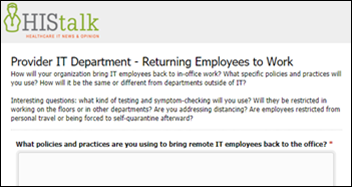
Survey Results: Provider IT Department Plans for Returning Employees to Campus
Working from home and remote meetings are both still considered the norm. Only have 50% of normal occupancy of the office, and have a sign-up SharePoint so that we stay until that limit. We keep track of everyone present and which rooms they’ve used in case there’s an infection later and we need to keep track. Avoid using anyone else’s wings /floors /meeting rooms. Hand sanitizers at almost every single intersection. Everyone is required to wipe down the meeting room and/or desk before use with sanitizer, which is provided. Point person who is in charge of maintaining rules in each area. No use of refrigerators, and dishwashers have to be run at highest temperature. No external visitors unless already approved.
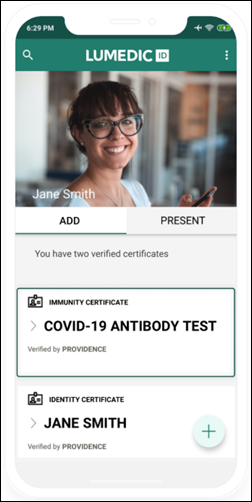
For the near term, we are not. We have virtualized all our contact center agents, finance, HR, marketing, IT, legal etc. As we get into a groove, we are finding that maybe not everyone returns. Also, being in the epicenter of NY/NJ, we still are very cautious. When we return (after Labor Day), it will be on a rotating basis, 2-3 days a week, to be able to do social distancing, deep cleaning, masks, Plexiglas in cubicles, not sharing of equipment, etc. Right now our focus is on returning the hospitals and physician practices to operations. And we are starting antibody testing of every single teammate, which will be completed by mid to late June – that’s 36,000 people.
We have four different office spaces. We are reviewing the spaces and will schedule staff onsite alternating 2-3 days per week ensuring social distancing. Will rotate staff weekly two days in office and three three home and than the reverse.
Bringing back while requiring masks to be worn. No travel.
My IT organization announced today that all employees will continue remote work practice until 1/1/21 at the earliest. This includes all install and go-live support and all corporate travel has been suspended until that date. The remote employees were approximately 40% of the workforce prior to the lockdown. The “bring back in” is not an issue for use today. Ask again in seven months.
Temp check when entering designated employee entrances. Must wear mask into the building. Mask must be worn when outside of office. Can remove mask if in office alone.
The IT department employees returning on-site follow the exact same protocols that all hospital and clinic employee departments follow. There is no differentiation. All employees must enter through the same designated employee entrances where temperature is checked via an infrared thermometer. Any employees (and visitors) with a temp of 100 degrees Fahrenheit or higher OR exhibit visible signs of illness symptoms are not allowed to enter the building. Employees who are turned away must contact the their supervisor and the employee health department to make arrangements for continued remote work and for X number of days away from the hospital before being allowed to attempt to enter on-site again. X changes are set according CDC guidelines. Cloth face mask worn at all times in the hospital. The only exception is at your desk or in other areas where there are not other people or the possibility that other people would enter the area. CDC social distancing guidelines are to be observed as well.
There is nothing formal. Departments are taking it on a person-by-person basis. A big challenge is reconfiguring work areas so that workers are more than six feet away from each other. Since many have been successfully working remotely, there will be a clash of opinions about having employees return at all (We need you back in the office. Why? We’ve been successful not being in the office.)
Bringing back 50% of staff on alternating days. Created A/B groups based on the office cubicle configuration so that no more than two employees per pod would be in on a given day. Keeping an alternating three-day / two-day bi-weekly work from home schedule. Marked off six-foot separations on the floors to indicate proper social distancing from cubicles and in conference rooms. Removed extra chairs from conference rooms and kitchen to allow only the number of individuals to conform with social distancing. Providing masks, hand sanitizer, and disinfectant wipes to staff for work space use.
Not allowed in the break room without mask and gloves on. Limit the number of people allowed in the break room at a time. Moved people around so that desks and offices create safe distances. Not everyone is allowed in the office at one time, so staggered schedule between WFH days and in office days. If you go to a hospital for more than a few hours, you WFH for 14 days.
We will continue remote work for the foreseeable future. We’ve been doing just fine being 100% remote for the past two months, so there is no rush to bring folks back into the office.
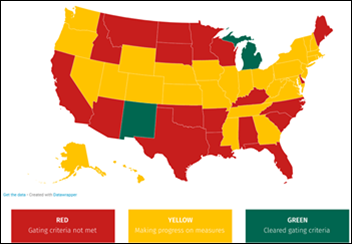
Presently evaluating how many workers we will ask to return to offices, considering office reconfiguration requirements to ensure proper social distancing. Many workers are rightly concerned with potential COVID spread. We are working to demonstrate the productivity impact of working from home, which we believe to be positive. With a large number of elderly workers, we must be concerned wit their vulnerability. As communities reopen, we have to watch for increased COVID incidence.
Schedule time for people to come to the office and remove all of their personal items and non-work items from their work surfaces to allow consistent cleaning. Extra furniture being removed. Face coverings required in common areas and screening required upon entering building. Still requiring manager approval to return to the office. We will have to have staggered start times to avoid congregation at the screening stations and staggered work days to ensure proper social distancing. That dense cube farm that seemed great is now a major liability. No personal reusable water bottles, coffee cups, etc. are allowed unless filled at home but cannot be refilled at work. Bottom line, still encouraging IT staff to stay at home unless absolutely necessary to be on campus.
Our team was almost entirely remote (almost entirely out-of-state, in fact) so we’ll see no change. Our sibling teams were more local-focused, but I expect they will drop to two or three onsite days per week, in shifts (likely in perpetuity, in my opinion).
For the most part, continuing to encourage them to work from home and limit days in the office. When in the office, they will be under the same masking policies as all staff. No in-person meetings unless social distancing can be enforced. No allowing vendors on campus unless they are required as part of installation, implementation, or service. No sales calls.
We are not actually trying to bring everyone back into the office. And we will wait until some time after the recommendations take place to do so. We are planning a very gradual increase to onsite work, starting with only coming in if needed to perform a function not able to be done appropriately remotely (where interacting with other individuals and/or equipment requires it). We’ve found that our team has been quite productive in the current mode and I see no reason to rush them back in.
We are considering 100% work from home and giving up our office space. Our employee productivity remains high, our employees are happier, and we believe it will be an advantage in recruiting new employees. We already have departments 100% remote, and more departments are considering going 100% remote.
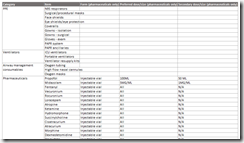
At our organization in Colorado, we’ve been using the CareCognitics workforce assessment tool for all of our employees. This includes evaluating each employee every day for risk for COVID-19 and escalating those at risk to testing when needed. The tool also assesses the mental health state of each employee. It has escalation to HR or other supervisors as needed. The analytics back end also tells us who hasn’t done their daily assessment so we can address that with the employee. Along with daily assessments, we also have created back to work assessments for those that have been off so we can assess them before they return.
We aren’t. Honestly, we’re evaluating whether we will for a large majority or just move to mostly permanent work from home.



















































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…