CIO Unplugged 1/31/18
The views and opinions expressed are mine personally and are not necessarily representative of current or former employers.
First Days
This is the third of a four-part series on key considerations and action items during your first 120 days in a new job.
They say the typical executive will switch positions 5-7 times during his or her career. How can you ensure a smooth and effective transition? This series is intended to compliment what others have written over the years with some fresh perspective. This post will begin where the last left.
Below are some ideas to consider from Day 31 – Day 60. A shout out to several peers whose experiences are reflected below.
Wayfinding
By this time, you should no longer need a GPS to find your way around campus. You are becoming familiar with the organizational culture and building foundations of trust with key leaders and team. You can now move to the next phase.
Meet and Greet
Continue your campaign to hit the ground listening. If you have already met with the primary leaders and influencers, meet with their direct reports. At the end of each week, look for key themes and opportunities and share with your team. Determine which challenges to pursue. Always close the loop with a handwritten note and share what action you are taking, if applicable. Remember, you have to build trust and confidence in you.
Extra: Publish key discoveries and the status of the action items to solve uncovered issues.
Vendors
By this time, the vendor community knows you are the new leader and how to reach you. Preserve your time. Unless something is on fire, resist the temptation to spend time with vendors until later. I believe in vendors as partners and I am a strong advocate of collaborative relationships that serve the best interest of the new organization. It is generally not a day 31-60 task. I will discuss leveraging vendors as partners in the next First Days blog.
Extra: Vendors interested in your success will provide invaluable organizational insights.
Assimilation Acceleration
Progressive organizations will have formal assimilation programs. Dive in head first. Take advantage of all programs offered. Assimilation is a process to help you identify any blind spots you might have as you immerse yourself in the new culture. It’s critical to receive feedback from peers and direct reports. Some of the feedback may hurt, but listen and learn.
Extra: If there is no assimilation program, work with your HR and develop one.
Coaching
Many organizations will offer formal coaching programs. Again, take full advantage of all resources offered aimed at helping you successfully transition in your new role. Leaders covet opportunities to enhance their abilities. If your organization does not offer coaching, ask for it. Asking for help is not a weakness, it is a strength. Arrogance stifles potential.
Extra: Interview potential coaches and go with the one who appears most unafraid to get in your face.
Present Often
Now is a good time to make yourself available to your organization so they can know you deeper and ask questions. Send invitations to all your management and offer to speak at their next team meeting. Make it a goal to make yourself available to all the smaller management teams in your division. Town Hall events are important, but the smaller the audience, the bigger opportunity for engagement.
Extra: Arrange a tour of different work areas so you can increase the odds of one-to-one interaction.
Live Healthy
More than ever, take care of yourself as a person. Leading is hard, but leading in a new job is harder. If you moved geographically, then the level of difficulty is increased exponentially. Eat clean, eat healthy. Drink in moderation, if at all. Get rest. You will be tempted to get up early and stay up late working, but the ROI is negative over time. Progressive companies often correlate healthcare benefit costs with live-healthy attributes, which provide additional incentive.
Extra: Share with friends and family your live-healthy goals so they can encourage you and hold you accountable.
The Why
You were hired into your role to bring about change. People will more readily follow leaders with a change agenda if they understand the why. As you formulate your go-forward strategy with your team, make sure everyone can articulate the why. Why do we need to change? Why is it important? Why should we change? Make sure the why is easily articulated and inspiring.
Extra: Ensure your manager is agreeable to and understands the why as well.
The Team – Gaps
If you have engaged deeply, you should be in the forming and storming stages. You may already know what gaps are in the team. This is not a bad thing. To think that there will always be this perfect match of new leader coming into an existing team is a fairytale. If there are gaps, identify them and fill them.
Extra: Engage the team in any new hire decisions, including full veto power over candidates.
The Team – Fit
If someone is a bad fit, address it quickly. Both you and the individual know it already, even if unspoken. It is likely the team also knows it. The worst thing you can do is to let it continue. It is bad for the individual involved, the team, you, and the organization. A bad fit does not mean a bad person or poor performer. It just means that there is probably a better fit for that person elsewhere. Sometimes it can be a fundamental philosophical difference that can’t be transcended. Sometimes it is a severe personality clash.
Extra: Be an advocate for that individual and assist him or her in their transition.
The Team – Develop
“Everything rises and falls on leadership” (Maxwell). Invest everything possible in developing your team. The ROI on developing engaged people interested in improving is immeasurable. The dividends pay out continuously. Take advantage of HR programs and supplement generously with IT specific programs.
Extra: Create complimentary opportunities that you can curate internally to increase your people development reach.
The Next 30 Days
While you are beginning to settle in and better understand your role, in Days 61-90, you lay out the strategy and begin execution. I’ll review some key considerations and takeaways in the next post.
Feedback
What other considerations and action items should leaders consider in their second month of a new role?

Ed encourages your interaction by clicking the comments link below. He can be followed on LinkedIn, Facebook, and Twitter.
















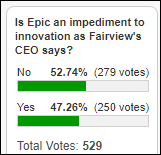










I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…