EPtalk by Dr. Jayne 5/28/20

Memorial Day in the US looked a lot different this year to most of us. I hope people were able to have some thoughtful time about the challenges our nation has faced in the past. Although the National Cemetery Administration didn’t allow “public” groups to place flags in the National Cemeteries as we usually do, I was glad to see that the 3rd US Infantry Regiment was able to take care of Arlington National Cemetery. I found this picture with a great piece featuring quotes and remembrances to honor those who died for our freedom.

It’s nearly impossible to keep up with my inbox lately, so I was glad that the announcement for the ONC Virtual Working Session on Patient Identity and Matching on June 1 caught my eye. Feedback gained from the meeting will inform ONC’s report to Congress. Nearly all of the organizations I work with struggle with patient matching, and the problem frequently leads to patient safety issues (missing data, erroneous data) or excess costs (repeating tests because they’re not in the right chart). Participants are encouraged to discuss their insights into existing challenges and innovations that can help. I’m registered and hope to see you there.
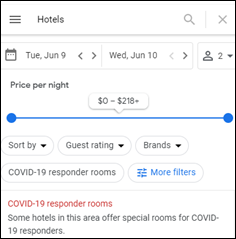
Another inbox item that caught my eye covered Google’s efforts to help COVID-19 responders find hotel rooms. The recently-launched feature allows searches to be filtered for hotels that offer “COVID-19 responder rooms.” I tried a couple of searches to see what the special rooms might include – discounted price, quiet floor, consolidated part of the hotel, etc. – but all of them just said “contact the hotel for details.”
I was dabbling in telemedicine prior to the pandemic, and then things got real very quickly. Patients were scrambling to understand whether they had been exposed and trying to obtain refills from medications they would usually obtain from doctors whose offices were suddenly closed.
As offices reopen in my area, volumes are trending back to the baseline. I chuckled when I saw the headline of this op-ed piece, “Telemedicine Tales: Let’s Reschedule When You’re Not Shopping.” Especially when wait times were long, it wasn’t unheard of for calls to connect when patients were somewhere other than at home, but fortunately I didn’t encounter some of the situations described by the author, including the “telephone encounter plus scalp exam” that resulted when a patient couldn’t resolve a camera angle issue. I completely agree with his assertion that he is “looking forward to the time when patients and doctors can determine whether in-person, video, or telephone visits best meet their mutual needs rather than having this dictated by public health emergencies or inflexible payment rules.”
Physicians in my area are sharply divided on whether telemedicine is going to be the wave of the future or the proverbial flash in the pan. There are some significant data points coming out of institutions like NYU Langone Health, which recently published in the Journal of the American Medical Informatics Association. They saw 683% growth in virtual urgent care visits and 4,345% growth in non-urgent virtual visits between March 2 and April 14. Most of my physician friends have enjoyed being able to see their patients virtually and be paid, especially when performing services that were previously uncompensated under traditional fee-for-service reimbursement models.
Those owning their own practices were happy with the flexibility, but employed physicians were a little less thrilled, depending on the arrangements. One large health system made the physicians physically come to the office to perform telehealth services, stating that it is required by HIPAA.
Speaking of large health system response to COVID-19, we’re not out of the woods yet for PPE. At my workplace, each employee has been issued four masks that they are expected to rotate on a daily basis and can only replace masks when the straps break or when they are visibly soiled. Apparently Missouri-based Mercy isn’t doing quite so well, with workers reporting that they’re wearing the same masks three shifts in a row. Competing health systems in the region are sterilizing masks daily. Most of the physicians I know still report a critical shortage of PPE and many are wearing non-medical respirators, such as those used for woodworking. Now that businesses are reopening and even more people need masks, the problem is worsening for some types of PPE, including surgical masks and gloves.
A recent Perspective piece in JAMA Internal Medicine describes some of the tensions found in expanding hospital volumes. It looks at the difference between making the hospital safe and making it feel safe, which aren’t always the same thing. I’ve experienced this in my own practice. Patients who acted shocked when I was masked during flu season and asked if I was afraid of catching their cold have become patients who file a complaint if they see a staffer removing their mask to grab a quick drink of water.
The author describes a new world where services that were previously in demand are no longer in demand and the importance of creating an appearance of safety. He notes the fine line between how new routines and procedures are presented, and whether they create an appearance of safety or danger that might cause hospitals to “inadvertently scare away the patients who need them.”
He closes by noting the difference between his weekend errand-running and life in the hospital with its critical care tasks. These are the skewed realities that many of us are living with every day, when we go from 12 hours of hazmat duty to hearing people complain about masks at the supermarket. Some days it’s surreal.
I see a lot of masks and gloves on the ground at retail locations, and at the same time, my office is limiting workers to one surgical mask per shift if they elect to not wear one of the four provided N95s. It’s a jarring visual and I certainly understand why many healthcare workers are seeking care for anxiety and acute stress reactions. This may be our new normal, but it doesn’t quite feel routine just yet.
The bottom line is that healthcare is still in crisis mode, but it feels like the rest of the world has moved on, especially when you see the videos of debauchery at some of the country’s lakes and beaches.
Is there anyone who is not operating under crisis standards of care? Leave a comment or email me.
Email Dr. Jayne.



Hard agree, and not just because I'm a spreadsheet nerd. Why are we all here? Isn't it in the service…