Ann Barnes is CEO of Intelligent Medical Objects of Rosemont, IL.

Tell me about yourself the company.
This is my 13th year of running healthcare companies, both on the services and now on the software side. IMO is a fun company that was founded in 1994. The founder’s vision was that software companies and technology companies that wanted to make a difference in healthcare had to think like doctors and clinicians. Everything we do at IMO, both with terminology and data insights, stems from giving clinicians and doctors what they need to be able to get off the computer, stop focusing on that, and instead focus on patients. Then, how we can help provide better data and better insights to improve patient outcomes.
What are the terminology challenges with interoperability and aggregating data from multiple hospitals?
Terminology is not static. It is constantly changing. You need clinicians to keep terminology current, which is hard for hospitals that try to do it on their own. We specialize in not only keeping the terminology current, but adding new terminology as it becomes necessary for the medical field. COVID was a strong example. We started in January working side by side with the CDC in adding new descriptors and terms so that physicians could describe the symptoms of COVID differently than they were describing the symptoms of the flu. Otherwise, it would all look the same.
Does demand exist, beyond public health, for immediately retrievable patient information that originates in hundreds or thousands of hospitals?
Yes. Probably one of the biggest challenges across healthcare right now is that as data is aggregated, details are lost because it is not standardized or it’s coded. Somebody wants to get back to that level of specificity about a patient or about a group of patients that they are monitoring or trying to find, but that is difficult once you get back at the granular level.
We are fortunate at IMO that one of the initial values of our product is that we let physicians speak physician and write something just like in Google, any way they want, and we make sure they have the freedom to document how they want. We translate that to 24 global code sets, but more importantly, we maintain the specificity of the data so that it can be unlocked on the other side. We are spending a lot more time thinking about insight products and how to normalize the data that’s coming out of disparate systems and then pull insights from that data in an easy way that is maintained and updated.
At least we didn’t force physicians to do their own manual terminology lookup and translation for someone else’s benefit, as was done with other scribing chores.
Exactly. Clinicians don’t want to have to think about what the data is going to be used for downstream. They are focused at that time on the patient and describing as specifically as possible what is going on with the patient and any sort of diagnosis. Whether that data is being used for reporting, billing, or quality reporting doesn’t matter to the physician. They are trying to capture the data and take care of the patient who is in front of them.
As value-based care increases and the focus on patient outcomes increases, that intensifies. We are trying to take off the plate of that physician the worry about what’s going to be done downstream with this data. Let’s capture the specificity as you want to share it.
Has the challenge become easier with consolidation in the number of EHRs being used?
We actually we see the number of EHRs increasing in health systems. They will have Epic, Meditech, or Cerner, but then they also have an ambulatory EHR, behavioral health EHR, or other EHRs in their clinics. The are sitting there in their health system trying to pull data.
COVID was again an example. Health systems were struggling to find the COVID-symptomatic patients or the COVID-positive patients with underlying conditions across the health system. That is one of the reasons we released some free COVID insight products during the timeframe to help our customers do that. We released terminology for free, open source terminology for non-IMO customers, so that everybody could be speaking the same language.
You have a couple of challenges. You have the systems being used. You have the terminology that is the base in that system. Then you have how it was implemented. All these complicating factors make it difficult if you can’t pull that data out, normalize it, and then pull insights from the normalized data.
Why is it hard to get a list of COVID-diagnosed or COVID-positive patients?
It’s easy to get a list of diabetic patients. But it’s harder if you are looking for Type 1 diabetic patients with BMIs over a certain level who have retinal problems.It’s more difficult to search disparate data systems. The way that those diagnoses are described continuously changes. It’s not good enough to create a group, or a cohort search, once. You have to constantly maintain and update it so that you are capturing all of the patients that should be in that cohort. That makes it difficult.
Does it take a lot of coordination and discussion to populate research databases using data from many hospitals?
Yes. It generally takes a back-end tool. We are finding that across healthcare now, beyond the hospitals, there’s this large need with data aggregators, top health companies, HIEs, and point-of-care solutions. Anybody who’s pulling from that same data has the same challenges. Each use case is different, but they are all trying to do the same thing. They are pulling from multiple platforms and multiple ways of describing things.
How much progress has been made so that a healthcare startup can get hospital data that is immediately useful, even if only from their own client?
It’s an enormous problem. For a while, people tried to rely on coded data or claims data, which is summarized data. It’s good for the purpose it was summarized for, but it doesn’t work when you get back to the specifics of a group of patients or a patient themselves. A lot of effort is being done across the industry to make this better. Our EHR partners are working on it and we certainly are. We launched a product last year called Normalize that allows an entity to normalize the clinical data and and then pull insight from that data. The way things are described is standardized.
Was it hard to get a historical picture of COVID infection after the fact once code sets were finally updated?
It was difficult, but that’s why we focus so much on letting the physician describe it clearly and specifically. We can go back to the specificity that the physician used in the description to sort through that. But it is much, much more difficult.
That’s why 2020 was an interesting year for us. We generally do four to six terminology releases per year for our customers. We had releases going out every single month because so much was changing with COVID and we needed to get the descriptors in there as quickly as possible. Each time there’s a new learning, we have to get those descriptors in so that the data is a little bit cleaner early on, and you’re not trying to go back for as many months.
What have we learned from the need to get near real-time hospital data for urgent research?
