Michael O’Neil is founder and CEO of GetWellNetwork of Bethesda, MD.

Tell me about yourself and the company.
I started this crazy journey called GetWellNetwork 17 years ago. I had a personal cancer experience while I was going through a graduate program for a JD/MBA at Georgetown in DC. I had one of these wonderful medical outcomes, but I had not so wonderful experiences as a patient and family. I decided to make this my life’s work and to use my limited talent to try to make it better for the next guy up.
Are we getting better at recognizing consumers as going through a health journey rather than seeing them as patients who make the cash register ring through a series of episodic encounters?
We are absolutely getting better.This starts first with awareness, then solutions and the commitment to implement them.
When we started this business, the only awareness measure and the only energy was because part of the executive suite’s bonus was tied to a Press Ganey score. Today, reimbursement changes, competition inside a market, and the ascent of the voice of the consumer have impacted the way healthcare providers operate and measure themselves. We’ve come a very long way and it’s been energizing.
Are patient satisfaction scores meaningful beyond focusing on low-hanging hospitality fruit that is only marginally related to outcomes, such as food quality and hallway noise?
The world is moving so much faster than CMS has declared these 23 questions, or whatever the number is that get measured, as part of a compliance requirement. To be honest with you, no, I do not think that the current patient satisfaction survey is the true measure of a patient’s experience. The way the world operates now, I’ll give you my feedback right now at the moment. That’s how consumers behave in restaurants, on airlines, and on their phones.
There is a total step function that’s underway in understanding how to capture, understand, analyze, and act on patient experience in the moment. The current measures are not right.
Outside of healthcare, businesses want to know about customer dissatisfaction in real time so they can fix the problem instead of losing the customer via a scathing Yelp review after the fact. Do patients have a way to push that imaginary button to get attention for their immediate clinical or comfort concern?
The cool thing is that the technologies exist today. Not only in other parts of the world, but they exist in healthcare today. The technology is in place and it’s fairly inexpensive.
The hard part of this job is change management. When a patient is at the point of care in a highly vulnerable moment and they’re telling us — through their behavior, reaction, lack of reaction, or lack of engagement – that, “I don’t understand my meds,” is the process and the workflow in place to make sure that we can respond to that unique, one-to-one patient need in the moment? That’s where I think the heavy lift is, and has to be.
Those workflows and systems are not all in place today. But the good news is technology is there and it is relatively inexpensive. For the organizations that have the courage and fortitude to say, we’re going to do this differently, it’s time. We can go make this happen together.
In both healthcare and IT, most customers like the individual person but not the organization that employs them. The institutional persona overrides that feeling that, “I like Bob the help desk guy or this nurse who was nice to me.” Are hospitals and practices finding a business case for at least trying to convey an appearance of organizational patient focus?
I think so. The evidence of that is pretty straightforward. I’m chairing a day of the Next Generation Patient Experience Conference in San Diego. You’ve got big investments. You’ve got chief experience officers, highly seasoned senior executives who sit on executive teams to drive strategy around this stuff. You have all kinds of new measures that the organization is being held to account on. It’s now impacting their business. They’re measuring it in terms of how patient loyalty translates to revenue and whether patients are leaving the system because they’re not having the experience we want them to have.
It has come an exceptionally long way. Competition inside these mini markets has gotten intense. You can’t walk out of a train station, pass through an airport, or get on a highway without seeing four out of eight billboards or signs for health systems. They’re competing significantly on patient experience.
Ultimately it’s great for the patient. You need to make it better for me. I love that about the whole process.
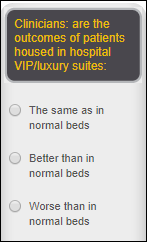
Health system executives, even though as patients they are treated as VIPs, often leave their own hospital encounter surprised by missed meds, poor communication, and impersonal care. Can those executives get a realistic idea of how their organization is doing beyond patient survey responses?
There’s an acute – no pun intended — awareness of the industry’s need to move a quantum step forward in how we deliver care. We think of it as precision engagement. It’s like the analog to precision medicine. If the person that you have just given this magic pill to isn’t going take it — they don’t understand it, they can’t afford it, they don’t know where to get it – it doesn’t matter how good the pill is.
