Jeremy Schwach is CEO of Bluetree Network of Madison, WI.

Tell me about yourself and the company.
Bluetree is about 400 people strong. We help the largest healthcare organizations in the country tackle their biggest problems. About half of our folks come from an IT background, specifically Epic, and the other half comes from a provider background and really understands the business of healthcare. We put those two things together, we figure out what our clients need, and then we jump on it.
How will current events affect the consulting business, both now and in the future?
A lot of our work is core IT related. In some instances, we are as busy or even busier in certain areas. In other instances, we are helping with the big strategy projects that our clients have pushed.
For the most part, we haven’t seen anything totally cancelled. There’s a lot of instances where our clients are saying, and rightfully so, “We need to stay focused on the crisis at hand.” They are dealing with what the rest of the world is dealing with from an economic standpoint, trying to figure out how to prioritize.
Certainly the bottom isn’t falling out. We are taking a long-term view. We’ve seen new opportunities around telehealth. Organizations have moved incredibly quickly for their size compared to how long it has taken historically to get big enterprise projects done. We feel good about the long term and we know that we need to make sure that we are weathering the storm like the rest of the world.
Epic, Cerner, and Meditech have turned around a lot of COVID-19 related changes quickly, ranging from terminology updates to mobile hospital support to telehealth integration. Are customers taking advantage of these new options?
I would say yes. It’s amazing how focused the mission becomes when you are dealing with something that is as acute, and in some cases as devastating, as the current crisis. It ranges from vendors who are putting their best foot forward to clients who have accelerated two-year projects to get them done in two weeks.
I’m impressed with our own folks, who have gotten creative in tough situations. We were remote-first to begin with, so we had a little bit of an advantage. But no one was prepared to take on full childcare and also support their clients who were, in some cases, as busy as ever fighting on the front line. A lot of people in healthcare deserve a ton of credit as their mission comes into focus in times like these.
Are your clients worried about cash flow after being forced to temporarily shut down their most profitable services?
Everybody is concerned, in part because it’s hard to plan. How long does this thing go? When do we start letting patients come back in? “Elective” is the wrong word considering that no one wants to get surgery. At some point, you have to let patients back in.
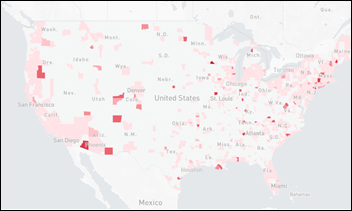
That is made more difficult by the regional nature. We work with a 160 clients across the country, most of them large. You can take an inner city hospital that is battling this thing on the front lines. Then you go two hours in any direction and you can find a hospital that has had few or no COVID patients. They’re still planning for it, so they have the the same economic hardship from reduced census and lack of profitable electives. While the regional nature is bizarre, everybody is in the same economic quandary.
What technologies have been recently embraced that will stick after things get back to some kind of normal?
We are seeing the same things that you listed in your post. A lot of digital tools. Chatbots getting deployed more widely.
What is interesting is the amount of infrastructure that is required to stand up something like telehealth. Most people look at telehealth as the tool itself and the availability of physicians. There’s an underbelly infrastructure that is a big part of the heavy lift. For example, we take patient calls for some of our clients and have expanded that service because our clients need it. But regardless of the telehealth tool, a whole demographic of patients are just not going to be comfortable using it. It’s basic things, like opening the right browser and getting webcams set up. We’ve seen this huge spike in patient calls as a result of some of these new tools, and it’s not even COVID related, necessarily. You have to build an infrastructure around these things.
We expected our clients to kick the can on some of our big strategic projects to keep everybody focused. We haven’t seen that happen. In some ways, our clients are even more focused on this consumerization of healthcare. We do a lot of work on patient access centers. Because we are accelerating these new tools, clients are having to create the customer service infrastructure that other industries have built up over 10 years, but that is new to healthcare. We are seeing a lot of demand, and these hard, big projects that impact tens of thousands of users continue to move forward.
If you want to put in cool new texting apps or the latest fancy bell and whistles from your new startup, you need that baseline infrastructure. A patient has to be able to call in, talk to somebody about financial counseling, get a nurse in real time, get their prescriptions refilled, or get an appointment scheduled. Now you are adding telehealth volume and chatbot questions to that mix. Our clients are accelerating building that core infrastructure, because otherwise it’s hard to do anything in the consumerization patient world. It was surprising how quickly something so strategic kicked into high gear.
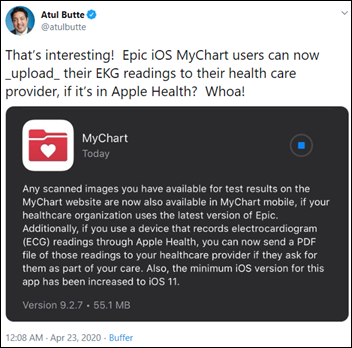
What interesting changes are you seeing from Epic and other vendors?
