Tom Skelton is CEO of Surescripts of Arlington, VA.

Tell me about yourself and the company.
I’ve been in technology for 30 years. I’ve been doing this a long time. I still find it challenging and interesting and I hope that all this technology that we’re all deploying is making a big difference out there.
Most people probably think of Surescripts in terms of electronic prescribing, which is now widely implemented and in some cases mandated. The next wave involves add-on capabilities, such as prescription price transparency and automating prior authorization. What is the status of those efforts within the industry and within Surescripts?
I think you are absolutely right. There’s a lot of information going back and forth. Prescriptions, eligibility, and some of the core things have made huge strides.
Price transparency is a big thing and we as an industry need to rise to the occasion. We’re now able to provide, at the point of care, information about co-pay and therapeutic alternatives. These are extremely helpful for consumers and fit very well into a consumer-driven world.
I would say it’s early stages here. It took 14 or 15 years to get 90 percent of prescriptions on the network. Electronic prescribing for controlled substances was introduced in 2011 and at the end of 2016, the number was up to 14 percent. The transparency piece is going to take a little while, but we expect a very big year in that regard for 2018. We have a lot of rollouts going on and physicians and patients will start to benefit from that very quickly.
Will the model follow e-prescribing, where the initial effort involved standalone applications that were rarely used that were then integrated into physician workflow?
Yes. Physician workflow is one of the absolute keys here. We’re in a market where physician burnout is rampant. Pressure on their time is just absolutely amazing.
Since its founding, Surescripts has been focused on partnering with electronic healthcare records vendors and other technology providers to make sure that physicians and pharmacists don’t need to step out of their workflow to do what needs to be done for a patient. If you’re looking at price transparency, the issue goes just beyond pricing and the alternatives. It’s a lot deeper than that. It sets the stage for whether or not a patient adheres to the treatment regimen that the physician has prescribed. That’s one of the key things that gets lost. That co-pay differential — $10 here, $20 there — makes a big difference in adherence levels.
That’s a huge issue for the industry. It’s a huge issue for the country. You move into the world of electronic prior authorization. All of this ties together when you look at what’s going on in the market. This front door of understanding what the patient’s benefits really provide them. Also, understanding whether or not that prior auth is really necessary. Making that as easy as possible is key.
When you look at adherence, the introduction of prior auth alone causes adherence scores to fall substantially. They approach a 40 percent decline in some cases. Not just prescriptions — when I was running a radiology company, we saw 25 percent declines in utilization as soon we sent letters saying that we were introducing prior auth for MRIs. This is something the healthcare system has to get good at.
That’s also true when you look at specialty drugs. You’re seeing a huge increase in utilization and cost of specialty drugs across the system. That’s also driving prior authorization work, and that’s important as well. When you’ve got $500 billion worth of specialty pharmacy spend, you want to make sure that very sick people get access to the drugs that they are required to take.
Is it a challenge for EHR vendors now that many other software vendors want to connect to them and it’s hard to determine whether a given company is a partner or a competitor?
Absolutely. I don’t think there’s any question that the EHR vendors have a tremendous challenge in dealing with all of the requests that are made of them and in meeting those requests. We’re coming out an era where government mandates drove a lot of the innovation and pushed a lot of the coding towards the EHRs. As that era recedes into the past a bit, they’ve got tough choices to make about what innovation they code first.
Our job is to make it as easy for them as possible. We’ve built tools that help do that. We have accelerators that make it easy for them to do that integration, taking advantage of standards that exist in the market, both technical standards in the information provided and the standards around how that’s formatted. They’ve certainly got a lot of work that they need to do. They are the front door, in many cases, to these hospitals and physician offices.
FDA and drug companies are interesting in using provider EHR information for market surveillance. Do you see Surescripts as having a role in provider-FDA data exchange?
As our role in the industry has grown and changed, we’ve tried to support certain key initiatives, whether they’re government initiatives, research initiatives, etc. We’ve been pretty selective about that, but we try to help out where we can. When they are looking for a comprehensive story, going to the EHR is the natural place for them.
Should we be optimistic about the current and future state of interoperability?
It has changed and improved substantially. I worked at a company in Raleigh, NC where we had a huge team of people doing nothing but HL7 work. It was unbelievable the time, energy, and resources we put into that. The industry has moved so far beyond that now.
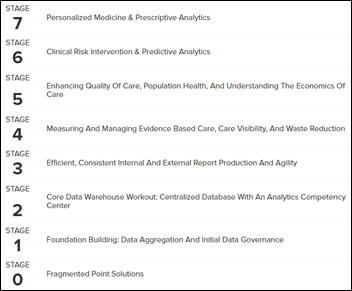
One of the challenges that the industry has is that we’ve not done a great job setting the bar for success. Like many industries that don’t have great data to support a position, we end up living on anecdote. I can tell you 10 stories about my mother and elderly relatives and what they encounter in the healthcare system with interoperability. Those anecdotes are going to rule the day until we as an industry come together to help explain what the interoperability journey looks like and help provide criteria upon which we can be judged.
What role do you see for pharma in using healthcare data?