There’s an acute awareness that one-to-one engagement is required to deliver great care. The leaders of the provider organizations know it’s there. There’s some confusion on how to implement a precision engagement model so you can actually deliver one-to-one care at scale. It requires, as always, people, process, and technology to come together to deliver a different model of care. That’s where the challenge lies. But the awareness is there.
How do you measure the result of that patient engagement in terms of outcomes or cost?
Here’s the cool thing about precision engagement as a transformative strategy for healthcare delivery. The measures are already there, already in place, and already required. Organizations are measuring patient satisfaction, readmission rates, the number of falls, and how many people are leaking out of their system and going somewhere else for their care.
The question is, if you implement a new precision engagement model of care, does the needle actually move on those measures? It’s not about creating new measures. The measures are sitting there right in front of them and that’s what’s on their dashboards. What we haven’t seen is, what are the breakthrough approaches in delivering care that move those measures in a significant way to make you the leader in the market and make you have the best outcomes clinically?
That’s where we believe there’s great promise. The infrastructure of measurement for impact on patient or precision engagement is there. It’s now about implementing breakthrough programs and watching the change actually happen by hard work.
We’re learning the power of social media commercial or political messages when they target users based on inferred characteristics from their Facebook likes or their responses to a a seemingly innocuous quiz. How can that power be used to improve health?
This is where the greatest promise is. It’s not just the clinical data and the claims data. The third leg of the data stool is patient-directed data. What is my situation at home, at work, and with my family?
Imagine if my mom’s provider knows that she needs to get to her rehab appointments, but I’m leaving on an international business trip. We probably could deliver a better dimension of care for my mom to keep her from having a fall and ending up in a hospital. What you’re saying is dead on. The capabilities are sitting right in front of us, adding a third leg to the data stool to deliver one-to-one interventions based on that person’s capacity to engage in their care at that particular time.
We can’t assume that all patients are the same. How do we make sure that we use the patient’s preferred method of communication and that we don’t bombard them with information that doesn’t pertain to them?
It’s taken us two and a half years, but we started with a 56-question survey that of course nobody would ever fill out. Through a bunch of clinical research, we have it down to 18 questions that assign a PEI score, a Person Engagement Index, that measures the capacity to engage across a couple of domains.
One of those domains is “technology use in my care.” Another is psychosocial. Imagine you and I are the same demographic and we both had a total knee replacement, but I scored a 27 on technology use and you’re an 89. Our provider can put you on a digital coaching program to have a great outcome, but for me, they had better visit me three times at home.
The possibilities are to be able to put a marker on every patient we ever touch, add that third leg of data to the data stool and deliver it to providers in real time so they can prescribe interventions that are relevant to me. My ability to follow my plan of care when I’m not in your skilled hands is literally the key to healthcare. That’s what we’re chasing at GetWellNetwork. Can we arm our provider partners with a new, unique data element that allows them to deliver the amazing care that they want to deliver on a one-on-one basis? It’s there today to be able to do it.
Is the term “patient engagement” misused?
A lot of terms are misused. All you need to do is walk the floor at HIMSS. Every year there are three or four buzzwords and all of a sudden, 3,000 companies claim to do them well. Like anything else, we need to look under the covers. These kinds of things are not small investments. Not necessarily of just money, but of time and focus.
It’s too easy to lump all this stuff into patient engagement. Patient engagement is not changing my visiting hours. Patient engagement is understanding down to the individual level what each patient wants their health for, not assigning their clinical indicators. What do I want my health for? Use that as a motivator to get patients to activate around their care, then use our amazing skill and infrastructure as clinicians to motivate and engage patients in their realm so they can be better active participants in their care.
The term patient engagement is overused. It has become mundane and generic. The whole world claims to do it. The easiest aspect of patient engagement is lighting up yet another app on the app store. That is not patient engagement. It’s important to understand the depth and the change management component to this work. It’s hard work. It takes a long time. You can’t sleep on it, because our patients need it and they need you to do it well.
Do some apps or approaches use methods that are overly paternalistic vs. participative?
What you just said needs to be literally reversed. Let me start by asking you what you want your health for. I would tell you, “As a 46-year-old cancer survivor with two daughters who are 14 and 12, the most important thing in my life is to be able to walk them down the aisle when they get married. There’s nothing that I wouldn’t do to take care of myself to give me the best chance for that to happen.”