We have learned, especially in a pandemic year, how critical it is to get the right information into the right hands of the right people and make sure the tools they are using can support it quickly, so that you can take care of the patient and create better patient outcomes. That isn’t happening, as you said, in the old traditional ways any more. There’s much more need to create networks of information and ways to disperse that information out to clients as quickly as possible. Not just from a company like IMO, but from many vendors in healthcare IT, who are working side by side with our hospital partners and with physician organizations across the country to make sure the information is shared, is accurate, and is complete and up to date.
How are health systems using value sets?
Value sets are searches that allow you to filter to find a specific cohort or group of patients. Then, to monitor them, reach out to them, and communicate with them.
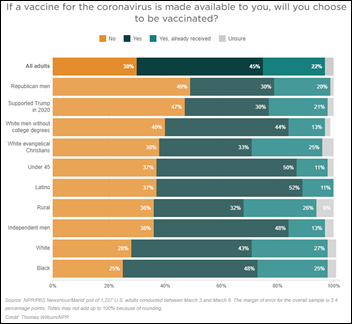
Hospitals are using them in many ways. They are using them proactively to reach out to patients, such as in the vaccine situation, where you are trying to find a specific group of patients. They are also using them after the fact to monitor patients and do post-communication or information sharing.
It becomes critical to create these value sets accurately and to include all of the specific descriptors, not just the code sets. That changes every month, as in COVID, where we were changing descriptors and information and adding new information every month. You have to maintain those and update those to continue to be accurate. It’s not a one-time event. Not just hospitals, but others in the industry are using those as well, to monitor groups of patients or find information on groups of patients at a more specific level than a high-level search, as I described earlier.
Has the need changed from retrieving a set of patients whose characteristics support a research hypothesis to instead hoping that technology, perhaps using AI or other techniques, can take a seemingly diverse group of patients and figure out what risk factors and outcomes they share?
AI and other technology is useful, as long as you maintain the specific information. Searching or using AI on summarized or aggregated data doesn’t work because you have the same problem as if a human was doing it. You can’t find the information. You have to make sure that the specific information is in there and that you are using some common language. Words become important and descriptors become really important so that you can pull from both the structured and unstructured data in the same way.
The biggest challenge, still, is the common language. But as we continue to create tools that can standardize that language and can normalize that data, then there’s an opportunity to start to use more technology to mine the data.
Here’s an unrelated question about your interest in creating opportunities for women in health IT and business in general. I can go to Company X’s leadership page and see rows of white male faces. How would you convince that company that the people they chose for those jobs weren’t optimal?
So much of it is awareness and being intentional. I spend a lot of time talking to different groups about this. I can tell you that first, the leadership has to recognize that diverse teams outperform non-diverse teams. Helping them understand that and showing them proof sources of where that’s really true makes sense. This isn’t an indictment of, “Hey, men can’t do it.” It’s just that men can do it and women can also bring a unique aspect to it. When you are serving something like healthcare, it’s obviously made up of many, many women as part of your decision-making. You are missing out on the unique opportunity to deliver what you need to, to an audience, if you aren’t looking at it from a diverse perspective, which actually goes way beyond men and women. It begins with believing that.
Once you believe that, stop talking about it and turn it into action. Many companies are good at executing, mine included, but if it isn’t a focused goal that you are executing on, then like anything else, it’s just a theoretical, conceptual conversation, and maybe it happens and maybe it doesn’t. Because women are so underrepresented, you have to be intentional about your hiring process, making sure that the candidate pools are diverse, because if the candidate pools don’t start out diverse, it’s difficult to get diverse hiring decisions.
I focus on it being intentional. I was intentional with how I built my team. I was intentional about specifically putting a female in the CFO role because we had a strong cultural belief in the company that men were CFOs and women ran HR. My chief people officer is a man, intentionally, and my CFO is a woman, intentionally. I found incredible candidates just by making sure that the pool of candidates was diverse.
So white men often get these jobs because somebody down in the company pushed them to the forefront as candidates?
That’s right. There’s a larger pool of those candidates. I gets even even more challenging when you race to that mix. We all have a responsibility to reach out to the college age kids and the high school aged kids, because we don’t have enough women. We don’t have enough black or Hispanic students going into majors around STEM, going into focus job opportunities or internships around STEM. You also have to get intentional about helping make a difference to help the candidate pools get better over time. We focus an intern program there to help our candidate pools become richer.
This definitely isn’t about hiring a lesser candidate. Nobody should hire a lesser candidate for the job. You need to hire the right person for the job, but it starts with having diverse pools of candidates to choose from.
Where do you see the company focusing in the next 3-5 years?
We will continue to grow terminology. More and more needs to be added, but we also will begin to focus more on the insight space and on new markets that need that. The way that I look at the ecosystem is that there’s this large pool of clinical data. No matter where you are in the ecosystem, everybody is pulling from that same data. There’s not a different data set somewhere else. There’s different use cases driving the need to get at that data, but there’s a variety of people — some that I described, some in the payer space, some in life sciences — who are all pulling from that same clinical data. I see an expansion for opportunity for IMO to help expand in the terminology space, but also expand who we are helping in the use cases we can provide solutions for, to actually accomplish more from the data.
Do you have any final thoughts?
We are improving in healthcare. As challenging as COVID was for the whole world, it put an exclamation point on where there are holes and where we need to make improvements. There’s a lot of opportunity for healthcare IT technologies to come in and fill some of those gaps. I’m excited about the movement in healthcare and the movement towards patient outcomes and the actual fact that the data can and will support it as we move forward.
Comments Off on HIStalk Interviews Ann Barnes, CEO, Intelligent Medical Objects

































Look, I want to support the author's message, but something is holding me back. Mr. Devarakonda hasn't said anything that…