Access

Booth 3571
Contact: Mike Kelley, VP of sales
mike.kelley@accessefm.com
314.330.5021
Paper-based consent forms (especially informed consents) and other paper-based processes cause all sorts of problems. Simply put, Access EForms solves your paper challenges with an EHR-integrated and tablet-enabled electronic form and e-signature experience. We spend most of our time figuring out how we can more deeply integrate our solutions into your EHR UI and workflow to make life easier for you and your team. Come find us at booth 3571 and we’ll show you what your paperless future looks like.
Bernoulli Health

To arrange a meeting, contact Sam Larson.
Contact: Sam Larson, VP of marketing
slarson@bernoullihealth.com
203.877.1999
Bernoulli is the leader in real-time solutions for patient safety, with more than 1,200 installed, operational systems. Bernoulli One is the market’s only real-time, connected healthcare platform that combines comprehensive and vendor-neutral medical device integration with powerful middleware, clinical surveillance, telemedicine/virtual ICU, advanced alarm management, predictive analytics, and robust distribution capabilities into ONE solution that empowers clinicians with tools to drive better patient safety, clinical outcomes, patient experience, and provider workflow. For more information about Bernoulli One, visit www.bernoullihealth.com.
Black Book Research

To arrange a meeting, contact Doug Brown.
Contact: Doug Brown, managing partner
Doug.Brown@BlackBookMarketResearch.com
727.463.7806
Bluetree

Booth 2187
Contact: Ryan Hill, marketing manager
rhill@bluetreenetwork.com
651.380.3713
We’re an Epic-focused consulting firm making a meaningful and measurable impact in healthcare. Based in Madison, WI, our more than 250 employees work from coast to coast and help customers maximize return on their Epic investments with an integrated approach. We help our customers get there by enlisting an end-to-end delivery process that taps into our 50/50 blend of operational and Epic experts.
Promotion: For every badge we scan, we’re donating one tree in our booth visitors’ names to the National Forest Foundation. We’re also co-sponsoring a networking reception with Instamed at Blue Martini on Tuesday from 6:30-10:30pm, and hosting an in-booth Happy Hour on Wednesday from 3:30-5:30pm.
Cantata Health

Booth MP65
Contact: Neil Taurins, VP of sales
Neil.Taurins@cantatahealth.com
512.917.9819
Cantata Health provides RCM and EHR solutions for acute, post-acute and long-term care facilities. With efficient, flexible, and modern solutions, Cantata Health guarantees to improve patient visibility throughout the continuum of care while increasing your bottomline.
Cantata Health will host a cocktail reception at the Hilton Orlando on Wednesday, February 13 at 7pm. Please contact Neil Taurins to join.
Ciox

To arrange a meeting, contact Cindy Bagley.
Contact: Cindy Bagley, marketing director
marketing@cioxhealth.com
800.737.2585
Every record represents a real person. Each data point is a potential game-changer in someone’s life – a connection to be understood and acted upon. And so our goal is to enable greater health by improving the way health information is managed. For 40 years, Ciox has advanced the healthcare industry through better health information management and exchange of health information. Our broad reach in medical records extends across industries, allowing us to modernize workflows, facilitate access to clinical data, and improve the accuracy and flow of health information. We help our clients manage, protect, and leverage health information to achieve operational improvements, optimized revenue, and better patient outcomes.
Clinical Architecture

Booth 3973
Contact: John Wilkinson, EVP of sales & partnerships
john_wilkinson@clinicalarchitecture.com
317.580.8417
Founded in 2007 by a team of healthcare and software professionals, Clinical Architecture is the leading provider of innovative healthcare IT solutions focused on the quality and usability of clinical information. Our healthcare data quality solutions comprehensively address industry gaps in content acquisition and management, content distribution and deployment, master data management, reference data management, data aggregation, clinical decision support, clinical natural language processing, semantic interoperability, and normalization.
CloudWave

Booth 4107
Contact: Christine Mellyn, director of marketing
cmellyn@gocloudwave.com
781.636.8169
CloudWave is the healthcare cloud transformation company. We create solutions that embrace the full cloud continuum – from the Cloud Edge, to managed private cloud services in our OpSus Healthcare Cloud, to seamless federation with public cloud services like Office 365 and Microsoft Azure. CloudWave’s focused portfolio of OpSus Healthcare Cloud services includes hosting over 100 healthcare applications, disaster recovery, systems management, security, backup, and archiving services. CloudWave architects healthcare IT solutions with the goal of operational sustainability. Our engineers and consultants have long-standing, successful track records designing and implementing solutions for hospitals. Stop by booth 4107 to charge your device, enjoy a cup of coffee, and learn more.
Collective Medical

Booth 888, Kiosk 12 (Personalized Health Experience Pavilion)
Contact: Kat McDavitt, chief marketing officer
kat.mcdavitt@collectivemedical.com
610.392.4726
Collective Medical empowers care teams to improve outcomes by closing the communication gaps that undermine care. With a nationwide network engaged with every national health plan in the country, hundreds of hospitals and health systems, and tens of thousands of providers, Collective Medical’s system-agnostic platform is trusted by care teams to identify at-risk and complex patients, and facilitate actionable collaboration to make better care decisions and improve outcomes.
Based in Salt Lake City, Collective Medical is proven to streamline transitions of care, improve coordination across diverse care teams, and reduce medically unnecessary readmissions.
At 3:45pm on Tuesday, February 12 in the Personalized Health Experience Pavilion, Collective’s head of product, Mandira Singh, will give a talk titled, "Collaboration as a Radical Approach to the Opioid Epidemic." At 4pm on Thursday, February 14 in room W206A, Benjamin Zaniello, MD Collective’s CMO and Beth Landon, the New Mexico Hospital Association’s head of policy, will present a session titled, "New Mexico Reduces Avoidable ED Visits with Technology."
ConnectiveRx

Booth 921
Contact: Mark Mosebrook, senior director, EHR business development
marketing@connectiverx.com
908.809.6100
ConnectiveRx is a leading, technology-enabled life sciences company that improves lives by simplifying how patients get on and stay on therapy to maximize the benefits of specialty and branded medications. We work with biopharmaceutical manufacturers, EHRs, pharmacy systems, and others to help patients afford medications, increase adherence, and simplify the patient-provider experience. We do this by leveraging our technology-enabled services to accelerate speed-to-therapy, and by expertly navigating the complexities in accessing innovative therapies and improving outcomes. Based on our experience pioneering copay programs, managing awareness/adherence communications, and establishing a state-of-the-art hub service, we help our customers overcome barriers to access and use so patients can experience better health. Visit us at booth 921 to experience our interactive digital roadmap detailing how we touch each critical stage of the patient journey.
CoverMyMeds

Booth 3278
Contact: Angela Masciarelli, PR manager
amasciarelli@covermymeds.com
614.360.1735
It all started with a question: “Why won’t my health plan cover my meds?” This was the catalyst of an idea to create a solution that enables providers and pharmacists to electronically manage their prior authorization requests. The CoverMyMeds platform was created to provide a solution that benefits all areas of the healthcare network. As a result, growth in one area of the business adds value to every other part of the network. In fact, in 2018 alone we saved providers $109 million by keeping staff off fax and phone.
Learn how you can be a part of this ever-growing network of more than 700,000 providers, 62,000 pharmacies, and payers representing 94 percent of US script volume to answer the next big question: “How do I get my patients the medications they need at a price they can afford?”
Come visit CoverMyMeds at HIMSS19 to learn more about our solutions that help patients get the medications they need to live healthy lives. There is also a Twitter Machine at the CoverMyMeds booth that dispenses exciting prizes that will "knock your socks off!"
Culbert Healthcare Solutions

Contact: Brad Boyd, president
bboyd@culberthealth.com
781.935.1002, Ext. 113
Culbert Healthcare Solutions provides high-value, professional services focused on improving clinical, operational, and revenue cycle performance, and the overall patient experience. Our experienced healthcare professionals help group practices and hospitals optimize technology and navigate the change management process. For more information about Culbert Healthcare Solutions, visit www.culberthealth.com.
Datica

Booth 621
Contact: Laleh Hassibi, VP of marketing
laleh@datica.com
888.377.3184, Ext. 725
Get through the maze of compliance and onto the cloud faster with Datica. Whether your biggest challenge right now is integrating your digital health product with a hospital or getting through a 2019 HITRUST audit, our products can help.
Visit Datica at booth 621 to see demonstrations of Compliant Kubernetes Service, Compliant Managed Integrations, and our newest SaaS product, the Cloud Compliance Management System. Reserve a demo spot ahead of time and get a MiiR cup or a copy of our new book, “Complete Cloud Compliance” at the show. You can also see a demo of Datica in the Microsoft booth or listen to a presentation on preparing for a 2019 HITRUST assessment in the AWS booth.
Definitive Healthcare