If I start my healthcare dialog with my new primary care doctor on that level, I bet you damn well there’s a lot better chance — when he or she talks to me about my cholesterol level, about my diet, about my exercise regimen, about my stress level — that I activate into that protocol. More likely than if you just tell me to download an app that will tell me me what to eat every day.
Changing this to starting with, “What do you want your health for?” and delivering care in service of that person’s life goal instead of their A1c3 score will ultimately help change care.
How can standardized questionnaires be used to incorporate consumer self-assessment of health and wellbeing?
We are seeing a lot more of that. We refer to these as patient pathways. The clinical delivery model has been driven forever off of clinical pathways and those are great. These are clinical protocols for heart failure, diabetes, asthma, total knee, bariatric surgery, or being a new mom. The clinical pathway is the foundation by which evidence-based medicine is being practiced by the clinician.
The analog to that is the patient pathway. What is the patient’s role along that clinical path that we should be paying attention to? That starts with the patient setting their own goal. If we marry — more consistently and holistically — patient pathways to clinical pathways and respect that both have to happen to have the best outcome, it will truly bend the cost curve and change the care model forever.
Where do you see the company’s future?
On the corporate strategy side, we’ve been a buyer, not a seller. We’ve acquired three companies in the last three years to add to our capabilities. There are incredibly smart and bright entrepreneurs building incredible tools. Distribution in healthcare is very, very difficult and has allowed us to be buyers in that realm to expand our capabilities.
We’re seeing are two incredibly exciting areas of expansion of our impact. One is simply cross-continuum. We started this business off of a personal hospital experience at Johns Hopkins in Baltimore. The first 10 years of our business was simply making the hospital experience more efficient, more effective, more enjoyable, and more impactful for patients during that four days.
What we learned very quickly — but not quickly enough now that we’re focusing so much of our time on it — is that this four-day stay is such a small part of the patient journey. One area of expanded impact for us the last two years and certainly the next 10 years is to get outside the walls of the hospital. How do we help a new mom, a total knee patient, or a diabetes or asthma patient navigate their life journey through their health to optimize their impact on their lives with the trusted help of their provider in their community?
The second area is international. We didn’t know, nor did our board and our investors, whether this work would translate globally. We picked the Middle East two years ago as our first international market. They’re building a lot of new hospitals and acquiring and implementing a lot of US health IT, so they were at HIMSS and and we knew a bunch of these folks and they knew us.
We just launched our first site in Saudi Arabia and our first site in Abu Dhabi. I was just there last week walking the halls to watch this work impact the nursing staff, the physicians, the patients and families halfway around the world that most of us here in the United States only see on CNN. These amazing people want the same thing we do. They want great, personalized healthcare for themselves and their families that they can trust. That when you show up, people know who you are and treat you on a one-to-one basis and treat you as if you are family.
So the two areas where I believe we’ll have expanded impact over the next 10 years will be cross-continuum — more like serving populations and not just hospital patients – and doing this work globally.
I’m humbled by the amazing folks I have the chance to work alongside every day in these organizations. They are doing a very, very difficult job in a complex business world and clinical world. Doing this work is the most intellectually challenging thing you could ever imagine because the industry is hard. At the same time, the work you do is touching your college roommate’s son. It’s not work. We are honestly blessed to have the chance to go do it.
Do you have any final thoughts?
Every single one of us in this industry is also a patient. Our family members are patients. Our commitment to taking an active role in our health journey is one of the absolute keys to our life fulfillment. It becomes less about whether or not your blood work comes back positive versus the fact that you have taken an active role in your own health journey to pursue your life goals. That has been such a rich learning for me, for my own life journey and company journey. To watch that impact more people has been one of my life’s greatest joys. I encourage us all to take an active role, because when we don’t, the system can chew us up.
Comments Off on HIStalk Interviews Michael O’Neil, CEO, GetWellNetwork




























































Move your quotes to where they should be and it's no longer politics-in-the-blog, but instead a fact that's true at…