Gabe Orthous is CIO of Central Georgia Health Network in Macon, GA.

Tell me about yourself and your job.
I’ve been in the business for 20 years. I started my career in revenue cycle, moved on to analytics and population health, and now we’re in the throes of value-based care and providing an understanding around the risk-based models that payers and CMS are presenting. Being accountable and at the forefront of provider engagement.
We support 1,100 providers in our network. Every single modality aligns with Navicent Health, which is our major hospital in this area of Macon. It’s a large footprint of the providers that we support from a PHO perspective.
My background is a technologist. I’ve been an expert apprentice of population health and value-based care. I also teach population health at a couple of colleges as an adjunct professor. I’ve been at this game for about five to six years, seeing the transformation from a quality-based PQRS kind of perspective into, how do we make these things actionable? How do we quantify the effectiveness of these programs to lower total cost of care? Because at the end of the day, that’s what we’re trying to do.
How do you see a clinically integrated network changing the relationship between independent physicians and hospitals?
I’ve worked as a consultant with several types of CINs, many different flavors of those. The relationship between a hospital and the community physicians varies throughout the United States. For us, we’ve always had a strong relationship with our hospital system, being more on a regional level.
It depends on the market. If you come from an educational hospital or a medical center that’s inside of the perimeter here in Atlanta, for example, it’s a little bit different on how they deal with their independent providers. There’s a lot more competition. We’ve been able to build that relationship. It is a bit of relationship building, understanding the priorities of those physicians and enabling them to do the things they need to do to make the hospital successful and vice versa.
Is the trend of hospitals acquiring practices changing the dynamic between independent doctors and hospitals?
I’ve seen in the past 10 years the ebbs and flows of that strategy of going after physician practices and becoming employed versus affiliated. Again, it depends on the health system. You have a “who moved my cheese” ideology of some of the physicians who are now employed, because now they have an 8-5 job or now they have a set of requirements or standards being imposed by their employer, which is in this case the hospital. For them, there’s not that risk of having to pay the light bill at the end of the month. It lowers the risk for those providers to go work for the hospital.
At the same time, the hospital now acquires that risk, and acquires the risk of making sure that the productivity — and in our old fee-for-service world, the RVUs – stay up. But now that dynamic is also changing, because now you have quality measures, specific programs that are requiring these physicians to do certain things in closing care gaps, HEDIS, etc. that now the hospital needs to be able to influence.
It is a hard proposition. These providers are already employed by the hospital, and having some providers do what they need to do to close the care gap, for example, when they may not see an immediate benefit in that performance. But as a whole system, you would.
The idea of affiliation is important to understand. Inside the walls of the hospital, you can enact certain change. You have one view of the world through your EMR, whether it’s Epic or Cerner or any type of hospital-based system. But when you get out into the community, you see more of a diversity of EMRs. It’s harder to enact change when things work differently from a workflow perspective. Epic-everywhere or Cerner-everywhere types of environments are few and far between. At the point of care, it’s important to have an understanding of the topology of that network and become the network of truth as opposed to a single source of truth.
What technologies are important when first moving toward value-based care?
One of the most detrimental phrases in today’s healthcare space is saying, “I don’t know what I don’t know.” Unfortunately, many organizations that I’ve worked with are always saying that. There are different views of the world of how you look at your data, how you look at analytics. One is the clinical focus, the EMR perspective of workflow and patient-centered focused around clinical things that have to occur. Usually those are part of a system of trying to identify CPT codes or ICD codes in order to get paid through a billing RCM model. You have dichotomies of political and revenue cycle. That’s just one component.
On the other side of the house, you have the payer view of the world, which is adjudicated claims that come with a three- to six-month lag of information, telling the providers, “You forgot to do an A1c” or maybe asking the provider to provide a supplemental data set to close the care gap.
The way I look at value-based care today, and to prepare for a technology stack that’s able to be nimble, is to have partners. If you have the money to create your own, that’s great. But have partners that are going to be nimble enough, that are going to be helping you through that data journey and that have flexibility in advocating that data and making it be purposeful.
A lot of times we get into these projects or these technology implementations that are more of a Connectathon. Just send me all the data. Being purposeful, starting with the low-hanging fruit, showing value initially, success factors, identifying the right KPIs, and then building upon that.
So I would say, one, nimble. Two, a technology stack that can aggregate data from disparate sources, including social determinants, care management, and all the other data sources that are out there. Of course claims and of course clinical. Then number three is letting you look at the view of the world through those different lenses. Just clinical, just clinical plus RCM, clinical plus RCM plus post-adjudicated, social determinants, That’s when you start identifying the right populations and how to target things that are going to be part of your performance contracts.
Will being exposed to those technologies encourage practices that are less technically savvy to consider the possibilities of using other technologies to enhance their practices?
