HIStalk Interviews Lissy Hu, MD, CEO, CarePort Health
Lissy Hu, MD, MBA is co-founder and CEO of CarePort Health of Boston, MA.

Tell me about yourself and the company.
I started the company as I was pursuing a joint MD/MBA at Harvard. I had always been interested in healthcare, but I became very interested in some of the more foundational problems around healthcare. I was in the hospital. I was seeing patients get discharged and come back in 30 days from nursing homes, where we had no visibility into the quality of care. All I knew was that there was a lot of variation in quality of care.
I left medicine to build CarePort to address some of the variations in post-acute care, to help patients make more informed decisions about the types of care that they can choose from. Also, to provide more visibility to their caregivers as they transition, often multiple times, across different nursing homes, home health agencies, and hospices. A lot of people, even in the healthcare industry, don’t realize that these settings are an integral part of the healthcare system.
From the hospital’s point of view, what are the most common transitions of care to post-acute care settings and what challenges do patients and families experience?
Patients get very little information about their post-acute care options, of which the two most common are skilled nursing and home health. Generally what happens in a hospital is that someone hands you a list of names and addresses and you have to pick. The case managers who are supposed to be guiding you are hamstrung by the vagueness of regulations around how they can get involved in patient choice. They are afraid to recommend one provider over the other. That’s something they really can’t do.
For a long time, we didn’t have much information about the quality of post-acute care providers. Patients were making important decisions literally based on just a name and an address. Most of them were choosing purely based on geographic proximity.
What you see in the Medicare data is that there is huge variation of quality of post-acute care providers. Just to give you one example, the average home health 30-day readmission rate is around 28 to 30 percent. But when you look at the bottom quartile of providers, it can be double. Even after you risk-adjust for different patient populations and all of that, you still see variation. It’s important when patients and families are making these decisions to think carefully and to have that information, because it can have a big impact on their recovery course.
What accountability do hospitals have for what happens when the patient moves to a post-acute care setting?
For a long time, there was no real accountability. In a fee-for-service world, you’re focused on throughput and trying to get your patients out in a timely manner. People started to think about post-acute care with the advent of readmission penalties. As we’ve moved toward bundled payments, accountable care, and risk-sharing with commercial plans, people have looked at those types of arrangements where they’re at risk. They have started to think about not only where they are discharging their patients, but also how they are doing in those settings.
Five years ago when I started this company, I would walk into a hospital and ask them, have you thought about your post-acute care strategy? It was crickets. Even doctors would say, all throughout medical school, I didn’t learn much about post-acute care or what that even is. Nowadays, when I walk into a hospital and we’re talking about their post-acute care strategy, it’s in the top three or five things that they’re thinking about. How do we have better control and management of our patients who are in this intermediate level of care who aren’t ready to go home just yet?
Should hospitals who claim to be managing population health have some control over what happens in post-acute care facilities? Are they expanding that idea into owning or managing those other providers?
The question of who owns the patient is a hot topic in population health right now. I think it’s the responsibility of the hospital to offer guidance in choosing that post-acute care provider. It’s not really much of a choice if you’re just giving the patient a list of names and addresses. At worst, it’s just totally uninformed and almost random. Hospitals have the responsibility to guide that choice and make sure that the patient is set up for success. That they’re going to a facility with lower readmission rates, higher star ratings, and all those factors that folks should be looking at when they’re choosing a post-acute care provider.
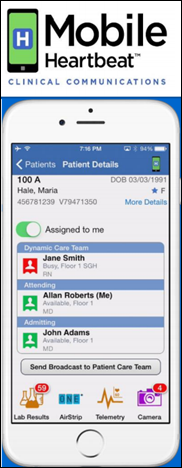
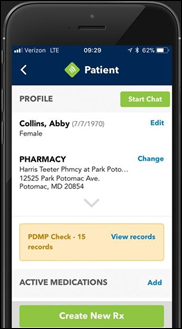
For ongoing management of the patient, it depends on who is bearing the risk for that patient. From what we’ve seen, hospitals that are engaged in ACOs or bundled payments are staffing out with care coordinators who are managing that patient across different settings. They need to have information from these nursing homes or home health agencies in real time about how those patients are doing. We make sure that the patient is set up for success, but we also continue tracking them once they’re in the post-acute care setting.
