Monday Morning Update 2/10/20
Top News
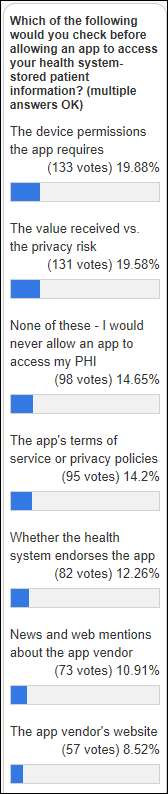
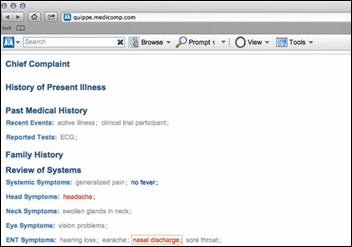
A JAMIA article — whose lead author is the AMA’s burnout expert Christine Sinsky, MD — calls for EHRs to automatically analyze their system logs to report seven standardized efficiency measures.
The authors say such reporting would help experts understand the practice environment. It would also help improve operational, technical, and policy decisions.
The efficiency measures are:
- Total EHR time for each eight hours of scheduled patient time.
- The amount of work performed outside of normal hours, which would require physician schedules to be published to the EHR.
- Time spent writing notes.
- Time spent prescribing and managing refills.
- Inbox time per eight hours of scheduled patient time.
- The percentage of orders that are completed by contributions from non-physician team members (bigger is better, indicating top-of-license optimization).
- Amount of undivided attention patients receive during an encounter, defined as total encounter time minus EHR time.
HIStalk Announcements and Requests
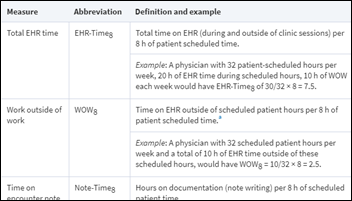
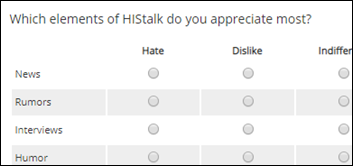
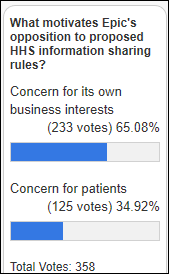
Quite a few poll respondents would never allow an app to access their health information, but others might after considering the permissions the app requires and whether the value received is worth the privacy risk. Not all that many respondents would read the vendor’s terms of services or privacy statement, which is where all the useful information hides. Note: the percentage figures are worthless, but that’s how the poll service lists responses when multiples are allowed.
New poll to your right or here: Do you think employers use the wellness programs and apps they offer to target medically expensive workers for layoffs? I would be super interested in hearing from someone who knows for a fact that it happens.
Welcome to new HIStalk Platinum Sponsor QliqSoft. The Dallas, TX-based company’s secure texting, on-call scheduling, patient communication, and clinical collaboration solutions – which use a unique, cloud pass-through architecture – are used by 1,000 hospitals, home health, and hospice organizations to offer reliable, real-time communication among doctors, other caregivers, and patients. Qliq Secure Texting processes 165 million messages each month, including group and broadcast messages, custom quick messages, active directory contacts, escalated call notifications, presence status settings, and EHR integration for customers such as Virtua Health. HIPAA Camera Roll supports image sharing in real time on personal devices. The company’s Quincy chatbot platform supports proactive patient engagement without requiring an app download, while its Visit Path mobile care delivery tracking allows hospice and home health agencies to comply with 21st Century Cures Act-required electronic visit verification. Thanks to QliqSoft for supporting HIStalk.
Here’s a Qliq for Android overview video I found on YouTube.
Reader Survey
Here’s your one last chance to fill out my reader survey, which benefits me (it’s my once-yearly chance to connect with readers) and might benefit you as well (I’m randomly drawing one or more respondents for a $50 Amazon gift card). Meanwhile, I admit that I’ve peeked at early responses and have already made two changes that readers suggested:
I found a way to allow reader comments to be automatically approved for regular commenters, which will eliminate the delay after a comment is posted until I approve it and thus make it visible to readers.
A survey respondent suggested that I run a “Sponsor Spotlight” occasionally to remind them what a sponsoring company offers. Platinum sponsors can provide a short description (no more than 75 words) and I’ll run the responses in the order received.
I’ll close the reader survey later this week and summarize the results. I appreciate the feedback, the good ideas, and the best wishes. I even appreciate the negative ones since they thicken my thin skin and show that someone at least cares enough to complain instead of just moving on.
Thanks to the following companies that recently supported HIStalk. Click a logo for more information.
Webinars
None scheduled soon. Previous webinars are on our YouTube channel. Contact Lorre to present your own.
Acquisitions, Funding, Business, and Stock
Insiders report that Thoma Bravo is considering selling health IT digital identity vendor Imprivata, which could command a price of more than $2 billion on annual revenue in the $100 million range. The private equity firm paid $544 million for the company in July 2016.
Vocera reports Q4 results: revenue up 2%, adjusted EPS $0.15 vs. $0.18.