Booth 2770
Contact: Aly Scott, CMO
ascott@definitivehc.com
617.821.9200
Join Definitive Healthcare at both 2770 for HIMSS19! Definitive Healthcare delivers a best-in-class data and analytics platform on healthcare providers for unmatched sales and marketing intelligence.
This is a big year for Definitive Healthcare at HIMSS: As of January 2019, Definitive Healthcare acquired the data services business and assets of HIMSS Analytics, including their Logic, Predict, Analyze, and custom research products. With this acquisition, Definitive Healthcare further bolsters its leading market intelligence platform, which already helps thousands of customers successfully engage with healthcare providers and advance industry efficiencies and best practices.
Looking for more reasons to visit our booth? Enjoy our beer keg and enter to win a free Oculus Rift Virtual Reality Headset. To arrange a meeting or software demonstration with a Definitive Healthcare representative at HIMSS19, book a time in Calendly.
Giveaway: Please visit our HIMSS booth (2770) to grab a beer from our keg and enter to win an Oculus Rift Touch Virtual Reality Headset.
Diameter Health

Booth 8441 and in the Interoperability Showcase
Contact: Tom Gaither, VP of marketing
tgaither@diameterhealth.com
781.249.9475
Diameter Health enables clinical insight through the normalization, cleansing, de-duplication, and enrichment of clinical data from across the care continuum. This creates a single, unified source of longitudinal, structured patient information for improved care and actionable analytics. The Diameter Health platform empowers organizations that depend on multi-source data streams, such as HIEs, ACOs, health systems, and health plans to realize greater value from their data. Visit us at booth 8441 to see a demo of our technology, and discuss the challenges and opportunities of clinical data standards. Pick up a free mobile phone wallet when you mention HIStalk.
Dimensional Insight

Booth 4358
Contact: Priscilla Ballaro, director of marketing
pballaro@dimins.com
781.229.9111
Every member of your healthcare establishment has a critical mission that may feel impossible. Dimensional Insight invites you to meet with us at HIMSS19 to share your daily challenges so that we can make your mission possible with the KLAS award-winning Diver Platform. Visit us at booth 4358 to gather intelligence on how to explore and use your data to make confident decisions, as well as to be entered in a raffle to win an Echo Show.
Direct Consulting Associates

To arrange a meeting, contact David Duggan.
Contact: David Duggan, account manager
dduggan@dc-associates.com
440.371.7783
Direct Consulting Associates is the relationship-focused executive search and contract staffing firm that assists top-tier organizations with recruiting and acquiring high-impact HIT talent for mission-critical technology initiatives. We are constantly in contact with hiring managers, candidates, and opportunities across the healthcare IT space.
EClinicalWorks

Booth 149
Contact: Laura Bujnowski, sales
sales@eclinicalworks.com
508.836.2700
Come to booth 149 to see how EClinicalWorks is transforming healthcare IT, with leading-edge products and services for ambulatory and specialty practices, urgent care facilities, ASCs, health centers, and hospitals. Our intuitive EHR lets providers document on the device of their choice. The EClinicalWorks Virtual Assistant and EClinicalWorks Scribe are streamlining workflows and helping reduce the risk of physician burnout. Our interoperability solutions deliver the most up-to-date patient information, on demand and at the point of care. EClinicalWorks strengthens patient engagement with kiosk check-in, Healow apps, and Healow TeleVisits. Our solutions for population health include data analytics and dashboards to improve planning and close care gaps. And Healow Insights automates the sharing of clinical records and supplemental data between providers and payers to streamline quality reporting. Together with our 15,000+ customers, EClinicalWorks is promoting patient safety, healthier societies, and understanding of the healthcare challenges and opportunities of the 21st century.
Ellkay

Booth 3671
Contact: Ajay Kapare, VP of marketing & strategy
ajay.kapare@ellkay.com
201.808.9128
Ellkay is a recognized healthcare connectivity leader, providing solutions and services nationwide. With 16 years of industry experience, Ellkay empowers hospitals and health systems, diagnostic laboratories, EHR/PMS companies, ACO and HIE companies, and other healthcare organizations with cutting-edge technologies and solutions. With over 50,000 practices connected, Ellkay’s system capability arsenal has grown to over 700+ EHR/PMS systems across 1,100+ versions.
At Ellkay, we are committed to making interoperability happen and are focused on innovation. Stop by our HIMSS booth (3671) to learn how we can help your organization with secure and efficient “data plumbing” for complete data connectivity.
Elsevier
Booth 3331
Contact: Coleen Stilwill, director
C.Stilwill@elsevier.com
404.574.9189
Elsevier enables you to make faster and better decisions throughout the patient journey. Our expert content and technology solutions help you to turn information into actionable knowledge to drive improved outcomes and more cost-effective care. Stop by our booth to:
- See an exciting virtual presentation: “Achieving High Quality Care with Next-Generation CDS,” featuring a panel of informatics experts from leading healthcare organizations. Everyone who attends a virtual panel session is entered into hourly drawings to win a Google Home or Oculus Go VR Headset.
- Get product demos for advanced clinical decision support, clinical practice, patient engagement, clinical reference and decision support, and learning and competency management.
- Participate in product development research interviews.
- Find out how to partner with us.
You can also find us at the Interoperability Showcase (booth 9100) and at presentations for Innovation Live, Lighting Sessions, and Personalized Health Experience.
EMDs

Booth 3100 and 9100
Contact: Patrick Hall
phall@emds.com
EMDs combines leading technologies with tailored services to remove operational burden and empower healthcare providers to maximize the impact of their care. Founded by physicians, EMDs brings decades of expertise and understanding to our integrated EHR products, practice management software, RCM solutions, and credentialing services for medical practices and enterprises. With tens of thousands of deployed clients across a range of specialties and settings, our extensive experience allows us to craft proven, transformative solutions that meet the unique needs of healthcare organizations, enabling unmatched productivity and a superior experience for patients and practitioners alike. Expert Solutions. Stronger Partners. Healthier Patients. Connect with us at www.emds.com and @emds.
To learn more about how Aprima, an EMDs company, can help your practice or organization, visit us at HIMSS19. We will be in the exhibit hall at booth 3100 and in the HIMSS Interoperability Showcase 9100 Hall F. While you’re there, you can see for yourself why our latest acquisition, Aprima EHR/PM has earned back-to-back Best in KLAS awards for both 2019 and 2018 in the Small Practice Ambulatory EMR/PM Category (1-10 physicians) and learn more about how Aria Health Services can meet your revenue cycle needs.
EMDs is participating in the HIMSS Interoperability Showcase. As part of the Clinical Exchange & Price Transparency tour featuring Surescripts National Record Locator & Exchange technology, this showcase is a collaboration of more than six health IT vendors and will demonstrate how EMDs uses interoperability standards to exchange information and improve the quality and value of care provided.
Join us as we follow Angela Davis, a 52 year-old with Rheumatoid Arthritis, as she moves across the country and visits multiple care providers – primary care, specialist, and emergency – in different care settings using multiple EHR technology platforms. Automated processes for clinical information exchange, drug price transparency, electronic prior authorization, and specialty prescribing enable Angela and her care team to make better informed treatment decisions that improve outcomes and the overall healthcare experience.
Where: Hall F – Booth 9100|Tangerine Ballroom
When: Tours of Clinical Exchange & Price Transparency start 15 minutes past each hour
Engage

To arrange a meeting, contact 509.230.8763 or rsvp@thinkengage.com.
Contact: Rich Robinson, director of marketing & account coordination
rich.robinson@thinkengage.com
509.230.8763
Engage is the premier vendor for Meditech application consulting and hardware technical services. Please visit with us during our coffee hour at the NetApp booth (2779), Tuesday from 10-11:30am. Engage is also co-hosting a bourbon tasting with Pure Storage on Tuesday and Wednesday from 2:30-5pm in booth 3827. Please be sure to register for the Meditech Customer Appreciation Celebration Wednesday evening from 7-10pm at Mango’s Tropical Cafe, co-sponsored by Engage. To register, visit: https://www.eventbrite.com/e/meditech-customer-appreciation-event-himss19-tickets-53251735374.
Epsi

Booth 3501 (Allscripts booth)
Contact: Ralph Keiser, CEO
ralph.keiser@epsi.io
512.745.2559
Epsi has launched its new cloud-based Cost Accounting application, the first application on its innovative RealCost platform, architected for the cloud and leveraging Amazon Web Services’ state-of-the-art technology. Epsi has the leading suite of integrated solutions that provide both the tools and knowledge to attain superior financial outcomes. Epsi’s holistic approach includes capital management, operational budgeting, strategic planning, cost accounting, labor productivity, and decision-support modules. Each component contributes to faster identification of fundamental business issues and helps avoid costly missteps. Together, the suite, including the new cloud-based offerings, provides enterprise-wide perspective proven by customer success and awarded for industry-leading innovation.
Experian Health

