Chris Klomp is CEO of Collective Medical of Draper, UT.

Tell me about yourself and the company.
Collective Medical is a Salt Lake City-based developer of collaboration software. I started working on the company with two of my best friends from Boise, Idaho. We grew up together and we all went to Brigham Young University together. Two of us studied computer science and I was the token business guy. I went off to Bain & Company and then Bain Capital for roughly a decade.
One of our moms, Patti, is a social worker in the emergency department. She had been working on complex patient care coordination, particularly for patients who move across emergency departments. She had hypothesized that not only was this happening, but that a subset of those patients was probably opioid-seeking. Nobody talked about that 15 or 20 years ago, so she was pretty prescient on the ground.
The guys didn’t want to go work for “the man.” Patti, who is a pretty intimidating and awesome lady, told them to “build a computer program” for what she was doing in a circulated Word document and they did. They won a couple of business plan competitions and decide to take it out to the world. It took a lot of years and a lot of bootstrapping, but off we went.
My dad was a physician who told me that healthcare is the highest calling, so that’s what I wanted to do in some form. I had a bit of circuitous path, but I found my way back and we’ve been doing that since.
Collective Medical builds collaborative care networks. We help disparate stakeholders across the continuum — emergency, inpatient, skilled nursing facilities, mental health stakeholders, and even health plans and ACOs with their care managers – become aware when a patient needs them, particularly those vulnerable members who have figuratively fallen. We then unify their records collectively and help pick that person up.
How do you see the company fitting into the interoperability landscape?
We’re attacking from a different direction. I’m not sure I would even classify what we do as carte blanche interoperability. Interoperability is principally concerned with moving data from Point A to Point B. There are a number of pathways by which that’s taking place.
Health information exchange has made tremendous advancements, particularly in the last several years, in linking communities together to unify a care record. There’s a lot more work still to be done, but they’re making great strides. You have the networks like CommonWell and Carequality that are doing that with CCDs and certainly have ambitions to do more. You have platforms like Epic Care Everywhere that are, in some regards, even more advanced in how they link data from Point A to Point B and unify that into a single patient record.
The world is focused on these opportunities for good reason, but it’s a necessary but insufficient condition of driving coordination across an otherwise highly fragmented set of providers in a landscape. We have data silos and we need to unify those. We should have a single patient record that isn’t replicated with duplicative tests or because a patient goes from one site of care to another. However, it’s highly unlikely that the entirety of the country is going to be comprised of organizations like Kaiser, Intermountain, and Geisinger. Even those organizations — and I can say this because Kaiser and Intermountain are among the owners of our company — still have affiliated providers that they don’t own and that aren’t on their same record of care. They still require collaboration and coordination across those disparate providers.
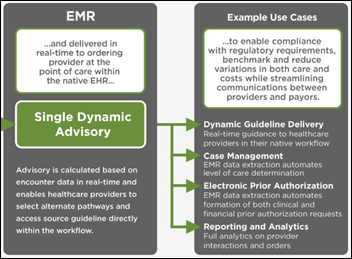
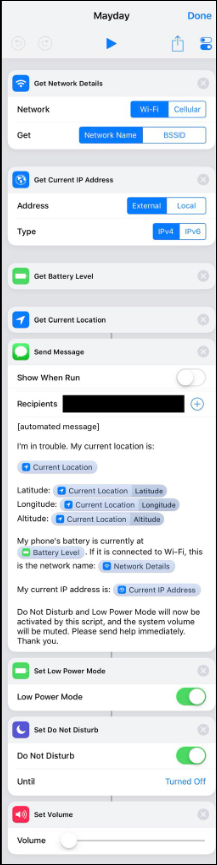
You can either throw a tremendous number of expensive, scarce bodies at the problem, which isn’t scalable, or you can use technology. I’m not talking about mere notifications that an encounter has occurred, which we do, but a deeper level of collaboration. A mental health provider in the emergency department creates a crisis plan for the patient at 3:00 in the morning that involves a primary care provider who is affiliated with a multi-specialty clinic that is not connected to the health system and a Medicaid managed care manager. How do you help those individuals get on the same page and interact with the patient in sequence so that we’re not wasting resources or missing opportunities to help the patient navigate across the continuum, efficiently using the existing technology infrastructure of each organization? That’s the set of problems that we’re focused on.
Notifications are a mechanism to gain provider attention or to nudge them to intervene to mitigate an identified risk. But your phone has 15 notifications an hour popping up and most of that is noise. The more that we can increase the fidelity of those notifications and distill signal from that noise to make them actionable, the better.