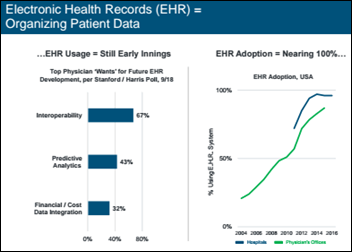
A lot of what clients are leveraging now existed in the past. We have just re-prioritized in healthcare. Vendors haven’t released a lot that is brand new or that was spun up quickly, but certainly they have been incredibly available on the analytics front. Maybe one of the surprising outcomes was Epic and other vendors working with the federal government to figure out, because of their large footprint, how to help from an overarching view of what’s happening in the country. Vendors weren’t necessarily doing or even feeling comfortable doing that historically. The current times demanded that, so they stepped up to the plate.
MyChart tools, chatbots, and telehealth all existed. It was a matter of prioritizing and then building the infrastructure.
What types of companies will be best positioned to weather the crisis and emerge strong on the other side?
We were acquired by Providence in July, which gave us a longer-term view. Our approach has been that current events are changing healthcare dramatically, and in some cases for the better. When we come out of this, the changes that we are already feeling will be accelerated. The opportunities in healthcare continue to grow and are maybe even being expedited by the current crisis. Anybody who takes a long-term view is going to be better positioned. We are doing everything we can to keep the team together, but our goal is to make sure that when times that are slower, we take advantage of the opportunity to build and focus on what our clients need now.
Your readers will roll their eyes when I say this because every CEO has to say this, but I personally feel incredibly fortunate to be attached to Providence. We are a small company that has an opportunity to make a big impact, because even as a small company, we work with some of the largest, most influential healthcare systems in the world, and on some of their most strategic projects. We feel fortunate to be in that position.
As a small company, you’re wondering about your long-term view and whether you can go about it as a solo practitioner. It is doable, but incredibly hard and increasingly rare.
You wonder if you should take the financial buyer route, such as private equity. You know the pros and cons of that. One of the cons is that your company will be sold every three to five years by an owner that really cares about just one thing, which is their prerogative and goal.
Then you have the strategic, who will look at how to leverage the skill set, the people, or the customer base.
Providence came to us in February and basically said, there’s a fourth option. We have this 170-year-old, mission-driven non-profit with an enormous footprint. We are one of the largest Epic clients on the planet. We want to keep delivering this vision for another 170 years. We know healthcare is changing, so we want to do things differently.
That was the Providence sales pitch to us. We could help them modernize and innovate, but we could also gain an opportunity to do things differently, remain independent, and work within a new commercial entity that can go out and do bigger things. We get the platform to do what we already do, but with a bigger impact.
We are nine months through it and it has been incredible. They have been an amazing partner because they aren’t a PE shop or a traditional strategic. They are totally different and they have been true to their word. We are fortunate to have them as a partner.
The initial announcement said that Providence planned to build a $1 billion business from their acquisition of Bluetree, Engage, and other companies. How is that working and what is the strategic direction?
The vision has been super clear from the beginning. It’s not easy to do. They’re a large organization. Those wheels have been turning for a very long time.
Before the acquisition was finalized, I had a chance to sit down with Mike Butler and Rod Hochman, the president and CEO. They said, tell me one other organization that is 170 years old, founded by a group of women, with our scale, that cares deeply about a non-profit mission, and that has survived for all these years because of that vision. Rod laughed and said, don’t think too hard about it because there isn’t any other.
They are in a unique position because of longevity, their 114,000 caregivers, and the skill to do it differently. Because of that vision, it’s been clear what we need to build. One of their guiding principles was that this would not be Bluetree and Engage folding into Providence. They could build that themselves. This is taking advantage of their scale and all of the smart people they have to build something different.
What’s been most surprising to us is that a consulting company, we’ve got folks across so many clients. We’ve got a pretty good long view of what’s happening. We felt like we could make a difference for Providence, and that’s important.
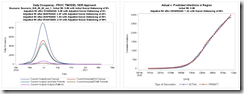
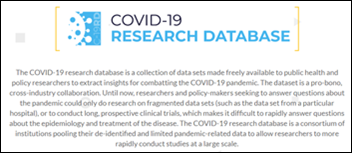
The crisis has shown us, in a short period of time, that Providence has as much to give us as we have to give them. Their response to the crisis has been unbelievable, that an organization with that level of scale could move that quickly. They had the first confirmed COVID-19 case in the US, so they had a head start. Not only did they stay focused and organized, they allowed us to come in and learn from them as they were going through this. Because they have this amazing non-profit vision, we posted their learnings publicly. Our website has a COVID-19 page and a lot of the content was from Providence’s learnings.
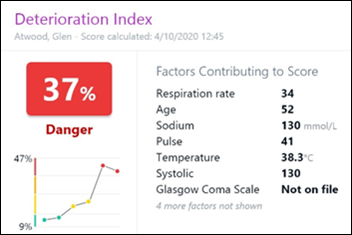
We did a deep dive as they were building their analytics tools across their large geographic regions and we learned a lot from them as they looked at cash, preserving cash, and accelerating cash as we come out of this. We got an inside view, the chance to exchange ideas, and then the opportunity to publish it quickly because it was good for the world. That drove home the fact that this is such an unusual partnership in healthcare.



























Why does the displayed "exam room of the future" still have the classic "clinician has their back to the patient"…