Booth 2033
Contact: Kristen Simmons, SVP of strategy, innovation & marketing
kristen.simmons@experian.com
949.567.7675
HIMSS Educational Session – Continuing Education Credits available. “Dive into the world of data: The intel you need now.” Uplift the patient experience and your business results. Attend one of two 30-minute sessions on February 12 at 4pm or February 13 at 10am. A reception will follow the 4pm session on February 12; drinks and appetizers will be provided.
First Databank (FDB)

Booth 1921
Contact: Scott Ashworth, VP of sales
sashworth@fdbhealth.com
800.633.3453
FDB (First Databank), part of the Hearst Health network, is the leading provider of drug and medical device knowledge that helps healthcare professionals make precise decisions. With thousands of customers worldwide, FDB enables our information system developer partners to deliver valuable, useful, and differentiated solutions. We offer four decades of experience in transforming medical knowledge into actionable, targeted, and effective solutions that help improve patient safety, operational efficiency, and healthcare outcomes.
FDB will be launching Targeted Medication Warnings – our NEW, patient-first approach to medication guidance; and AlertSpace Analytics to help users identify insights to optimize alert management and crowd sourcing optimization opportunities.
We will host a wine and cheese reception in booth 1921, Wednesday, February 13 from 4:30 – 6pm to promote the launch of the Targeted Medication Warnings product (also, visitors may keep the stainless steel stem-less wine glass!). We will serve coffee in our booth throughout the exhibit.
Case study presentations highlighting FDB solutions:
- “Dignity Health Boosts Medication Adherence with SMART on FHIR (Meducation®)” on Monday, February 11 at 3pm at the Rosen Centre in Rosen Centre Grand C.
- “SMART on FHIR Integration to Improve Medication Adherence (Meducation®)” on Wednesday, February 13 at 8:30am at the Orange County Convention Center in W304E.
Formativ Health

To arrange a meeting, contact Mike Demuth.
Contact: Mike Demuth, VP of sales
mike.demuth@formativhealth.com
Formativ Health offers technology and services that enable hospitals and health systems to give their patients a high-touch, consumer-first experience. At HIMSS this year, we’ll demo our Patient Engagement Platform in the Salesforce booth (3311), to show how we can improve efficiency, schedule utilization, patient payments, appointment logistics, and more.
Fortified Health Security

Booth 2889 and 400-67 (in the Cybersecurity Command Center)
Contact: Judy Cooper, director of marketing
fortified@fortifiedhealthsecurity.com
615.600.4002
Join the Fortified Health Security team at booth 2889 or in the Cybersecurity Command Center (400-67) to gain mission-critical insight on the latest vulnerabilities in cybersecurity and details on escalating cyber attacks. Fortified Health Security teams with healthcare organizations to develop dynamic, agile cybersecurity solutions that help our partners proactively mitigate cyber risks, resolve IT performance gaps, and maintain industry-mandated compliance throughout their organization. We offer our clients access to a comprehensive suite of cybersecurity services designed explicitly for the healthcare industry. Our expansive portfolio of strategies include:
- Connected medical device security.
- Data-loss prevention.
- Vulnerability threat management.
- HIPAA risk analysis.
- Security information and event management.
- Penetration testing.
From initial risk assessment to ongoing support (and every step in between), Fortified Health Security’s team of cybersecurity experts helps reduce IT gaps and minimize system risks for seamless, speed-of-light performance at all times. For more information, visit www.fortifiedhealthsecurity.com.
Forward Health Group

To arrange a meeting, contact Cameron Nankivil.
Contact: Cameron Nankivil, corporate development analyst, sales operations associate
cameron.nankivil@forwardhealthgroup.com
608.347.0073
Data + Analytics x Visualizations x Passion = Improved Outcomes. Forward Health Group has a population health management solution that does what it’s supposed to do. It’s a data strategy and analytics platform that’s ahead of the curve. It’s able to measure care effectiveness and optimize networks. It becomes the catalyst for care improvement and is the key to managing risk and being financially successful. This makes real change possible. Fast forward to value-based reimbursement.
Glytec

To arrange a meeting, contact info@glytecsystems.com or 864.370.3297.
Contact: Jeremy Hogg, VP of population health
jhogg@glytecsystems.com
615.268.2392
What can your hospital, health system, or payer organization do, right now, to markedly improve outcomes, safety, and cost of care for patients with diabetes? Partner with Glytec. We offer a turnkey, virtual care program proven to reduce A1C by an average of 2.7 percentage points, saving you an estimated $7,560 per patient (or per member), per year. We combine FDA-cleared technologies with the services of diabetes care management professionals to optimize insulin therapy for your highest-risk patients and deliver the results that matter most – rapid attainment of target blood glucose and sustained reduction in A1C. Our program centers on use of Glucommander Outpatient, a pioneering digital therapeutic (software-as-a-medical-device) able to respond to blood glucose trends in a dynamic, highly personalized, and evidence-based manner to ensure people with diabetes are taking the right dose of insulin at the right time.
Goliath Technologies

Booth 527 (Citrix Ready Partners booth)
Contact: Michael Clark, VP of marketing
michael.clark@goliathtechnologies.com
856.857.5882
Learn how to ensure that patient records are always available with:
- The Industry’s only purpose-built modules for Cerner, Epic, Meditech, and Allscripts EHR systems.
- A single console combining metrics for EHR performance, Citrix performance, and end-user experience.
- Unique products available for purchase directly from Cerner, and allowed to monitor Cerner RHO.
- The only monitoring and troubleshooting tools available from the Epic App Orchard.
- A proactive early warning system that troubleshoots your entire delivery infrastructure, automatically.
Stop by the Goliath Technologies booth to learn why hospitals like UHS, Catholic Health Initiatives, Monroe Clinic, NorthBay Healthcare, and many more trust Goliath to help healthcare IT anticipate and troubleshoot issues before users are impacted. You can also enter our drawing for an Amazon Echo Spot.
HBI Solutions

To arrange a meeting, contact Eric Widen.
Contact: Eric Widen, CEO and co-founder
ewiden@hbisolutions.com
415.350.3140
HBI Solutions was founded in 2011 by a physician, a data scientist, and a healthcare IT business executive who shared a vision of improving health and reducing costs. HBI partners with healthcare organizations worldwide to deliver actionable information that helps providers reduce patient health risks, improve care quality, and lower the cost of care. The HBI Spotlight solution is grounded in clinical care and data science, and the analytic approach and methods are prospectively tested, peer-reviewed, and published in leading scientific and medical journals. Visit HBI online at www.hbisolutions.com.
HCTec

To arrange a meeting, contact Rob Borella.
Contact: Rob Borella, VP of marketing
rborella@hctec.com
615.786.9496
Join us at The Pub for the Tennessee HIMSS Chapter reception on February 12 at 5:30pm. Email info@hctec.com for further details and an invitation.
HealthCast

Booth 4114
Contact: Rachel Stephenson, event and social coordinator
rstephenson@identityautomation.com
281.220.0021
Identity Automation helps healthcare providers enhance clinical workflows, improve patient care, and embrace security. For over 20 years, HealthCast has designed innovative clinical workflow solutions purpose-built for healthcare’s mission-critical environments. Now, with Identity Automation’s acquisition of HealthCast, our complete portfolio of identity and access management (IAM) solutions offer a better alternative for addressing healthcare’s regulatory, identity lifecycle, and integration challenges. Identity Automation operates globally, with tens of millions of identities managed across on-premises and cloud resources.
Identity Automation will be featuring our award-winning HealthCast product line alongside our RapidIdentity IAM solution in booth 4114. Stop by to demo our solutions and be entered for the chance to win discounts and free licenses for ExactAccess, QwickAccess, EPCS, and Remote Access.
Stop by our booth for a demo and you will be automatically entered for a chance to win:
- 500 ExactAccess one-year subscription licenses.
- 250 EPCS one-year subscription licenses (existing customers only).
- Remote Access for 250 users.
- Fifteen-percent discount on a one-year subscription license of QwickAccess (with a pre-scheduled demo).
- A Peleton bike.
- Plus many more booth giveaways you’ll have to come by to receive!
Need a new headshot for your LinkedIn profile? We’ll provide free, professional headshots in booth — no demo required!
Healthfinch

Booth 2790
Contact: Dawn Burke, director of marketing
dawn@healthfinch.com
608.561.1844, Ext. 17
Healthfinch develops the Charlie Practice Automation Platform, which helps organizations reduce provider burnout, improve quality metrics, and enhance patient satisfaction. Charlie seamlessly integrates with EHRs to automate routine, repetitive workflows, allowing clinicians to spend more time on direct patient care and less time performing non-reimbursable, below-license busywork. Learn more at healthfinch.com.
Please visit us at the Allscripts booth at 12pm on Tuesday, February 12 for a fireside chat with Healthfinch founder Jonathan Baran. Afterward, Healthfinch will host an in-booth happy hour from 4-6pm. Visit with the Healthfinch team at booth 2790. To schedule a meeting during HIMSS, please email sales@healthfinch.com with your availability.
Healthwise