Patti’s original work involved competing hospitals sharing her Word document, which was probably shockingly collaborative back then. Is the questionable business case for broad interoperability a non-issue when the addressed problems are overuse of opiates or EDs, which are in nobody’s best interest?
The premise of our business is that bad people don’t go into healthcare. That’s true even with the big, bad health plans that sometimes get painted into a corner. I’m not suggesting that there aren’t disagreements or even mistrust in healthcare and I’m sure there can be tense moments during contract negotiations between a health plan and a health system. But our job is to find the opportunities where there’s an alignment of incentives. When good people are reminded of why they joined up in healthcare and what their true purpose is, those instincts of competition or mistrust that might lead them to not want to share data fall away. When you give them a cause or a reason to collaborate, people will rally.
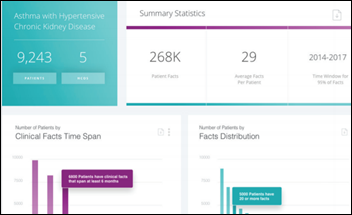
Let’s say we have a low-income, low-acuity pediatric asthmatic patient who’s bouncing around emergency departments. Nobody’s looking to increase their volume by having that patient coming to their hospital. The health plan, the Medicaid ACO or MCO, and the pediatrician, pediatric pulmonologist, or emergency department physician all have a perfectly aligned set of incentives to get that patient into the most appropriate care channel, stabilize them, and help them lead a healthy life. What level of interoperability and coordination is required to restore that child to a point of health?
How will Virginia’s statewide ED collaboration project work?
Our objective is to connect healthcare at scale. Virginia is a perfect example. You have 130-some hospitals and health systems, hundreds of post-acute operators, and thousands of ambulatory providers across the state, along with Medicaid, Medicare, and commercial health plans. The state’s objective was not only to reach a level of interoperability in terms of data sharing, but even more so, to reach a level of collaboration to manage down medically unnecessary utilization, avoidable friction, or risk.
The state evaluated a number of different paths and vendors and ultimately partnered with us. In five months, we connected 100 percent of the state’s acute care hospitals. We brought on all of the managed Medicaid organizations. In the next wave, we’re onboarding skilled nursing facilities and non-Medicare and other ACOs. We’re beginning to bring on ambulatory providers as well.
The state of Virginia had phenomenal leadership and vision. They didn’t just talk about interoperability that could move data from A to B. They’re goal was real coordination. It’s called the EDCC — Emergency Department Care Coordination — initiative because it starts in the emergency department, the front door of the healthcare continuum for so many vulnerable patients. Virginia is seeking to instantiate workflow broadly out into the rest of the community. Not just through interoperability, but by actually prompting coordinated sequences of engagement of various providers across specific patient archetypes to drive resolution.
Interoperability is the base layer. Then, how do we use data to coordinate human behavior? We make it easier for them by meeting them in their workflow, not making them go look up information. They can understand which of their patients are at a place of need and coordinate with others who can help meet the needs of that individual, to lift them up and catch them before they fall.
How will the company’s momentum or direction change following the large fundraising you completed a year ago?
We bootstrapped the business for most of our history. We aren’t a non-profit, but we’ve effectively run it that way. We don’t dividend out proceeds. The principals haven’t taken raises and draw pretty nominal salaries.
Our goal now is to invest in the platform and to grow networks. Building network effect-enabled platforms is capital intensive because you need to reach critical density in a given geography to create value for the constituents there. We’ve done a pretty good job of that. We’re live in 17 states, not just with one or two hospitals, but penetrated broadly to 100 percent of acute hospitals. We’ve got a bunch more in the hopper.
We realized that while bootstrapping a company gives you tremendous autonomy to do the right thing, it’s a rate limiter to growth. Building a network effects-enabled platform hasn’t been previously done at scale in healthcare. We raised capital to accelerate our growth across the country, to deepen our technical capability with significant R&D dollars, and to gain partners who can help us think through these things since this is our first rodeo.
Our whole point is to act as a rising tide. It’s not to give any individual health system a competitive advantage — which isn’t to say they can’t find it by using our software — but our goal is to help communities lift up their most vulnerable patients. We think about the entire country as that community.
Comments Off on HIStalk Interviews Chris Klomp, CEO, Collective Medical











































I'm generally in favor of fairness and withholding judgment. However, in the context of the Oracle EHR's $100b of waste,…