News 2/26/25
Top News

Lawmakers warn the VA of their concerns about its Oracle Health implementation in a House hearing:
- An independent analysis predicted a total project cost of $50 billion, but that was before program changes and delays that warrant producing a new estimate.
- Recent staffing cuts that were mandated by the White House included the firing of eight probationary employees of the EHR modernization project and the resignation of another 16 under the deferred resignation program.
- The Oracle Health contract expires in May 2028, but its system is live in just six VA facilities with 164 to go, and go-lives won’t be started until mid-2026. The VA acknowledges that it won’t be finished by the contract’s end.
- Oracle Health EVP/GM Seema Verma stressed that “The totality of updates, enhancements, investments, and innovations to the EHR show that this is a dramatically improved system from what was originally deployed in Spokane in 2020.”
HIStalk Announcements and Requests
Thanks to long-time HIStalk sponsor AGS Health and CEO Patrice Wolfe for stepping up as a Founding Sponsor. Those coveted Founding slots, which are limited to two, have become available only 2-3 times over many years, and only when one of those sponsors was acquired. Here’s a refresher on what the company does:
AGS Health is more than a revenue cycle management company — we’re a strategic partner for growth. Our distinctive methodology blends intelligent automation with award-winning RCM services and high-touch customer support to deliver peak end-to-end revenue cycle performance and an empowering patient financial experience. We employ a team of 13,000 highly trained and college-educated RCM experts who directly support more than 150 customers spanning a variety of care settings and specialties, including nearly 50% of the 20 most prominent U.S. hospitals and 40% of the nation’s 10 largest health systems. Our thoughtfully crafted RCM solutions deliver measurable revenue growth and retention, enabling customers to achieve the revenue to realize their vision.
We’ve been longtime Costco members, but I kept hearing about Sam’s Club’s superior technology and its stress-free, line-free shopping, and unlike Costco, an app and website that allow checking prices and inventory levels. In my first Sam’s trip this week, I used Scan and Go to ring myself up, paid instantly, and then bypassed checkout entirely and just sauntered out the door as AI-powered cameras verified my cart. No waiting in line to pay, no door-check bottleneck. I can see making a quick stop at Sam’s for just a handful of items, whereas the cupboard has to be pretty bare to be worth Costco trip anxiety. I’ll keep both memberships since Sam’s wins on prices, store layout, and produce, but Costco still leads on clothes, wine, and regular rollout of new items that I don’t need.
Sponsored Events and Resources
Live Webinar: March 4 (Tuesday) noon ET. “Securing a competitive edge in value-based care with AI: Data-driven strategies for enhancing returns across MA, ACO and Commercial programs.” Sponsors: Navina, AMGA. Presenters: Dana McCalley, MBA, VP of value-based care, Navina; Ron Rockwood, executive director of value-based care, Jefferson City Medical Group; Jonathan Meyers, CEO, Seldon Health Advisors. As value-based care models evolve, healthcare organizations must leverage AI to stay competitive and drive better financial and clinical outcomes. This webinar offers data-driven strategies for improving risk adjustment accuracy, optimizing risk stratification, and streamlining clinical and administrative workflows. You’ll walk away with proven techniques for measuring and quantifying the impact of your value-based care initiatives across your organization
Live Webinar: March 20 (Thursday) noon ET. “Enhancing Patient Experience: Digital Accessibility Legal Requirements in Healthcare.” Sponsor: TPGi. Presenters: Mark Miller, director of sales, TPGi; David Sloan, PhD, MSc, chief accessibility officer, TPGi; Kristina Launey, JD, labor and employment litigation and counseling partner, Seyfarth Shaw LLP. For patients with disabilities, inaccessible technology can mean the difference between timely, effective care and unmet healthcare needs. This could include accessible patient portals, telehealth services, and payment platforms. Despite a new presidential administration, requirements for Section 1557 of the Affordable Care Act (ACA) have not changed. While enforcement may unclear moving forward, healthcare organizations still have an obligation to their patients for digital accessibility. In our webinar session, TPGi’s accessibility experts and Seyfarth Shaw’s legal professionals will help you understand ACA Section 1557 requirements, its future under the Trump administration, and offer strategies to help you create inclusive experiences.
Contact Lorre to have your resource listed.
Acquisitions, Funding, Business, and Stock
OpenEvidence, which offers a clinical decision support chatbot for providers, announces $75 million in funding at a $1 billion valuation. It recently signed a content agreement with The New England Journal of Medicine.
EXA Capital acquires human services-focused EHR and care management software vendor PrecisionCare.
Clinical documentation software company Retrieve Medical will acquire Curatus, which specializes in AI-powered provider data management.
HealthStream reports Q4 results: revenue up 5.2%, EPS $0.16 versus $0.15. HSTM shares have gained 24% in the past 12 months, valuing the company at $1 billion.
Sales
- Mass General Brigham (MA) will implement the Philips Capsule Medical Device Information Platform, Philips Clinical Insights Manager, and Philips Capsule Surveillance technologies.
- Hartford HealthCare (CT) will use K Health’s agentic AI-based virtual primary care software to power its new HHC 24/7 virtual care service.
- ECU Health (NC) selects Pep Health’s patient experience analysis software.
People

Eric Talbot, MBA (MedFuse) joins CheckedUp as chief data and analytics officer.