Booth 4449
Contact: Bruce Hedemark, account executive
BHedemark@Healthwise.org
208.331.6936
Since 1975, our singular mission has been to help people make better health decisions. The Healthwise mission, combined with our innovative spirit, leads to health education, technology, and services that power patient relationships. From the point of care to coordinating patients beyond the clinical setting, Healthwise easily embeds within existing workflows to deliver enterprise-wide solutions. Patients access relevant health education wherever they are, on any device.
Iatric Systems

Booth 400-61 (Hall A – Cybersecurity Command Center)
Contact: Judy Volker, marketing director
judy.volker@iatric.com
978.805.3191
Secure remote access. Protect patient privacy. Hacking was named the #1 health technology hazard of 2019 by ECRI Institute. And internal users still cause 56 percent of healthcare breaches, according to Verizon’s 2018 Data Breach Investigation Report. Come to our kiosk in the Cybersecurity Command Center to learn how hospitals are securing remote access and successfully reducing patient privacy threats. Be sure to attend our 20-minute case study presentation, “Confront Internal & External Threats,” on Wednesday, February 13 at 10:15am in Cybersecurity Theater 2.
IMO

Booth 4859
Contact: Dennis Carson, director of tradeshows and events
dcarson@e-imo.com
314.308.3378
IMO is the most-widely used terminology service for EHRs with over 4,500 hospitals and 500,0000 clinicians relying on it every day. IMO provides over 1.5 million diagnoses descriptions and code mapping, ensuring that the patient encounter is accurately documented with the correct terms and billing codes.
IMO Lightning Session: “A Smart Solution for Cumbersome EHR Problem Lists: A Case Study,” with Shaun Miller, MD, associate CMIO, Cedars-Sinai, February 12 at 3:15pm in Hall D, booth 7145.
Wine in the booth: Join IMO for a glass of wine in one of our unique tumblers February 12 and 13 from 4:30 – 6pm in booth 4859. Toast Valentine’s Day with IMO on Thursday, February 14 from 12-2pm.
Booth presentation: “HIMSS19 Tales from the CPO Trenches” on Wednesday, February 13 at 3:30pm in booth 4859. Hear from two battle-hardened chief product officers – one from a large and prominent healthcare system in Southern California and the other from a dynamic and rapidly growing technology firm in the EHR space. This is a facilitated discussion covering industry, healthcare delivery, and innovation at Cedars-Sinai, and how tech companies can work best with large provider organizations. Both will address the future of health IT, so it’s well worth the time. Open to all HIMSS19 attendees, this is of value to provider organizations, CMIOs, CNIOs, CIOs, CEOs, and director-level hospital executives.
Imprivata

Booth 2959
Contact: Kerry Pillion, director of corporate communications
kpillion@imprivata.com
781.761.1452
Think Healthcare. Think IT Security. Think Imprivata. Only Imprivata offers the most complete end-to end identity and access management platform, purpose-built for healthcare. Visit us at booth 2959 and explore:
- Interactive demos on clinical efficiency, multifactor authentication, EPCS, and patient identification.
- Revealing stories on healthcare solutions presented by your peers, while you relax in our theater.
- Thought-provoking insights into the future of healthcare security and more global regulatory changes.
Learn more at https://www.imprivata.com/himss19.
Leidos

Booth 1209
Contact: Matt Maloney, director of marketing
matt.maloney@leidoshealth.com
317.908.8345
Stop by the booth to discover how we are helping healthcare organizations improve patient care, optimize clinical workflows, improve financial performance, and enhance public health as part of our mission to help create a healthier world. Stop by for a chance to win a drone.
LiveProcess

To arrange a meeting, contact Terry Zysk.
Contact: Terry Zysk, CEO
tzysk@liveprocess.com
603.759.1221
Born in the crisis-oriented world of emergency management, LiveProcess has more than a decade of success enabling large and complex networks to plan for and respond to critical, catastrophic, and time-sensitive incidents. We now bring our proven logistics and coordination expertise across healthcare settings, within and beyond hospital walls, enabling personnel to take control of situations and collaborate to resolve operational disruptions, urgent healthcare needs, and routine transitions in patient care. Headquartered in Chelmsford, MA, more than 650 healthcare organizations and public agencies rely on LiveProcess’ unmatched mobile SaaS solutions to effectively manage, analyze, and respond to changing conditions. Learn more about our approach to emergency management and clinical communication and coordination on our blog at www.liveprocess.com/blog.
Loyale Healthcare

To arrange a meeting, contact Michael Morrison.
Contact: Michael Morrison, chief marketing officer
michaelm@loyale.us
406.868.9179
Loyale Healthcare is committed to a mission of turning patient responsibility into lasting loyalty for its healthcare provider customers. Based in Lafayette, CA, Loyale and its leadership team bring 27 years of expertise delivering leading financial engagement solutions for complex business environments. Loyale currently serves approximately 2,000 healthcare providers across 48 states. Loyale recently announced an enterprise-level strategic partnership with Parallon, including deployment of its industry-leading technology to all HCA hospitals and physician groups nationwide.
Loyale Healthcare will have several specialists in attendance at HIMSS this year. We’re not exhibiting this year, but we are eager learn more about your patient-pay challenges. Loyale Patient Financial Manager is the industry’s leading end-to-end patient financial engagement platform. Let’s see if we can make a difference for your patients and your bottom line. Interested in learning more? Contact Michael Morrison, CMO, at michaelm@loyale.us or 406.868.9179. We’ll gladly make arrangements for a conversation at this year’s HIMSS conference. We look forward to seeing you there.
MDLive

Booth 6979
Contact: Michelle Rider, SVP of marketing
mrider@mdlive.com
972.345.6400
MDLive is delivering the future so you can deliver the best digital telehealth patient care today. The future is here. Instant communication, world-wide connectivity, new concepts, cutting-edge technology, and the upheaval and overthrow of past paradigms. How do you manage, let alone stay in the forefront, of consumers’ demands and shifting utilization? We are your partner in the digital healthcare space. We’ve perfected a frictionless patient experience, created superior telehealth professional services, designed varied market solutions, will support you with specific adoption and buy-in strategies, offer interoperability, and are Medicare and Medicaid plan experts.
What you can learn and do at the MDLive booth:
- Talk to a sales representative.
- Learn about the exciting new offerings we are adding to our suite of products and services for 2019.
- Experience a demo of the platform.
- Learn about MDLive Engage for driving utilization at your health system.
- Talk with our CMO about joining our network of providers.
Giveaways: We are giving away many prizes at our booth. Scan your badge for a chance to win an Apple Watch.
Medhost

To arrange a meeting, contact Brian Grant.
Contact: Brian Grant, senior director of marketing
brian.grant@medhost.com
615.761.1998
Medhost has provided products and services to healthcare facilities of all types and sizes for 35 years. Today, more than 1,000 healthcare facilities are partnering with Medhost and enhancing their patient care and operational excellence with its clinical, financial, and operational solutions.
Whether you are a clinician, an administrator, or work in healthcare IT, Medhost has a solution with you in mind.
The Medhost Healthcare Hero Utility Belt includes:
- Fully integrated EHR.
- Emergency department information system.
- Hosted and managed solutions.
- Revenue cycle solutions and services.
- And exceptional customer support and implementation services.
For more information about Medhost solutions and services, visit www.medhost.com.
Medicomp Systems

Booth 3901
Contact: James Aita, director of business development
jaita@medicomp.com
647.207.0080
Medicomp Fixes EHRs Where They Hurt – Experience the Medicomp Cure in Booth 3901. Are you suffering from EHR aches? Disorganized data? Quality quandaries? Medicomp has the cure. Isn’t it finally time to fix your EHR AND win prizes? To learn more, play our OpEHRation Game and see our solutions in action. Plus, we’re giving away $100 to a lucky winner every 30 minutes. To reserve your space to play OpEHRation or to schedule a 15-minute demo with the Medicomp team, visit www.medicomp.com/himss19. If you have any questions, please email himss@medicomp.com.
Also, you’re invited to join Medicomp and Phoenix Children’s Hospital on Tuesday, February 12 at 1:30pm in room 311 for “Enhancing Patient Care with Physician-Driven Documentation at Phoenix Children’s Hospital,” presented by Vinay Vaidya, MD CMIO and VP at Phoenix Children’s Hospital, and Michael Shishov, MD a practicing pediatric rheumatologist. Can’t make the live session on Tuesday? Join us in our booth for a Q&A with Phoenix Children’s on Tuesday at 4pm. Refreshments will be served.
Meditech

