HIStalk Interviews Lissy Hu, MD, CEO, CarePort Health
Lissy Hu, MD, MBA is co-founder and CEO of CarePort Health, powered by WellSky, of Boston, MA.

Tell me about yourself and the company.
I’m a physician by background. CarePort connects hospitals with post-discharge providers, such as nursing homes, home health agencies, hospice, community-based providers, and all of the services that patients need after a hospital stay.
What activity are you seeing around hospitals sending ADT notifications to the patient’s other providers now that the deadline is getting close?
We’ve spent the last couple of years helping hospitals and post-acute care providers navigate that initial transition from the hospital into post-acute. Instead of a fact-based or manual process, where the discharge planner at the hospital picks up the phone and calls around to all the different nursing homes in the area asking if they have a bed, we have a network of hospitals and post-acute providers on our platform that can send these referrals electronically and that can communicate back and forth.
Over the last two years, we’ve seen more interest in closing that loop or that round trip. For the ADT piece that you referred to, not just how to get patients out of the hospital efficiently and share information back and forth in that transition, but being able to understand, when a patient lands in a skilled nursing facility, how long they are there, especially if a patient then goes back into the ED or gets admitted. We are seeing a new level of collaboration between acute and post-acute, especially as folks are starting to realize the importance of post-acute and how much that drives outcomes, both from a cost and quality standpoint.
We’ve learned that open hospital beds aren’t managed like a grid, where COVID-19 patients are moved between hospitals based on individual hospital capacity and clinical capability. Are hospitals showing an interest in sharing open bed information with each other?
On the bed availability piece, you are right. There’s not a centralized information piece out there, and we are seeing more interest in wanting that level of visibility. We are seeing it not only on the hospital side, I would say, but interestingly, on the post-acute side as well.
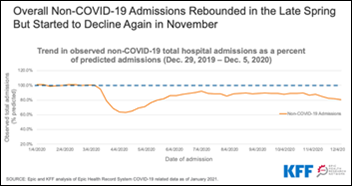
One of the things that has been so interesting about COVID-19 and the pandemic is that we sit in the middle, in terms of the hospital and the post-acute. We see the impact on both sides. Even in April and March of last year when things were really kicking off in the New York area, what we were seeing was that the hospital capacity and their capacity to take patients is very much tied to their ability to discharge patients into that next level of care, in terms of that post-acute.
People will start to see that it’s not just about the hospital bed — it’s around capacity and that flow across the entire continuum. New York hospitals were having a hard time getting their patients out of the hospital and into post-acutes, because a lot of these post-acute providers changed their admissions policy with COVID-19 in their vulnerable population. That hesitation to take on new patients backed things up from the hospital. What I’ve been encouraging our customers to think about is that visibility into the hospital beds is helpful and it’s necessary, but you also need to think about that next step. Where does that patient go? Because it is a pipe that’s connected.
We also saw in New York a high number of nursing home deaths that were possibly caused by forcing them to accept their residents back into the facility following discharge from a COVID-19 hospital stay. How will that situation change permanently and will technology play a part?
That highlights two things. First, the interdependency between hospitals and post-acute providers. It also highlighted to a lot of people the dual roles that nursing homes play in our society.
On the one hand, they are residential facilities for the elderly, the vulnerable, and those who can’t be in their own homes, so they are these long-term care settings. On the other hand, we rely on them as post-acute settings, where folks who have gotten a hip or knee replacement or are recovering from surgery go for a couple of weeks, almost like a step-down unit, to recover, to rehab before moving on to home with home health or back into the community. That was the challenge of New York and really all across the country — we need places for people to recover that aren’t the hospital.
At the same time, these facilities traditionally have been these residential facilities for the elderly and the vulnerable. How do we balance that? Does that get split apart? The role that technology can play is facilitating that transition as much as you can with high-quality information. In our products, we looked at facilities that could take COVID-19 patients, that had a separate wing, isolation wings, and a separate admissions processes. We tag those in our system so that the discharge planner at the hospital will know. We transmitted COVID-19 results that were pending from the hospital to the post-acute care provider.
Those were all COVID-specific changes that we did in part because we had to help our customers, but also because the market is moving to increased interoperability between the hospital and the post-acute care providers. There is a need to share more and more information, especially as we are seeing sicker and sicker patients going into post-acute because of length-of-stay pressures in the hospital.
Your product helps hospitals and families select a skilled nursing facility, with CMS star ratings being one factor. Were those ratings predictive of which SNFs had a lot of COVID-19 deaths, and will consumers look at different criteria after the pandemic is controlled?
The biggest change we’ve seen is a shift away from facility-based care towards more home-based care. There have always been patients who clearly need to go to a facility, or who clearly can go home. But in the middle ground of patients are those jump ball patients that could go home, but maybe they are just sick enough or frail enough that they need to go to a facility. We’ve seen a lot of this shift, where patients who might have gone to a facility in the past are now going home.
The other change is that going home instead of to a facility is a more difficult discharge. When you go to a facility, you’ve got your dialysis, you’ve got your infusion, you’ve got your nursing care. All of that is set up for you. When you go home, the discharge planner has to set up all of those pieces a la carte.
