Curbside Consult with Dr. Jayne 5/23/16
I’m working with a client who hired my partner and me to do a complete review of their practice operations and both financial and clinical workflows. Initially, they had requested us for a system selection engagement since they were ready to jettison their vendor and look for greener pastures.
Since I’ve worked with this particular vendor multiple times, I strongly suspected that the problem wasn’t with the system at all, but with how it had been implemented and was being used. The client has been on the system for a long time and I suspected they hadn’t been keeping up with newer releases, or if they had, that they hadn’t been adopting new features and incorporating them in their workflows.
They understood that paying us for a thorough review and potentially executing a remediation plan would definitely be more economical than completely throwing out the system. My partner started digging through their financial workflows a couple of weeks ago and we didn’t find anything too surprising there.
The practice is a group of procedure-driven subspecialists. In our experience, those groups tend to be fairly strong at maximizing their financial returns. We found some opportunities as far as them not using some of the automation available in their system. Although it may save them a couple of staffing FTEs, in a group their size, it wasn’t truly earth-shaking. If we had to give them a grade on how well they’re using the system and keeping up with the times, we’d give them a solid B+.
The clinical team’s use of the system was something else entirely. As we worked through their clinical workflows, it was apparent that they hadn’t taken advantage of many of the system upgrades that had occurred since their initial go-live more than five years ago. Once we review the user workflows, we typically meet with the physician champion or super users to determine whether they are aware of new workflows and made a conscious decision not to use them or whether they were not aware of the best practices. We try to avoid having these conversations with end users because they become frustrated when they learn that there were enhancements that could have helped them and their practice didn’t implement them for one reason or another.
The group has had a fair amount of turnover with regard to EHR super users, although the same EHR lead has been present since system selection. With every feature we discussed, her answer was, “Nobody told me about this” despite the vendor offering free Web-based training every time a system upgrade was available.
The physician champion just wanted to argue about how poor the system was and how they were going to replace it anyway rather than wanting to learn about the features that would eliminate their pain points. He clearly was not on board with the practice’s executive committee decision to bring us in to try to fix the current system rather than chuck it.
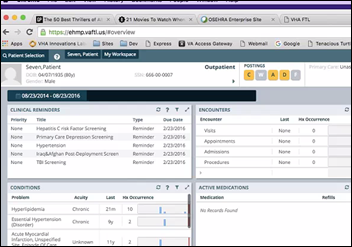
We also found that essentially they had been doing what needed to be done to get their Meaningful Use incentive payments, but hadn’t at all embraced the clinical realities of the metrics they met. For example, they made sure that every patient had an entry on his or her problem list, but the lists were not up to date; nor was there any policy or procedure in place to cover how often they should be updated or by whom. As far as they were concerned, since their vendor provided documentation that the problem list was “in use,” that’s all they needed.
One of the providers I interviewed told me that he didn’t put any problems on the patient’s list that he didn’t personally treat. This is the classic view of the problem list as “the physician’s problem list” rather than “the patient’s problem list.” I tried to have a conversation with him about the goals of Meaningful Use in providing more comprehensive records for patients, making it easier for practices to integrate data, the evolution of patient-driven medicine, etc. but he was having none of it.
He mentioned that his job was to take care of patients and made statements that sounded an awful lot like he felt he was above making sure he was aware of all the different problems impacting the patient. I tried to use logic with him, noting that although he doesn’t manage a patient’s hypertension or diabetes, they’re certainly important factors to consider prior to putting the patient on an operating table.
I also demonstrated his system’s functionality to filter the problem list by sorting the problems that are attributed to him to the top of the list, but he continued to push back. Although he seemed to agree in principle, he wouldn’t arrive at the point where he admitted that he (or his staff) should be keeping an updated problem list.
Having tried the “it’s good clinical care” angle and failed, I decided to press a little more on the MU aspect. I asked how he felt about the fact that he accepted federal incentive payments for doing something that he clearly wasn’t doing.
Mind you, I had no problems pressing this guy because he’s taking home more than half a million dollars a year. He’s also pontificating about being there to care for the patient, but refusing to do the basics. I tend to get a little aggravated with people like this, having come from the primary care trenches where many of my peers were working long hours updating charts to provide complete and accurate data for their patients (simply because it is the right thing to do) while making 70 percent less money than this guy.
He rationalized his actions (or lack thereof) by saying that the EHR vendor provided documentation that he met the performance threshold. I explained that the reports deal with the fact that the problem list contains data, not that anyone is actually working with it or keeping it current. Ultimately the physician is responsible when someone attests on his behalf that he has done something that he clearly hasn’t.
Although this guy may be a technically brilliant surgeon, I’m not impressed with his professional ethics. When I told this story to a friend, he assumed the surgeon in question was older and had been trained in a more paternalistic model. This physician finished his training within the last decade, so I’m not buying that excuse.
Medical schools are doing a lot of work trying to shift physician culture and educate in the benefits of patient-centric care. Regardless of whether you use an EHR to document your work or not, we need to be doing things differently and this guy clearly doesn’t get it.
Still, as one of the highest-compensated physicians in his region, he’s being rewarded because we still value procedures over cognitive skills. Ultimately the drive towards value-based care should help with some of this, but I don’t think I’m going to see the change in my career lifetime.
Is it just me, or are there still a lot of physicians like this out there? Do you have to deal with them? Email me.

Email Dr. Jayne.













































I initially questioned the profile's authenticity because all of the headshots in the profile are clearly generated or enhanced by…