Booth 3921
Five decades. One EHR. No limits. More than ever, Meditech’s reputation for excellence resounds across every care setting. As we celebrate 50 bold years of vision and innovation, we invite you to see healthcare through a whole new lens with Expanse, the premier EHR for the digital healthcare paradigm. Our cutting-edge solutions help organizations and providers all over the world to take on the challenges of healthcare’s ever-expanding landscape. Come see the latest solutions Meditech Expanse offers for engaging patients, improving clinical workflows, adapting to value-based care, and much more.
You’ll also get to see clinicians demonstrating our solutions LIVE, showing how you can reclaim your productivity. Hear from industry experts in Meditech booth 3921, and learn to work more efficiently, access information faster, build stronger relationships with patients, and more!
Join our #HIMSS19 Tweetup on Tuesday, February 12 at 12:30pm to discuss "The Nurses’ Voice: Incorporating Nurse Feedback to Improve Care."
Midmark RTLS

Booth 2909
Contact: Stephanie Bertschy, senior marketing manager
SKBertschy@Midmark.com
231.313.8564
Better care doesn’t happen by chance. It happens by design. To help you design better care in your health system, Midmark provides a complete, connected ecosystem of solutions. Fueled with accurate data from our real-time locating system (RTLS), thoughtfully designed workstations, diagnostic devices and more, we’ll help you transform your clinical spaces to provide an exceptional care experience for every patient. Midmark RTLS, formerly Versus Technology, uses both precise and WiFi real-time locating system (RTLS) technology to effectively manage mobile assets, enhance safety, and improve patient flow. Let our lean workflow consulting, implementation services, and industry-leading location accuracy help you improve the delivery of quality care and enhance the patient experience.
Visit the Midmark RTLS booth, 2909, for LIVE demonstrations featuring a fully operational patient flow system, along with new software options that make it simpler than ever to optimize patient flow. Want to know more? Don’t miss the following session by a client who has experienced first-hand the benefits of RTLS, improving exam room utilization by 67 percent, despite moving to a facility with 40-percent less space: “Using RTLS Data to Increase Ambulatory Care Capacity,” with presenter Rodney Haas, VP of operational excellence at the University of Minnesota Health Clinics and Surgery Center, Tuesday, February 12, at 3pm in room W204A.
MModal

Booth 2079
Contact: Lisa Martin, senior manager of marketing
lisa.maritn@mmodal.com
267.535.7222
Join MModal as we showcase our our cloud-based clinical documentation solutions that connect workflows for efficient and accurate medical speech recognition, medical transcription, CDI, and coding. We facilitate physician-patient relationships by making it easy for doctors to capture the patient story, and by delivering information when it is needed most – at the point of care.
National Decision Support Co.

Booth 4185
Contact: Mary LaRusso, director of marketing
mlarusso@nationaldecisionsupport.com
847.345.2648
Join National Decision Support Co. at HIMSS 2019! The HIMSS Global Conference & Exhibition brings together 45,000+ health information and technology professionals, clinicians, executives, and market suppliers from around the world. NDSC, a Change Healthcare company, is the market leader in EHR integrated decision-support solutions. CareSelect leverages our evidence-based clinical standards, analytics, native workflow integration capabilities, and services to enable value-based care and clinical process improvement. Through CareSelect, healthcare organizations identify and eliminate waste and care variation in order to save money and improve quality. CareSelect has facilitated more than 30 million clinical decision support consultations at more than 500 health systems, representing more than 3,000 acute care facilities nationwide. Join us in booth 4185 to find out more. Make your NDSC in-booth appointment today!
Netsmart

Booth 1413
Contact: Cory Harden, business development
charden@ntst.com
913.242.6078
Visit with us at HIMSS19 to learn from one of our experts how Netsmart is going beyond the EHR to integrated care, and enter to win a Roomba!
NextGate

Booth 926
Contact: Mary Molaskey, sales development representative
mary.molaskey@nextgate.com
928.237.2939, Ext. 109
Stop by booth 926 to learn how NextGate can help your organization overcome the clinical, operational, and financial challenges that result from duplicate records and disparate EHR and IT systems. As the global leader in healthcare enterprise patient identification, NextGate’s flagship EMPI platform currently manages patient identities for more than two-thirds of the US population.
During HIMSS19, our executives will be on hand to discuss how NextGate will continue to pave the way for a new era in patient matching and provider data management with advances in geocoding, machine learning, referential data, and mobile application for patient enablement. For every visitor that comes to our booth, NextGate will make a donation to St. Jude Children’s Research Hospital. We’ll double that donation if you pre-schedule a demo or attend one of our SDOH panels on Tuesday, February 12. To learn more about NextGate’s HIMSS19 activities, visit https://nextgate.com/events/himss19 or follow us on Twitter @NextGate.
Nordic

Booth 2579
Contact: Michelle Lichte, EVP of client partnerships
events@nordicwi.com
608.268.6900
NVoq

To arrange a meeting, contact 866.383.4500 or connect@nvoq.com.
Contact: Kristen Ayers, director of marketing
kristen.ayers@nvoq.com
303.304.7021
NVoq offers a variety of healthcare-oriented, HIPAA-compliant speech solutions. Our desktop client, SayIt, works seamlessly with any EHR and is compatible with both PCs and Macs. SayIt offers highly accurate, secure, cloud-based speech recognition technology that saves providers time and money. We also offer a wireless mic and tablet solution. For more information about the NVoq platform, please contact us at connect@nvoq.com.
Obix by Clinical Computer Systems
Booth 8559 (in the Intelligent Health Pavilion)
Contact: John Murray, national accounts manager
john.murray@obix.com
888.871.0963, Ext. 648
Clinical Computer Systems will be exhibiting at HIMSS19 demonstrating the Obix system in the Intelligent Health Pavilion (booth 8559), in the LDR room, and at a kiosk. The Obix system will also be shown in the Interoperability Showcase (booth 9100) as part of the connected demonstration and integrating with Epic in the Mother and Infant Mortality Prevention use case.
Visit our booths in the IHP and Interoperability Showcase where demonstrations will provide firsthand experience of our integration capabilities and our clinical decision support. Your visit will also provide the opportunity to learn more about our capabilities, whether it be the premises-based Obix system or the Obix Hosted Solution.
Clinical Computer Systems stands out in the industry affirmed by KLAS as the Category Leader in Labor and Delivery nine out of 10 years. As a leader, we never stop seeking innovative solutions. Our commitment to the development of the Obix system is based upon solutions that incorporate changes in technology, regulations, and standards in the obstetrical department to support hospitals’ strategic initiatives. Ultimately, our goal is to provide our customers with software that incorporates the clinical workflow specialized for perinatal care.
OmniSys

To arrange a meeting, contact Scott Warshaw.
Contact: Scott Warshaw, CFO
scott_warshaw@omnisys.com
214.459.2574, Ext. 2577
OmniSys is a technology company that helps pharmacies and pharmaceutical manufacturers drive growth by engaging patients, competing on value and distinguishing their brands. With over 25 years of experience, we leverage our unique market insight, pharmacy workflow expertise, and extensive industry knowledge to deliver valuable solutions to our customers. We provide medical billing, immunization services, and patient communication solutions for pharmacies and consumer engagement programs for pharmaceutical manufacturers that drive value and deliver real results. OmniSys currently serves over 25,000 pharmacies, connects to hundreds of payers, and touches millions of patient lives.
OnPlanHealth by Flywire

To arrange a meeting, contact Patrik Vagenius.
Contact: Patrik Vagenius, VP of sales, healthcare
patrik.vagenius@flywire.com
219.229.5733
Flywire is a Signature Sponsor at the HIMSS pre-conference Revenue Cycle Solutions Summit, where Leslie Richard from CHI will present a 15-minute case study alongside EVP and GM, Healthcare John Talaga. "Owning the Patient Financial Experience In A Consolidated World: A Catholic Health Initiatives Case Study" will be presented on Monday, February 11 at 2:10pm.
Flywire’s healthcare platform was developed in collaboration with hospital partners by the creators of the industry’s first online patient billing solution and is infused with the intelligence and expertise developed over 30 years in the industry. Co-founded and lead by John Talaga, an industry leader who has partnered with hundreds of healthcare providers to develop innovative patient billing and payment solutions, Flywire’s platform offers a complete patient pay strategy that fills the gaps in revenue cycle processes in order to enhance collections while building strong, long-term relationships. Please contact Patrik Vagenius at patrik.vagenius@flywire.com if you would like more information on Flywire’s innovative healthcare payments platform.
Flywire’s OnPlan Health is a full-service patient billing and payment platform that engages patients with responsive payment offers, based on their profile and ability to pay. This creates a personalized, relationship-building financial experience that improves response time to settle balances on mutual terms, reduces patient calls, prevents unnecessary placements to agencies, and increases cash. OnPlan combines accounts into a single view, both online and offline, providing a seamless experience for patients and providers, including the tools that revenue cycle teams need – a robust CRM, automated payment posting, performance analytics and reporting, and payment security and compliance. OnPlan makes it easy for providers to optimize their revenue cycle strategy by integrating seamlessly with any existing systems and processes.
Optimum Healthcare IT