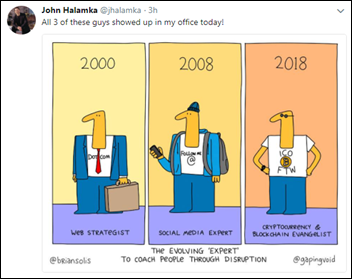
You’re asking specifically about data, but I’ll tell you one of our learnings. We just had some folks come back from JPMorgan. Emerging firms, smaller innovative firms, are being founded to fulfill a specific niche need. Pharma and life sciences are being viewed as important to their business models. Whether that’s a good thing or a bad thing is probably less the point than the fact that these are large, healthy firms that are seeking to foster innovation and further their interest. A lot of these smaller startups are looking to them as key components of their business model.
How much of the success of Walgreens and CVS was due to innovative IT work and what can providers learn from that as the market consolidates?
The key word obviously is consolidation. Whether it’s horizontal or vertical, the entire healthcare ecosystem is undergoing another wave of consolidation.
As you pointed out at the beginning, when you and I used to talk 15 years ago, there were 800 EHR vendors. That number is down substantially. If you look at the market share on the hospital side, you’ve really got three key firms. If you think about the fact that firms like Walgreens and CVS have historically been innovative, both in technology and in evolving their business model, I don’t think that’s a surprise. That would also be true of groups like United Healthcare and others. There are a lot of large firms that have been innovative in terms of what they’ve done to evolve both their model and the infrastructure that they’ve built to support that new model.
Where do you see the future direction of Surescripts?
You highlighted a couple of these things that we would talk about. We would certainly talk about price transparency. The other thing that we would talk about is that there’s a lot of commentary and interest in how interoperable the system is. The second piece of that is you have to peel back the onion a little bit. The information that’s being moved — how actionable is it when it arrives? How accurate is it? We’ve made a huge investment there over the last few years.
The introduction of Sentinel was an important moment for us as an organization. It moves us beyond just talking about how data is formatted to how actionable it is when it arrives. It puts us in a situation where, instead of having one in 10 prescriptions requiring some type of phone call or human intervention, we can work with our EHR partners to help identify areas where those prescriptions might benefit from different work up front to make those scripts more actionable when they arrive. We think that’s a important.
We’re going to scan 2 billion prescriptions this year and eliminate 50 million instances where somebody’s got to do something. That 50 million is a monthly number, not an annual number, so 50 million times a month we’re saving a pharmacist, physician, pharmacy tech, or a physician assistant a lot of time trying to sort through these. That’s what technology is all about. We’re proud to be moving down that path.
The ability to get information at the point of care is still an aspiration. Forty-eight percent of all diagnostic errors are still due to a lack of access to the appropriate information at critical points in the care process. We’re doing work around medication history. Delivering that information in a natural workflow for the physician is an important piece of what we do. A lot of folks do those things, but they do it with information that has lags in it or information that’s incomplete. But we’ve got big and deep coverage there and we’re providing a billion medication histories annually.
When you’re looking at informing care decisions, it is still a heterogeneous world. Health systems still rely on information from other medical practices and other healthcare institutions. The ability to locate a record for a patient in this heterogeneous healthcare system is an important piece of what we do. We can help people locate records, and once they’ve located them, there are a number of mechanisms for moving them and we have offerings in that area. You have to be able to know where that patient was and we think we can help.
Those are the types of things that we’re working on today. You can see additional intelligence coming to bear with us helping physicians and pharmacists through clinical alerting based on rules and engines that they help configure. We see all of that as natural for us and part of the prescription and medication ecosystem.
We haven’t even discussed opioids yet. Certainly from our standpoint, that is a huge situation that needs to be dealt with. We certainly respect, understand, and applaud all of the attention and the scrutiny, but there’s still a lot of work that needs to be done to make that real.
Our medication history offering is a big part of that solution. Doctors are allowed to see a lot of that information in most states. That’s important. I just saw some data the other day that shows that following the I-STOP implementation in New York, they’re approaching 90 percent penetration. When nationally you’re at 14 and New York is at 90, you can see the digitization that has occurred.
Digitizing those prescriptions is an important part of allowing people to do the analysis they need to do. If society as a whole decides that we need to do more behavioral work to support those patients, or whatever it is that we decide to do to treat them, the sooner we can help recognize it, the better. This problem is not going away without some type of intervention.
Do you have any final thoughts?
You asked a great question. Where are we on the road to interoperability? Should we be positive about it? Should we be concerned? What I would say is that there’s a huge amount of work to do, There needs to be an appropriate amount of focus on that work. There’s also a huge amount of progress that has been made, and will be made in the future.
I continue to be optimistic that with the combination of private entities partnering, and then private entities partnering with the public interest at the state and federal level, you’re going to see continued progress and acceleration over the course of the next few years. It’s not a panacea, but I think it’s going to be very positive and will have a huge impact. Patients and all of us US citizens are going to benefit enormously.
Comments Off on HIStalk Interviews Tom Skelton, CEO, Surescripts







































Traditionally Professional Courtesy is something that physicians gave each other - but we had to be careful with it when…