Nuance announces Q1 results: revenue flat, adjusted EPS $0.27 vs. $0.27, beating Wall Street expectations for both. The company said in its earnings call that early adopters of of its ambient clinical intelligence “exam room of the future” are reporting improvements in physician satisfaction, patient throughput, and documentation time, with its formal launch planned for Q2. Nuance says its HIMSS demonstrations will show a more interactive solution. The product is customized for each medical specialty and will start with five high-revenue and complex specialties, after which rollout will continue to additional specialties at the rate of 1-2 per month. Nuance is considering licensing the product based on exam volumes, bundling in hardware to minimize upfront cost.
Sales
- Minnesota mental health clinic provider Nystrom & Associates chooses Relatient for patient outreach and communications.
People

Children’s Minnesota promotes acting VP/CIO Dave Lundal, MBA to the full-time position.
Announcements and Implementations

The local TV station profiles the rollout by UCHealth (CO) of BioIntelliSense BioSticker, a chest patch that monitors vital signs (respiratory rate, heart rate, skin temperature, gait, and body position) and stores the information for 30 days. UCHealth’s CARE Innovation Center help develop and test the FDA-approved device, which will receive its first patient use later this year.
Government and Politics

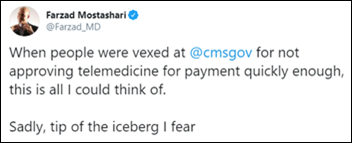
Interesting: several Missouri health systems don’t allow their doctors to certify patients for medical marijuana use – even though such use is legal in that state – because they receive federal funding and federal laws still classify marijuana as an illegal drug that has no medical benefits, potentially threatening their income or licensure. SSM Health’s chief medical officer says, “There’s not a great evidence base to support using this for the majority of complaints that come through. But again, I think the important thing for our providers was to trust them to do the right things. If patients are going to use cannabis, they should be using it under the supervision of a doctor they know and trust. We don’t want our patients to run off to the local doc-in-a-box to get certified for medical marijuana without us participating in that care.” Note the telemedicine aspect in the company webpage above.
Other
KHN reviews the “moral injury” that is experienced by ED doctors whose employers push them to order unnecessary but profitable tests; to see patients quickly but superficially to improve “door to doc” time and generating higher facility fees; and to treat patients in hallways because of ER overcrowding and hospital discharge inefficiency.
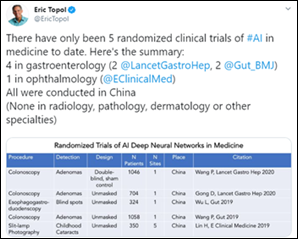
Eric Topol’s medical literature review finds that only five randomized clinical trials have looked at the use of AI in medicine (all of the studies were performed in China) and just 11 prospective trials have been completed in a real clinical environment. All of the studies addressed diagnosis rather than treatment.
Sponsor Updates
- Meditech publishes a new Success Story, “CalvertHealth Makes Major Gains in Battling the Opioid Epidemic.”
- Mobile Heartbeat will exhibit at the ACNL Annual Program 2020 February 10 in Rancho Mirage, CA.
- Clinical Computer Systems, developer of the Obix Perinatal Data System, opens an office in Dubai.
- PatientPing features Cerner VP of Population Health John Glaser, MD in its interoperability video series.
- Redox releases a new podcast, “The New Interop Paradigm with America’s First CTO, Aneesh Chopra.”
- Relatient announces its patient relationship management software now integrates with Virence Health’s Centricity Practice Solution.
- T-System relocates its headquarters to 6509 Windcrest Drive, Suite 165, Plano, TX 75024.
- Wolters Kluwer provides easier access to latest coronavirus resources and tools for front-line clinicians and medical researchers.
Blog Posts
- On-call scheduling: 4 ways to boost patient care and satisfaction (Spok)
- Leveraging Technology to Improve Patient Satisfaction (Lightbeam Health Solutions)
- Maintain Situational Awareness of Continuity of Operations During a Hospital Cyber Attack (LiveProcess)
- The American Healthcare System’s 800-pound Gorilla Has Spoken (Loyale Healthcare)
- How Annual Wellness Visits improve patient outcomes and organizational revenue (Meditech)
- AI in Healthcare: Finding the Right Answers Faster (Health Catalyst)
- Marketing Your Physical Therapy Practice to Physicians (MWTherapy)
- Why Your EMPI Needs Address Verification Technology (NextGate)
- Developing a strong lab outreach program (OpenText)
- How consumer data can help attract and retain healthcare consumers (Experian Health)
- What Healthcare Providers Need to Know About New Price Transparency Requirements (PatientBond)
- Digital-First Billing Makes a Difference for Roper St. Francis (Patientco)
- Why Your Governance is Only as Good as Your Identity Data (SailPoint Technologies)
- Six Critical Aspects to Deliver Strong ROI from Any Test Automation Program (Santa Rosa Consulting)
- Addressing Coronavirus and emerging health concerns with engaging content (StayWell)
- How a Rural Health System is Transforming Lives in the Face of Addiction (Surescripts)
- There’s Voice Communication. And Then There’s Voice Communication for Healthcare. (Vocera)
- AI can save you from drowning in prior authorization problems (Waystar)
- The 3 Stages of Building Referral Relationships that Last (WebPT)
- Bend the cost curve in your senior population (Philips)
Contacts
Mr. H, Lorre, Jenn, Dr. Jayne.
Get HIStalk updates.
Send news or rumors.
Contact us.


























































I use a wiki and was exploring some of the extended character sets. I was startled to learn that the…