To arrange a meeting, contact Larry Kaiser.
Contact: Larry Kaiser, VP of marketing
lkaiser@optimumhit.com
516.978.5487
Optimum Healthcare IT is a Best in KLAS Healthcare consulting firm based in Jacksonville Beach, FL. We offer expertise in advisory services, EHR implementation, EHR training and activation, security, managed services, community connect, ERP, and ancillary services such as laboratory. We are hosting a Lunch and Learn on “Optimizing Outcomes with Real-Time Data Harmonization” on Tuesday, February 12. Click here to learn more and register.
PatientBond

Booth 4591
Contact: Brent Walker, SVP of marketing & analytics
brent@patientbond.com
513.314.5981
Founded in 2011, PatientBond’s mission is to leverage healthcare consumer insights and innovative technology solutions to help its clients better navigate the rise of consumerism in healthcare and evolving reimbursement models. PatientBond’s highly configurable communications platform leverages a proven psychographic segmentation model developed by healthcare consumer experts from Procter & Gamble to motivate and influence patient/member behaviors. PatientBond supports a diverse set of digital workflows to help our clients build a tighter bond with their patient/member population while improving healthcare consumer acquisition, loyalty, and health outcomes. PatientBond is a portfolio company of First Health Capital Partners. Information about PatientBond is available at www.patientbond.com.
PatientKeeper

Booth 1903
Contact: Kathy Ruggiero, senior director of marketing
kruggiero@patientkeeper.com
781.373.6100
PatientKeeper software optimizes EHR systems to streamline physician workflow, improve care team collaboration, and bolster revenue. Over 400 provider organizations comprising more than 65,000 physicians use PatientKeeper. A
t HIMSS19, PatientKeeper will showcase its integrated software suite including CPOE, medication reconciliation, e-prescribing, clinical documentation, sign-out, and more – and point solutions, such as physician charge capture and clinical communications. In addition, visitors can see PatientKeeper’s joint solutions with Medhost and ShareableForms. Medhost now offers its inpatient EHR customers PatientKeeper’s mobile apps, while ShareableForms is integrating PatientKeeper Charge Capture with its iPad-based EHR lite app.
Giveaway: The first 50 visitors to PatientKeeper’s booth (1903) each day will receive PatientKeeper’s popular “Physicians save lives. I save physicians.” T-shirt.
PatientPing

To arrange a meeting, contact SVP, Head of Growth Brian Manning at bmanning@patientping.com.
Contact: Melissa Palardy, senior marketing manager
mpalardy@patientping.com
401.309.4848
PerfectServe

Booth 1113
Contact: Carlene Anteau, VP of marketing
canteau@perfectserve.net
865.212.6380
PerfectServe (booth 1113) is building healthcare’s most advanced communication and collaboration solution to unify the entire care team across the continuum – from inpatient, to outpatient, to patients at home. The secure platform uses advancements in mobility, AI, and analytics to optimize scheduling, automate clinicians’ communication-driven workflows, eliminate non-clinical tasks, and decrease clinician burnout, resulting in quicker time to treatment and superior patient outcomes. PerfectServe’s scalable cloud-based architecture is not affected by on-site outages, allowing the 500,000-plus clinicians who rely on the platform for clinical communication to focus on delivering the best patient experience possible.
Wrap up your day on Tuesday and Wednesday for Happy Hour in our booth from 4:30-6pm.
PeriGen

We will be at the Qualcomm Life booth 5759
Contact: Mike Espy, strategic account director
mike.espy@perigen.com
773.322.5162
PeriWatch Vigilance is an automated early warning system for labor and delivery. Using artificial intelligence and other analytical techniques, PeriWatch Vigilance notifies clinicians when a patient’s condition is worsening.
Philips

Booth 2101
Contact: Kaitlin Pierce, marketing leader
kaitlin.pierce@philips.com
Philips’ mission is to continuously improve the health outcomes of patient populations through effective insights, monitoring, interventions, and programs. Our portfolio of diverse solutions empowers our customers to deliver care more effectively. By aligning care delivery strategies across the entire continuum of care – from the ICU and the hospital bedside, to out-of-hospital care with remote monitoring programs – we enable a strong collaboration between patients, providers, and payers through interconnected platforms and technologies. Stop by booth 2101 to learn more about how Philips is improving the lives of 3 billion people by 2025.
Phynd Technologies

Booth 975
Contact: Keith Belton, VP of marketing
Keith.belton@gmail.com
978.421.5710
Your providers are your lifeblood. Every step of your patients’ journey – from website to scheduling to discharge to care coordination – requires provider information. Isn’t it time to invest in a platform that manages all employed, credentialed, referring, and affiliated providers … so your operations hum, as you scale? Phynd manages all operational provider data – who your providers are, where they work, their expertise, and what networks they serve. Using Phynd, health systems enroll, manage, report on, and search for providers. Phynd integrates with EHRs, websites, and other systems that depend on intelligently searchable provider data. It powers core processes via easy-to-use provider enrollment, management, search, and reporting. Health system leaders use Phynd … Yale New Haven, Kettering Health Network, Michigan Medicine, UNC Health Care, Duke Health, Orlando Health, and more … 250+ hospitals and growing. Join the crowd! Come by booth 975 to learn more!
Pivot Point Consulting, a Vaco Company

To arrange a meeting, contact Rachel Marano.
Contact: Rachel Marano, managing partner
rmarano@pivotpointconsulting.com
773.633.3448
Pivot Point will have an open meeting space at the Urban Tide Restaurant in the Hyatt (connected to the convention center) with food and drinks. If interested, please contact us via phone 800.381.9681 or email info@pivotpointconsulting, or simply stop by on Tuesday, Wednesday, or Thursday between 9am and 4pm.
Pivot Point Consulting is giving away some amazing gifts as part of our Back to the Future theme for HIMSS19. Win a set of Apple AirPods, a pair of Original Ray-Ban Wayfarer sunglasses, or a Patagonia hip pack. Come to our Tuesday night event at 6pm at Marlow’s Tavern in Pointe Orlando to enter the drawing. We’ll be giving away a prize every hour and you must be present to win. Register here: www.pivotpointconsulting.com/himss19. No vendors, please.
PMD

To arrange a meeting, contact sales@pmd.com or 800.587.4989, Ext. 2.
PMD gives healthcare professionals powerful, intuitive, mobile software that improves patient care. With PMD’s mobile communication, data capture, and care navigation platform, healthcare teams finally have an elegant and simple technology to maximize efficiency and collaboration, capturing everything right at the point of care. PMD interfaces with all major EHRs, hospital systems, and medical billing systems, enabling the efficient sharing of data and cutting down on medical errors. The PMD team is committed to developing the best solution and providing superior customer service. For more information, contact PMD.
PreparedHealth

To arrange a meeting, contact Tim Coulter.
Contact: Tim Coulter, COO
Tim@preparedhealth.com
707.330.7870
PreparedHealth’s solutions safely links hospital case managers with home health aides, skilled nursing facilities, social workers, and other post-acute providers, enabling all parties to share patient information and status reports electronically – and all with the intuitive simplicity of familiar social media platforms like Facebook or LinkedIn. By facilitating a more accurate, real-time exchange of information, PreparedHealth helps patients receive higher quality care as they transition from hospital to home.
Recondo Technology

Living Room #3
Contact: Elyse Lazartic, marketing director
marketing@recondotech.com
303.974.2895
Recondo delivers industry-leading automated, accurate, and actionable financial clarity to all participants within the healthcare revenue cycle. Recognized by Black Book Research as one of the top three leaders in RCM software, Recondo empowers more than 900 hospitals with solutions that connect providers, payers, and patients to ensure proper payments across the care continuum. The company’s patented software and expertise streamline operations and allow providers to be paid more, faster, and at a cheaper cost. Recondo brings efficiencies and cost savings to patient access through to payment processing — a continuum today where inaccuracy and inefficiencies currently cost US healthcare a staggering $480 billion per year.
Promotions: Come get your special pair of Recondo socks and learn about integrating Best in KLAS patient access content directly into your Epic system with RevSmart in HIMSS Living Room #3.
Redox

Booth 7861
Contact: Erin, program manager
paige@redoxengine.com
608.535.9501
Redox accelerates the development and distribution of healthcare software solutions with a full-service integration platform to securely and efficiently exchange data. Provider organizations and technology vendors connect once and authorize the data they send and receive across the most extensive interoperable network in healthcare. Redox exists to make healthcare data useful and every patient experience a little bit better. Learn how you can leverage the Redox platform at www.redoxengine.com.
Join us on Monday night for a Block Party at The Pointe sponsored by Redox, PointClickCare, and ImageMover. RSVP here. Stop by the Redox booth (7861) for demos from our customers at 1pm and 3pm on Tuesday and Wednesday, and at 11am and 1pm on Thursday.
ROI Healthcare Solutions