Troy Tazbaz, the former director of the FDA’s Digital Health Center of Excellence, returns to Oracle as SVP of data center planning – corporate development.


Guidehouse names Erik Barnett and Brian Smit (R1 RCM) partners in its health and managed services practices, respectively.

MGMA hires Julia Rosen, MBA (Pera Healthcare) as SVP of IT.

Jeff Surges (RLDatix) joins Brighton Park Capital as partner.

Eve Cunningham, MD, MBA (Providence) joins Cadence as chief medical officer.

Clinical Architecture names Laura Nixon, MBA (Nixon Strategic Consulting) as VP of interoperability solutions.
Announcements and Implementations

MyMichigan Health implements QGenda’s provider credentialing software.
Corti adds Wolters Kluwer Health’s UpToDate clinical decision support content to its AI-powered Assistant app for clinicians.
Lumeris announces GA of Tom, an AI-powered clinical workflow tool for primary care.

Ray County Hospital and Healthcare (MO) works with OCHIN to replace CPSI (now TruBridge) and EPowerDoc with Epic.
Altera Digital Health integrates Medicomp’s Quippe AI engine with its TouchWorks EHR. Medicomp also releases Quippe Alchemy that applies AI to problem list cleanup.
Inovalon launches an AI-powered, EHR-integrate clinical trials recruitment tool.
Government and Politics
The White House says that former health tech executive Amy Gleason is serving as acting administrator of Elon Musk’s DOGE cost reduction program.
Privacy and Security
Malware researchers find that a China-based hacker group is disguising its malware as a Philips DICOM viewer.
Other

Technical.ly profiles the University of Maryland Medical System’s AI-powered remote fetal monitoring program, which launched last year using technology from PeriGen. Sixteen nurses work at the Neonatal Outcomes Impacted by Escalation Safety Telemetry (NEST) center, monitoring labor and deliveries across seven hospitals in real time. Nurse Manager Christine Haas, RN points out that the nurses have often been quicker to catch abnormalities than the AI: “This program is fundamentally the nurses’ brains with the AI counterpart, just really sort of being a reinforcement and a help for them.”
Sponsor Updates
- Capital Rx releases a new episode of “The Astonishing Healthcare Podcast” titled “Pharmacy Benefits 101: Stop-Loss Insurance, with Mike Miele, FSA, MAAA.”
- Agfa HealthCare announces that several hospitals within the Osakidetza Basque Country healthcare network in Spain have successfully transitioned to its Enterprise Imaging for radiology and molecular imaging.
- Philips Capsule participates in the IHE North America Connectathon 2025 in Toronto.
- CloudWave publishes a new guide titled “The Strategic Value of Managed Cloud Services in Healthcare.”
Black Book Research’s list of top, physician-rated health IT for rural and critical access providers includes the following HIStalk sponsors:
- TruBridge and Meditech Expanse – rural and CAH inpatient EHRs
- Redox – rural healthcare interoperability and HIE vendors
- Inovalon – population health, rural healthcare management, quality and safety solutions
Blog Posts
- Celebrating 15 years of innovation and impact in healthcare (Nordic)
- How to Transform Patient Scheduling: 7 MEDITECH 2.2 Features (CereCore)
- Pharmacy Benefits 101: Building an Award-Winning Call Center from Scratch (Capital Rx)
- HIPAA is More Than Keeping Medical Records Secure (AdvancedMD)
- Agfa HealthCare Shines at ViVE 2025 with Incredible KLAS Triple-Award Win (Agfa HealthCare)
- 2025 New CPT Codes to Capture Evaluation and Management Telemedicine Services (AGS Health)
- EHR System Speed and Reliability – The Foundation for EHR Success (Goliath Technologies)
- Advancing interoperability: Altera at the IHE North America Connectathon (Altera Digital Health)
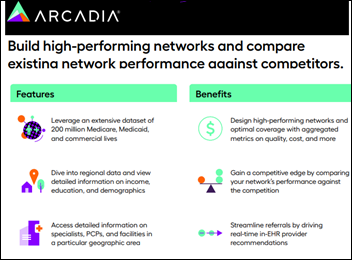
- 3 actionable steps to turn healthcare data into action (Arcadia)
- Inside Healthcare’s Cybersecurity Battle: A Q&A with Availity’s CISO (Availity)
- Managed services in healthcare: Balancing efficiency, stability, and growth (Cardamom)
- 8 Easy Ways to Prepare for an OCR HIPAA Compliance Audit (Clearwater)
- The Growing Importance of Population Health in 2025 (Direct Recruiters)
- Wintry Weather Can’t Dampen the Vibe at ViVE 2025 (DrFirst)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Follow on X, Bluesky, and LinkedIn.
Contact us.

















The CEO sentenced to jail for massive healthcare fraud will get pardoned in a week.