and stay. We’ve had 10 people leave in nine years. If you know the IT consulting industry, that’s an unbelievably amazing retention rate. People want to work for a company that’s mission-valued, mission-aligned. That creates values for our clients because our clients get employees that stay for the entire duration of a project. Mission-aligned teams outperform ones that aren’t mission-aligned, all else being equal.
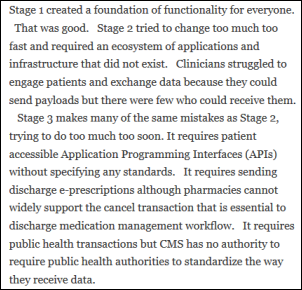
What’s the state of healthcare IT consulting compared to a couple of years ago when everybody was mostly focused on Meaningful Use and ICD-10?
We’re seeing this tremendous interest in transformation, as a keyword, caused by a bigger interest in consumer-focused healthcare and this whole interest in the Triple Aim concept that we’re seeing from our clients – quality, access, and reliability. Those things combined are creating this enormous interest in transformation, whether that’s digital transformation or even just core operational function. Looking holistically at the organization, doing organizational assessment work to align around those goals and values.There’s also the obvious trend of mergers and acquisitions going on across the space.
Those three things — Triple Aim, mergers and acquisitions, and the focus of on consumer-focused healthcare – are revolutionizing the space and creating these large transformation projects that look across security, digital, organizational structure, and how to best align both from an IT perspective as well as a business perspective for delivery. We’ve been really focused on these large, enterprise-wide transformation projects for assessing, planning, designing, implementing these efforts and managing the delivery of those efforts.
Slow-moving and change-resistant health systems are being asked to respond quickly and to assimilate cultures thrown together by merger and acquisition. What are they doing to address their cultural lethargy?
I think it’s streamlining. We’re helping both payers and providers in these transformational roadmaps. We’re seeing a common denominator being, whether it’s Triple Aim or others, that technology needs to provide the right customer engagement, the right information at the right time with optimal cost. It all sounds so obvious, but as you said, they’re really moving into a brave new world that maybe other industries has already transformed themselves and healthcare is being pulled into that same transition.
Providers are suddenly interested in patient engagement now that there’s a financial carrot in place. Why did it take so long to bring patients to the table?
We’re seeing governmental programs and payers creating a financial incentive for providers – whether it’s accountable care organizations, medical homes, or any of the various models – in paying for performance and paying for outcomes. Those things require direct patient engagement and consumer focus, almost like a retail organization would. They need to be creative and not only to do the right thing for the patient, also to be successful financially.
What are providers doing to change from a "here we are, come knock on our door to get services” model to reaching out like a traditional company might do?
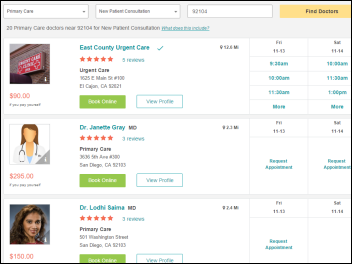
There are a number of trends. The one that we’ve been focused on is making sure that we make that connection between the patient and provider. Not the hospital provider, but the individual physician or specialist. Interactive smart provider search engines that are very specific and unique that make sure the patient with the right keywords get to the right specialist they’re looking for at the right time. Trying to make sure that that interaction happens. For health systems, that it’s the physician that’s within their health system. There’s a desire to ensure the patient stays within the system.
Secondly, using mobile technology to interact with the physician specialist and patients in a way that enhances clinical outcomes. It has to be a secure way, of course.
Those are the areas where we focused within the digital framework to ensure consumer engagement.
Short of changing their business structure, what can companies do to make a social difference beyond the usual employee volunteer day?
We have the ownership structure, but we also give up to 30 percent of our operating margin away to local charitable organizations that are secular, apolitical, 501(c)(3), local to where we do work, and that help people help themselves. We’re governed by a volunteer board. I’m the founder of the company, but I don’t own any of it. Our volunteer board chooses these partners.
Whether you give 30 percent or 10 percent, choose mission-aligned partners that might be aligned in the healthcare space — if you’re doing healthcare consulting — to support. Make that part of your brand. That’s meaningful to employees. You don’t have to do 100 percent over the life of the company like we do. Even 10 percent or 15 percent is meaningful. Doing good is good business, too. It adds to the value of the brand. It adds to your own employee engagement in what you’re doing.
We also do pro bono consulting for our charitable partners. Having employees being able to, during work hours, work at client sites is meaningful to employees and is a benefit to employees and creates community impact. Having a mission and leading with values. We started with mission and then our values came from that. That’s been the true reason why we’ve been successful, because we are absolutely values-based. Doing the right thing is critical for both clients and employees.
Our executive team says, do the right thing for our client. Do the right thing ethically and morally. If you have to make a decision with the client without going up the chain and you do it, as long as you do the right thing, we’ve got your back.
Having those strong values and articulating those values often. Our performance review process is tied starting to our values at the highest level, and everything follows from there. We repeat that often at every company meeting.
Then the final thing is we’re a founding B corporation, which is a certification standard for companies that aren’t just about making profit, but also taking into consideration the environment, employees, and community and aren’t just about maximizing shareholder value, although they’re all for-profit companies. Companies like Patagonia, Ben and Jerry’s, and Etsy that just went public are shining examples of B corporations. It’s a community, internationally now, of 1,400 companies that are focused on making a difference using the power of the free market to solve social and environmental problems. Any company that has a mission to make a difference can consider that to be part of something bigger than just the company that they’re doing and help spread that ethos within business.
Do you have any final thoughts?
What we’re doing is pretty game-changing. It’s pretty disruptive, actually. If you think about what we’re doing, we’re a group of middle-class professionals doing the same work we’ve always done, but structuring it differently, and collectively making the same impact in the community as foundations, and eventually large foundations.
Our goal is to have, in the next seven to 10 years, a sale of the company that puts $120 million into these foundations that will make in-perpetuity impact and create more Impact Makers through the investments that they do. Not doing it at the expense of employees, because we pay market salaries to employees, and have employees share a little bit in the value that’s created. At the same, have a way to raise capital from the capital markets. We’re in the process of raising preferred stock equity in a way that is still aligned with our model and is largely from the non-profit world.
If we can solve that, that’s creating a new model that no one has ever done before. It’s democratizing philanthropy in a way that’s not even done. I think that’s the disruption, that group of middle class professionals structuring things differently and collectively making an impact in the community like has never been done before.





























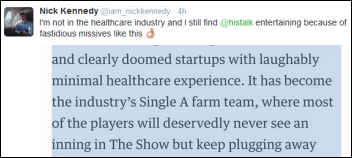












I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…