A lot of people don’t even know that nursing homes have EMRs. When I was initially talking to hospitals about giving them tools to track their patients in real time rather than just having retrospective data, a lot of them were skeptical. They thought that nursing homes were on pen and paper. We had to validate early on the hypothesis that most skilled nursing facilities are on some type of system, and often cloud-based systems where you can build APIs and pull this data rather than having these painful, one-off integrations that sometimes you encounter in healthcare.
How do you describe the benefits of your product to hospitals?
I emphasize that they need to have visibility into what’s happening to their patients in post-acute care from a readmission perspective. Also from a cost perspective, because if 40 percent of their Medicare patients are going into some type of post-acute care setting, that’s a big tranche of patients and they need to have that visibility from a readmission perspective. There are wide variations in how long people are in skilled nursing facilities. The average cost per day in a skilled nursing facility is between $500 to $700, so it’s a big chunk of change. Also to prepare themselves, as they are managing larger and larger patient populations, for having a sense of how their network is performing from an analytics standpoint and having that holistic view.
What patient information do skilled nursing providers and hospitals want to exchange?
I see this almost like a two-sided network. You need the engagement of the hospital, but you also need the engagement of the post-acute care providers to want to share that data.
When I was starting this company, one of the things I wanted to validate and test was the willingness of a skilled nursing facility or home health agency to share data with the hospital. It wasn’t a completely clear-cut answer. From what I had seen in the hospital, there was definitely some trepidation in sharing their own data. When we went out and spoke with a lot of these post-acute care providers, one of the things that they said to us was that they are being asked for specific care protocols to take care of ACO patients, for example, in a certain way. Often they have no idea who those ACO patients even are.
We need to add value, not only to the hospital, but to the skilled nursing facility and home health agency. We can collect data on when a patient is admitted, when they’re discharged, and some of the clinical factors, like the medications that they’re on in the nursing home. We can pass that, for example, to a hospital care coordinator. But at the same time, while the post-acute provider is not paying us, we add value by giving them things such as the name of the patient’s care coordinator and whether they are an ACO or a bundled patient. We add value to both partners.
How has the Allscripts acquisition affected the company?
It wasn’t something that we were looking for. It’s not like I started this company and had it in my mind that it was going to be acquired in a couple of years. We had supportive investors who were willing to put more money into the company, so we had multiple options. This is my company, my baby, and I wanted to make sure that whatever the decision was would set us up for long-term success.
When I jumped out of medicine, it wasn’t because I didn’t like taking care of patients. I saw this as a problem that needed solving. I was passionate about it and I wanted to make an impact. I didn’t want to just get sold. You hear stories of products getting shelved and never seeing the light of day again. It was important to me that we were able to operate independently and that there was strategic value in the acquisition that would allow us to scale quickly.
I could have gone two ways. I could have raised a boatload more money, hired out a sales team, and sold on my own to hospitals, health systems, ACOs, payers, and all that. Or, here was Allscripts, which has a product called Allscripts Care Management, which was formally known as ECIN before they acquired it. This product was in 1,000 hospitals and 70,000 post-acute care providers – SNFs, home health, LTAC, rehab, transport, and DME – are receiving referrals from it. We were encountering it over and over again as that nexus between the hospital and the community. When I thought about scaling this product, it provided a real strategic advantage for us to be able to link up with this discharge planning product. Because the other thing I hear constantly in hospitals is, I don’t want to go to another platform. If I’m using this for discharge planning, I don’t want to log into another platform.
From a user perspective, the discharge planning product sends the referral from the hospital to the post-acute care provider and CarePort bookends that process. We help with the selection and then we continue to track that patient. From a platform perspective, it made a lot of sense. That being said, most of our customers are Epic or Cerner. We’re fairly EHR-agnostic in terms of our client base.
Do you have any final thoughts?
This is a really exciting time to be in healthcare. People are finally paying attention to this whole area of post-acute care that for a long time was largely ignored. I’m hopeful that with these payment changes and the focus in post-acute care, we will finally be able to deliver to patients a better post-acute care experience. It is a critical part of their recovery and I’m glad there’s an awareness around that. I’m glad there are financial incentives around that. I’m really excited in terms of where the next five years is going to take us as an industry.




































There was a time when my company went through multiple rebrands. These were relatively minor shifts, but completely unnecessary. It…