Booth 4573
Contact: Jason Berry, SVP of sales
jason.berry@roihs.com
678.270.2867, Ext. 201
A Brief Word About ROI: Top Rated KLAS Leader in Business Solutions Implementation and Partial IT Outsourcing. ROI Healthcare Solutions is healthcare’s trusted IT services partner, founded in 1999. We save clients time and money, creating clinical, operational, and financial excellence through ERP and EHR initiatives. ROI offers industry-centric project management, consulting, implementation. optimization, support, and staffing services. Our leadership is committed to delivering quality services with highly engaged team members to clients who appreciate long-term partnerships.
About Our Practice Areas: ROI’s HIS practice focuses on managing, implementing, and optimizing clinical, revenue cycle, technical, and reporting systems such as Cerner, Siemens, AllScripts, McKesson, Epic, and Meditech. We are the top-rated KLAS Partner in Partial IT Outsourcing. We are also a Cerner Preferred Collaborator with multiple resources certified through Cerner’s Revenue Cycle Certification Program. Our core offerings center around project management, legacy support, application management/shared services, data migration/extraction, and decommissioning services. Our proven methodologies are applied to create smooth transitions of people, processes, and systems for healthcare providers across the country. ROI is a CloudSuite-specialized Infor Alliance Partner and KLAS Category Leader that works with providers to reduce costs, increase efficiency, create confidence, and drive success of planning, implementation, and optimization of Infor’s ERP and BI solutions. We give life to our clients’ mission and vision through optimizing processes, people, and technology. We are recognized by both Inc 5000 as a fast-growing private company and Modern Healthcare as the #23 Best Place to Work in Healthcare. ROI has been rated within KLAS Research’s "Partial IT Outsourcing" category, with a current score of 95.7.
ROI will exhibit this year within the largest HIMSS State Chapter Pavilion – Georgia. (Click here to see our exact location within the convention center.) We invite our clients, prospects, and partners to our booth, so we can exchange mutually beneficial information and figure out how we can help one another.
Daily raffles will include gift cards, a Megaboom Speaker, and fun/functional giveaways. We will announce winners each day of the conference, as well as at the Georgia HIMSS Reception on Tuesday, February 12 at 4:30pm in the pavilion.
SailPoint Technologies

Kiosk 400-89
Contact: Matthew Radcliffe, director, healthcare vertical
matthew.radcliffe@sailpoint.com
410.937.2562
SailPoint enables healthcare providers to confidently secure patient data and other sensitive information while improving user access to drive better operational workflows. Recognized by Gartner, Forrester, and KuppingerCole as the leading authority on identity governance, SailPoint delivers modern, comprehensive identity solutions that are central to security, privacy, and compliance. Its technology provides process automations that increase operational and cost efficiencies. Furthermore, SailPoint solutions reduce cybersecurity and compliance risks inherent to manually governing a diverse user population with multiple personas and access requirements across cloud and on-premises environments.
Schedule a private visit in meeting pod 400-105 to discover how smart identity will help your organization optimize workflow while improving security and compliance. You can also stop by to fill out a quick survey to instantly generate your organization’s identity score – an indication of your cybersecurity and compliance risk. We’ll be giving away a $100 Visa Card to each organization who consults with us!
Join us Wednesday, February 13 at 4:45pm in the Cybersecurity Pavilion – Theater B to attend a panel discussion on how smart identity will aid healthcare provider organizations.
Visit SailPoint’s kiosk 400-89 at your convenience for live demonstrations and conversation.
Sansoro Health

Booth 5649
Contact: Kelly Thotland, marketing specialist
kelly.thotland@sansorohealth.com
952.465.7903
Sansoro Health provides powerful, one-stop integration solutions for enterprise health technology leaders so they can rapidly deploy and scale innovative solutions. Sansoro Health believes deeply in the power of innovation and collaboration to usher in the next generation of healthcare. To learn how Sansoro enables integration at the speed of innovation, visit us at booth 5649. At our booth, we’ll have information on the advantages of API integration in healthcare, a Plinko board to play for prizes, and a charging station for your devices to keep you connected at the show.
Also, subscribe to our new 4×4 Health podcast series on ITunes featuring opinions from industry innovators, media, analysts, and clinicians, including Dave Butler, MD, Calyx Health; Ed Marx, CIO, Cleveland Clinic; Don Rucker, former ONC director; Nick Van Terheyden, MD founder and CEO, Incremental Healthcare; Mark Hagland, editor-in-chief, Healthcare Informatics; and Aneesh Chopra, president, Care Journey; as they discuss predictions on the future of healthcare.
Santa Rosa Consulting

Booth 3106
Contact: Gala Wilson, sales & marketing manager
galawilson@santarosaconsulting.com
813.966.1920
Join Santa Rosa Consulting in booth 3106. Acknowledge someone you view as a Healthcare Champion on our #HealthHeroWall and we’ll make a $5 donation (up to $5,000) to one of our favorite charities, Together We Rise. We will also give away conference survival kits filled with the items you need to get through HIMSS.
Our HIMSS19 Speaker Series will help demystify some of the trickier aspects of implementing and continually optimizing your EHR technology. All presentations will take place in our booth. They include, "Test Automation: Defeating the Constraints of Manual Testing," on Tuesday, February 12 at 10:45am; "ELearning: Transforming Apprentices into Masters," on Tuesday at 3pm; "Activation: Assembling the Go-Live Super Team" on Wednesday February 13 at 10am; and "Integration: Nailing the Follow-Through" on Thursday, February 14 at 10am. Visit santarosaconsulting.com/himss19 to learn more and add presentations to your schedule.
Spok

Booth 3371
Contact: Derek Kiecker, solutions advisor
Derek.kiecker@spok.com
952.230.5306
We know you’re on a quest to be a champion of health. To do so, your communication technology needs to integrate with existing workflows in your hospital, and enable you to deliver information to clinicians who need to take action. Top hospitals rely on the Spok Care Connect platform to enhance workflows for clinicians, support administrative compliance, and provide a better experience for patients. Our customers send over 100 million messages each month through their Spok solutions. Spok is making care collaboration easier.
At HIMSS19, we will demonstrate the first phase of our new, cloud-native healthcare communication platform. You’ll find us at booth 3371 and the Interoperability Showcase.
Giveaway: You play — we pay! Locate one of the interactive displays in the Spok booth to play “Pop for a Purpose.” Your goal is to pop as many highlighted bubbles as possible. We’ll donate the dollar amount popped to the charitable organization of your choice (Cancer Research Institute, American Lung Association, or Mental Health America). Make sure to scan your HIMSS badge for a daily chance to win a $500 donation in your name.
Strata Decision Technology

Booth 879
Contact: Rachel Broghammer, marketing coordinator
rbroghammer@stratadecision.com
319.310.8748
Ranked “Best in KLAS” four years in a row, Strata Decision Technology is known for a platform that has emerged as the solution of choice in the market. Our solution, StrataJazz, is the leading, cloud-based SaaS financial planning, analytics, and performance platform in healthcare. We provide seamless integration between our enterprise-wide solution and existing EHR, ERP, and EDW systems to leverage the organization’s existing infrastructure and investments.
We will have an exclusive survey only offered at HIMSS19 for attendees to complete in exchange for a $5 Starbucks gift card. An analysis of the survey results will also be shared with participants. Contact kbores@stratadecision.com to reserve a time to complete the survey, or stop by booth 879 while in Orlando!
We also wrote the book on cost, titled “Margin + Mission: A Prescription for Curing Healthcare’s Cost Crisis,” and will have copies to share with attendees.
Surescripts

Booth 6158
Contact: Leah Bruch, director of consumer marketing
customer@surescripts.com
703.921.2121
Surescripts serves the nation with the single most trusted and capable health information network, built to increase patient safety, lower costs, and ensure quality care. Through the Surescripts Network Alliance, we convene health IT stakeholders to tackle critical issues all year long. HIMSS19 is an excellent opportunity to continue that work. If you’ll be in Orlando, visit us in booth 6158 to learn how we’re partnering across the Network Alliance to address some of healthcare’s biggest challenges, with a special focus this year on prescription price transparency. Or, just stop by for a coffee break and say hello.
Highlights Include:
- The Interoperability Showcase: "Clinical Exchange and Price Transparency," Tuesday, February 12-14.
- Panel: "Enabling Price Transparency with Actionable Intelligence at the Point of Care," Tuesday, February 12 at 12:30pm.
- Booth Panel: "Advancing Healthcare with the Surescripts Network Alliance,” Tuesday, February 12 at 4pm.
SymphonyRM

To arrange a meeting, contact Sheetal Shah.
Contact: Sheetal Shah, VP of client development
sshah@symphonyrm.com
310.916.7379
Visage Imaging