We saw hospital admissions go down, so we were expecting referral volume to go down. We found that when we looked at 2020, our referral volume went up by almost 20%, even though total admissions to hospitals were down. I think a lot of that can be explained because of the complexity of setting patients up at home and the need to set up more and more services. A lot of people are saying that COVID probably accelerated some of that, but that trend of more patients opting to go home was already there.
That was a roundabout answer to your question about whether patients are picking facilities differently. The shift to home was probably the number one trend that we saw. But in terms of patients picking facilities differently, I think people are paying more and more attention to the quality of nursing homes. COVID highlighted some of the problems with those ratings that a lot of folks in the industry have already raised. I hope this will push CMS for more transparency, more data on the quality of these nursing homes. Right now, for example, they are considering adding COVID-19 vaccination rates of staff and patients to that rating. That is an excellent idea, given what we know about the vulnerability of that patient population.
Overall, it has pushed patients and their families to consider that choice with wanting more information and better information. Hopefully that pressure from patients and their families will give us even more transparency than what we have today.
WellSky said when it acquired CarePort that it would invest significantly to expand CarePort’s capabilities. What changes do you expect to see?
Luckily when we went through this process of parting from Allscripts and choosing our next home, we had a choice, which is important. When we spoke with WellSky and we talked about our shared vision, I wanted to be very specific around what that meant, rather than amorphous corporate jargon about synergies. I was impressed with WellSky because they had been thoughtful about the process. Given the price that they paid, it makes sense that they were thoughtful, speaking in the realities of the world.
Specifically, in terms of the benefits to our customers, there were probably three things that we looked at and valued. The first is, as we are seeing more of a shift towards home-based care, our clients are asking us to connect more and more with these home-based providers. WellSky is in one in four home health agencies in the US. Being able to add those agencies to our network, both as referral partners and to add visibility in terms of that ADT and deeper clinical data, was valuable out of the gate for our customers.
The second piece was that WellSky has a network that goes beyond home health and delivering medical services into the home. They have a huge network in the social determinants of health space. Again, as we are seeing more of a shift home, there are more concerns around how the patient is going to get their meal. How do we think about the non-medical parts of their care that we can support in their home? That was another piece that the WellSky network added for our customers.
The third piece was funding. The deal closed on December 31, 2020. We started the year with 200 people and we are already in the process of trying to hire 50 more people to our team.
You’ve said that you want CarePort to be a place where smart women want to work. How do you make that happen?
It all starts with the culture that you build. When I was in business school and in medical school — and I’m almost embarrassed to admit, even when I was taking classes on corporate culture and team dynamics — those soft classes almost felt less important in some ways than the finance and accounting classes. The hard business classes, if you will. I have to say that my biggest learning in these last eight or nine years since I founded CarePort is that it’s the opposite. Team building, figuring out how to manage, figuring out how to set up a positive culture where women are valued, where you enable everyone to speak up — that’s the hardest part about building a company.
At our scale, the lesson that I’ve learned is that it’s not even just about you and maybe the senior people in the team. You have to be hiring people at the manager level, at the director level, all down through the org, to make sure that those managers embody the competencies that they need to meet the roles and responsibility of that job, but the right culture and the right attitudes as well. That’s how you build a culture at scale. It’s not just from the leader, the CEO, the founder, the visionary. You have to staff in your company at all levels with people who want a positive working environment for women, who value the contributions of women, and who understand some of the complexities and challenges that women face. When you’re building a company and trying to recruit, all those things are difficult to prioritize. But really, that’s how you bake this into your DNA. You have to find people at all levels who embody that.
How did you protect that goal while being acquired twice?
You have to be thoughtful about why you’re doing the acquisition. To be fair, some companies just don’t have that choice. For us, luckily, we’ve always had optionality, because we’ve been doing well and we’ve had supportive backers, first from venture capital, then Allscripts. For me, when I evaluated an acquisition and whether we should do it versus do nothing and continue on our current path — because that was always an option that was available to us — there are two lenses that I always thought about. One is, do I see a tangible benefit to the customer? If the answer is no or it’s amorphous, then immediately we shut the conversation down. Because ultimately, if it’s not good for the customer, it’s not good for the business, end, period, stop.
But the second lens, once you get through that hurdle, is, is it good for the team? What is the feel of the culture of the other organization? What is their leadership like? What is that working environment? Is it a place where I could see my team thriving? Because as a founder, some of these people have been with me since the very, very beginning. They left higher-paying jobs with more security, they had families, and they came to a startup where there was none of those guarantees. I feel a tremendous responsibility to my team to make sure that they are taken care of and that my customers are taken care of. Not every company has this choice, but because I’m still here, because we’ve been doing well, because we have this choice, I wanted to optimize around both of those fronts and I was able to.
Do you have any final thoughts?
I’m excited about the future of acute and post-acute care. We have seen even more so than when we last talked, given the changes caused by COVID-19, the interdependency between acute and post-acute. In the next couple of years, I’m seeing payers become more involved in that relationship as well, as payers are trying to think about post-acute and think about how to work with post-acute. Those are some of the things that I’m excited about. Also, having patients who are more engaged, who have more data available to them. Those things will be important for patients who need post acute-care, a number that will only increase.













































































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…