Absolutely. You’re bringing up a great point, which is point-of-care analytics and using technology and data to enhance workflows, patient experience, and the things that you just mentioned. But there’s also another component, which is the network view of the world. What are the things that are going to get these physicians the most money for their risk contract? What are the things that they need to do at the network level to have a critical path for patients to follow so that they have better quality and lower cost of care?
Those are two separate things. One is more episodic, while the other is more longitudinal. The technologies and the data required are a little bit different, although they come from the same sources.
At the point of care at the physician level, having additional data sets that are external to “patient presents” is important. I’m going through an HIE implementation right now with a local HIE here in Georgia. I truly understand the physicians wanting to see what happens outside their doors. When the patient presents to the ED, they want to see those discharge notes. That’s an important factor. The problem with interoperability and intraoperability is that those files become convoluted quickly. A CCD as it stands today is a bulky file. It’s hard to read and it’s hard to realize what’s important and what’s not important in there. So we lose a little bit of the usability factor in the technology utilization that we have today.
There are many new technologies that are coming about that are helping the providers focus on what’s important for the patient that presents in front of them from that external actor. But unfortunately, we’re not there yet with all of these EMRs. I’m not talking about one EMR or another. All of them have a lot of work to do around interoperability and parsing the right data set for the right patient at the right time.
What frustrates most people about interoperability isn’t practices not sharing information with each other, it’s that hospitals and practices don’t share information. How do your members see that situation?
It’s a challenge of not knowing what happens outside your doors, whether it’s the walls of a hospital or the doors of the physician’s office. More information is the best around medication adherence, for example. It would be awesome to understand what types of medications are being prescribed outside of that one encounter that you have with your patient.
It’s easier on the commercial side of the house with payers because it’s different types of populations. But when you get into Medicare, ACO, or frailty, for example … frail patients who come in may be prescribed seven medications in seven points of care. It is a struggle and a challenge for providers to understand the full totality and the picture of these patients.
From a workflow perspective, having only 15 minutes to spend with a patient diminishes the amount of value add. A lot of these providers don’t have access to the data. Not just the data, but having enough time to be able to have a conversation with the patient and have that relationship being built.
We still have a lot of problems getting external data into the point of care where it can pinpoint the providers to do the right thing with the data that they’re seeing in front of them that is actionable. It’s kind of a buzzword these days that everything has to be actionable, but it is the truth. These EMRs are becoming more and more convoluted, built on top of version, on top of version, on top of version, and not necessarily making it easier for the provider as opposed to death by a thousand clicks.
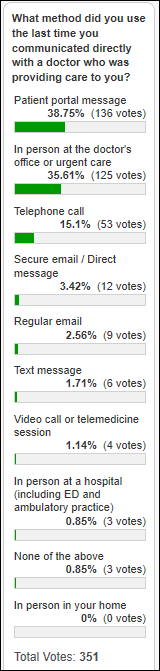
Are practices maximizing the value of that 15-minute visit by collecting more information from the patient beforehand and then following up with them electronically afterward?
There’s definitely an art and a science in that gathering of data pre-visit and post-visit. It really depends on the engagement level of each individual patient. We can have predictive models as to which patients are more likely to fill out a survey pre and post. But in general, I’ve seen minimal impact and engagement from that factor.
I took my daughter to a doctor’s appointment the other and they gave me an iPad to fill out forms, which I loved as a technologist. A generation X-er given an IPad to fill out the information. I even paid my co-pay on the IPad. It was beautiful. They asked me a thousand questions and it was great. It was death by a thousand surveys type of thing as opposed to clicks. Then I’d go in and the HIPAA paperwork was on paper and I had to sign that.
We still have a lot to do from an engagement perspective. I’m sure that there’s a lot of new apps out there that are trying to streamline that process. It’s getting better. Now if you send me an email three days later asking me for an opinion or a survey on my engagement with the provider, I’m not going to fill it out personally. But that’s changing.
Do you have any final thoughts?
No matter what a vendor or a technologist says, value-based care is a hard journey. It will take us numerous years to figure this out. We have an entrenched system of fee-for-service and we’re starting to see models that can help us to ease the transition towards value-based care. For now, we have the two-payment problem of “having food in two canoes.” I’m still in one canoe, and maybe one of my fingers is in the other canoe. Different markets are doing it differently, but value-based payments are here to stay and we’re not questioning that any more.
My suggestion is to think about it more holistically, more of a long-term plan. Have a one-, three-, five-year plan around engagement with your providers, engagement with your patients, technology enablement, ROI on technology implementations, analytics, and data for actionable insights. All these things have to be addressed. Distribution models, so when the payer gives you a downside risk capitation, how do you distribute that money? How do you make it flow to your providers?
There are a lot of things to think about from a strategy perspective. Be patient. It’s not going to change just because you buy a technology. People and process must be outlined before technology comes into a CIN or a network like ours. But having that strategy beforehand is important.
Comments Off on HIStalk Interviews Gabriel Orthous, CIO, Central Georgia Health Network

















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…