Booth 1391
Contact: Sean Lambright, global head of sales
slambright@visageimaging.com
480.200.9385
Visage Imaging is a proven global provider of enterprise imaging solutions scaled to support PACS replacement and more, at the world’s most prestigious and sophisticated imaging organizations. The Visage 7 Enterprise Imaging Platform delivers amazingly fast server-side rendered images, streamed via an intelligent thin-client viewer. Radiologists and referring physicians have a customized, protocol-driven workflow to natively view multi-dimensional imagery using One Viewer.
Visage delivers best-in-class modular interoperability, enabling institutions to optimize their informatics investments. To that end, Visage offers Visage 7 Open Archive, a native, modular component of the Visage 7 Enterprise Imaging Platform, including enterprise-class speed, capability, and scale with no additional software required. Visage 7 also supports the viewing of non-DICOM and medical multimedia objects, provides diagnostic mobile access with Visage Ease Pro, and most recently at RSNA 2018 announced Visage 7 AI (works-in-progress) unifying research and diagnostic imaging in the same platform. Come experience why more of the top institutions have chosen Visage than any other vendor, including two of the top-four ranked hospitals in the US. Visage has the proven experience at massive scale to deliver what your institution needs for impactful, lasting, future-proof imaging transformation.
Voalte

Booth 2287
Contact: Melissa Pickle, marketing specialist
mpickle@voalte.com
941.312.2830, Ext. 179
Voalte develops smartphone solutions that simplify caregiver communication. Ranked number-one and named 2017 Category Leader in the Best in KLAS: Software & Services report for the Secure Communications Platform segment, Voalte is the only company to offer a comprehensive mobile communication strategy that enables care teams inside and outside the hospital to access and exchange information securely. Founded in 2008, Voalte is a privately held company based in Sarasota, FL. Visit booth 2287 to power up your care team collaboration!
Vocera Communications

Booth 1747
Contact: Shanna Hearon, manager of PR and communication
shearon@vocera.com
669.999.3368
Meet the new Vocera Smartbadge: For too long, complex clinical workflows and disparate systems have caused unnecessary hassles and fatigued nurses and doctors. Visit booth 1747 and see how the new Vocera Smartbadge makes it easier for clinicians to bring care together with hands-free communication, secure messaging, and intelligent notifications, delivering real-time situational awareness about patient status. https://www.vocera.com/himss
Vyne Medical

Booth 3391
Contact: Molly Maron, director of marketing
molly.maron@vynecorp.com
865.292.0505
Vyne Medical serves a growing base of over 600 active hospital and health system clients nationwide. Best practices are hardwired through technology solutions proven to help hospitals achieve sustainable top performance. Well-published results include improvements in financial performance, physician/staff alignment, patient experience, compliance and patient safety/quality.
YOU MAY HAVE TO TALK LOUDER at the Vyne Medical booth this year as we are giving away mini cell phone speakers that amplify the sound on any phone without having to connect via Bluetooth or cords. And be sure to enter the drawing for a Bose Bluetooth Speaker, perfect for the party you’ll throw after seeing how much time and money we can save your hospital!
Waystar

Booth 6149
Contact: Tina Newman, director of events
events@waystar.com
844.4WAYSTAR (844.492.9782)
Break through to a simpler, more modern revenue cycle with Waystar. Stop by booth 6149 for an immersive visual experience — and a chance to win a Peloton treadmill or an ORU kayak. We’re also hosting a private reception on Wednesday, February 13, at the Hyatt Regency Pool Terrace. Contact your friends at Waystar for an exclusive invitation. We hope to see you soon!
WebPT

To arrange a meeting, contact Shawn McKee.
Contact: Shawn McKee, VP of marketing
shawn.mckee@webpt.com
866.221.1870, Ext. 314
WebPT is the market-leading software platform for physical, occupational, and speech therapy professionals. With WebPT, therapists, executives, and front office staff have access to patient medical records and operational reporting anywhere, anytime, from any Web-enabled device. In addition to documentation, billing, analytics and outcomes reporting, patient engagement, scheduling, and an interactive home exercise program, WebPT provides the highest levels of compliance and security as well as seamless integrations with numerous EHR systems. Ranked the highest performer in the 2018 KLAS Ambulatory Rehab/Therapy Report, WebPT has a 99.9-percent uptime rate and a 99-percent customer retention rate. To see WebPT in action or schedule a consultation with one of our experts, visit webpt.com.
Zen Healthcare IT

Booth 8643
Contact: Marilee Benson, president
Marilee@Consultzen.com
949.528.3600
Don’t miss the opportunity to improve your health information exchange, data quality, and data integration strategy. Your path to simpler interoperability begins with visiting the Zen team at HIMSS. Zen offers a unique Healthcare Integration as a Service (IaaS) platform, as well as interoperability tools and engineering services to help organizations answer these mission-critical questions:
- How can we expand our data exchange abilities and scale for volume?
- How can we add interfaces quickly and efficiently?
- What tools can we use to improve data quality?
- How can we quickly connect to Carequality, EHealth Exchange, or other HIEs?
- What options do we have to improve efficiency in supporting data exchange and data aggregation?
- Who can help us when we don’t have the technology or the expertise to deliver on a mission-critical integration project?
Need answers or better ways to address these common challenges? Meet the Zen team at HIMSS. They will share ideas and discuss technology solutions that will help you fill gaps in your current platforms, and expand your capabilities to meet the ever growing need to connect with the healthcare ecosystem in your community.
Giveaways: Swing by the Zen booth to pick out your own Interoperability Flare Buttons, with several designs to choose from. These are very popular, so come by early!



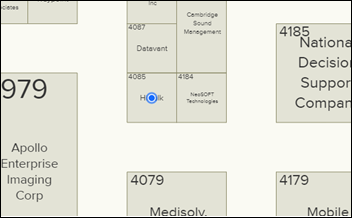
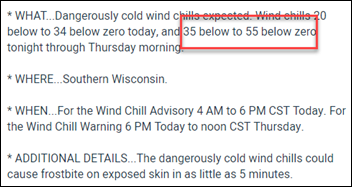



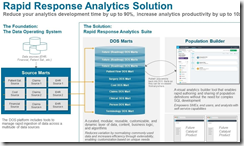




































































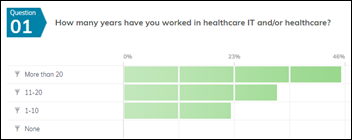
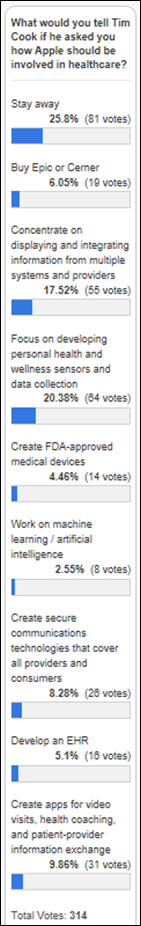
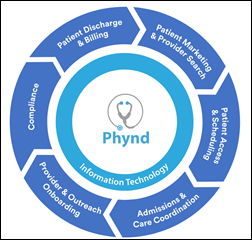
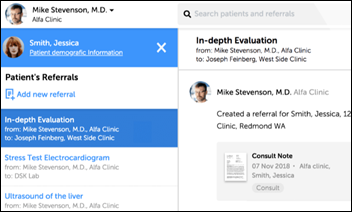
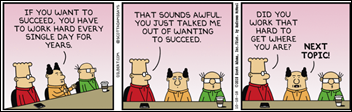



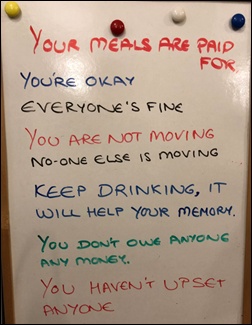
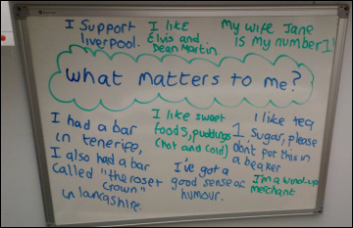





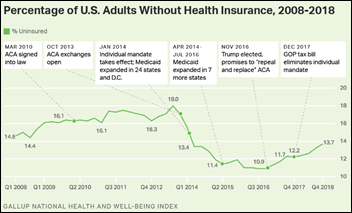

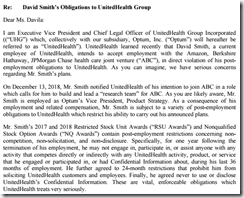

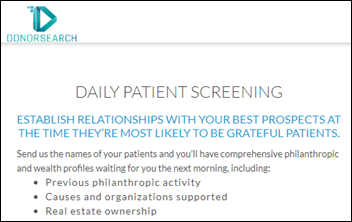





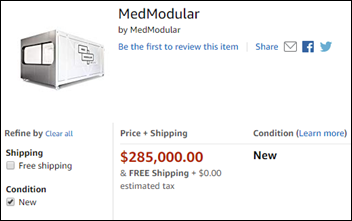




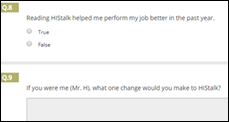




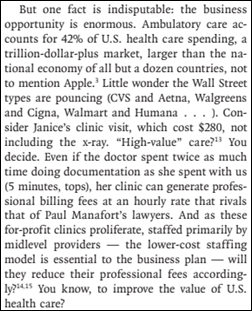

Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…